|
 
 |
| CASE REPORT |
|
| Year : 2014 | Volume
: 2
| Issue : 2 | Page : 62-64 |
|
Central nervous system toxoplasmosis in human immunodeficiency virus infection: Imaging findings
Adenike Temitayo Adeniji-Sofoluwe
Department of Radiology, College of Medicine, University College Hospital, University of Ibadan, Ibadan, Nigeria
| Date of Acceptance | 12-Jun-2015 |
| Date of Web Publication | 3-Jul-2015 |
Correspondence Address:
Adenike Temitayo Adeniji-Sofoluwe
Department of Radiology, College of Medicine, University College Hospital, University of Ibadan, Ibadan
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157.159972

Toxoplasmosis is one of the most common zoonoses worldwide caused by Toxoplasma gondii. Majority of T. gondii infections are asymptomatic or induce transitory and mild symptoms characterized by lymphadenopathy. Risk factors are immunosuppression and pregnancy. Human immunodeficiency virus (HIV) infected persons represent the group at highest risk of developing symptomatic toxoplasmosis especially with a CD4 count of <100, which can be fatal. A middle-aged acute-on-chronic ill-looking, conscious, lethargic but confused, pale man with lymphadenopathy involving the cervical, sub-mental and axillary nodes, and widespread fungal infections is presented. Neurologic imaging is frequently used in the diagnosis of central nervous system (CNS) toxoplasmosis in combination with serology and clinical assessment. Computed tomography scans show multiple, bilateral, contrast-enhancing ("ring enhancing"), focal brain lesions in 70-80% of patients with CNS toxoplasmosis. The course of disease can frequently be fatal if not recognized and treated early as was the case in this patient. Keywords: Central nervous system, computed tomography, human immunodeficiency virus, toxoplasmosis
How to cite this article:
Adeniji-Sofoluwe AT. Central nervous system toxoplasmosis in human immunodeficiency virus infection: Imaging findings. J HIV Hum Reprod 2014;2:62-4 |
How to cite this URL:
Adeniji-Sofoluwe AT. Central nervous system toxoplasmosis in human immunodeficiency virus infection: Imaging findings. J HIV Hum Reprod [serial online] 2014 [cited 2018 Feb 14];2:62-4. Available from: http://www.j-hhr.org/text.asp?2014/2/2/62/159972 |
| Introduction | |  |
Toxoplasmosis is one of the most common zoonoses worldwide caused by Toxoplasma gondii a worldwide facultatively heterogeneous parasite with intermediate hosts that are probably all warm-blooded animals and definitive hosts, which are members of the family Felidae. [1] There are three infectious stages in the life cycle of T. gondii; the tachyzoites, bradyzoites, and sporozoites, which may be acquired via ingestion or by transplacental passage of tachyzoites. [1],[2]
Less common modes of transmission include blood transfusions and organ transplants. [2]
| Case report | |  |
S. O was a 56-year-old married Nigerian diplomat, who presented with cough of 4 weeks, difficulty with breathing of 3 weeks, intermittent and high grade fever of 2 weeks, and altered sensorium with irrational talks for 5 days duration. The cough was productive of yellowish sputum, worse at night, but there was no hemoptysis. He had been treated for chronic cough and toxoplasmosis in 2004 in Greece. He was not a known hypertensive or diabetic. As a diplomat who worked with the Federal Ministry of Foreign Affairs, he had worked in Greece and the United States of America. He divorced his first wife 13 years prior to presentation and remarried 4 years later. No history of owning cats/previous human immunodeficiency virus (HIV) screening, sexually transmitted disease or sexual history was obtainable.
On examination, he was an acute-on-chronic ill-looking man, pale, acyanotic, febrile, with ankle edema, and lymphadenopathy involving the cervical, sub-mental, and axillary nodes. Widespread fungal infections of the face and trunk were seen, and these lesions appeared well-circumscribed papular, circular, and scaly. The chest was barrel shaped, with reduced breath sounds globally. Basal crepitations were also heard. The abdomen and cardiovascular system showed no abnormality. He was conscious and lethargic, confused, but responded to calls and was aphasic. Muscle tone and reflexes were also normal. Electrolyte, urea, and creatinine were normal. HIV screening was positive and was confirmed by polymerase chain reaction. Enhanced cranial computed tomography (CT) was done, [Figure 1] the serial axial images showed an area of extensive hypodensity that was centrally located at the level of the basal ganglia extending marginally on either side. There was also an anterior extension of the hypodensity with resultant compression of the anterior horns of both lateral ventricles and the third ventricle. The contrast images showed ring enhancement of the hypodense lesions. In view of the location, marked surrounding edema, and typical enhancement pattern, a radiological diagnosis of toxoplasmosis was made with lymphoma as a differential. Based on the clinical and radiological findings, the HIV disease was staged at IV acquired immunodeficiency syndrome (AIDS) according to World Health Organization (WHO) staging criteria. He was treated empirically with antimicrobial broad spectrum therapy; he deteriorated and died 4 weeks after admission despite treatment. The use of highly active antiretroviral therapy could also have made a difference but was not available at the time. Furthermore, prophylaxis against T. gondii infections with trimethoprim-sulfamethoxazole, which is effective against toxoplasmosis, was not common practice.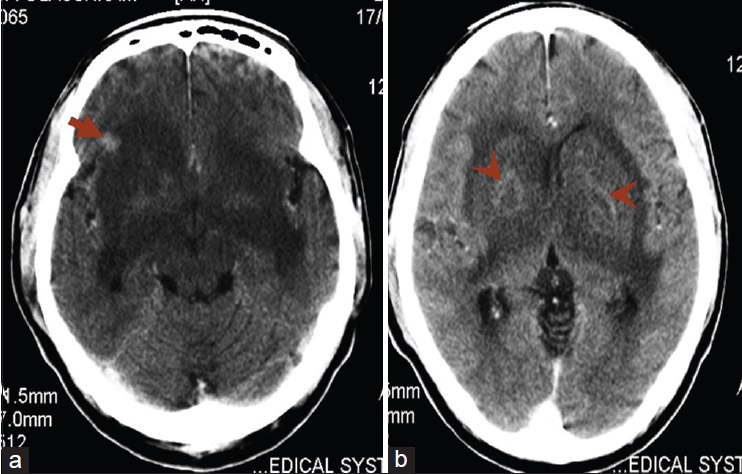 | Figure 1: Axial contrast enhanced computed tomography of the brain: (a) An area of extensive hypodensity in the region of the basal ganglia bilaterally with compression of the third ventricle and a focus of enhancing hypodensity in right frontal lobe (arrow), (b) anterior extension of the hypodensity with resultant compression of the anterior horns of both lateral ventricle with ring enhancement within the hypodensity in the basal ganglia (arrowheads)
Click here to view |
| Discussion | |  |
Toxoplasma gondii is a single-celled parasite with a worldwide distribution. [3] The risk of acquiring T. gondii infection varies by geographic location and population group. The rate of seroprevalence can be as high as 90% in Western Europe possibly due to consumption of raw or undercooked meats (especially pork, lamb, and venison), and in some tropical countries from eating uncooked foods that have come in contact with infected meat or the accidental ingestion of contaminated soil containing cat feces. [4] Among animals reared for food, T. gondii is frequently isolated in pigs, sheep, and goats. The main source of infection is an oocyst shed by a cat or a tissue cyst in intermediate hosts. [3],[5]
Risk factors are immunosuppression and pregnancy. HIV-infected persons represent the group at highest risk of developing symptomatic toxoplasmosis especially with a CD4 count of <100, which can be fatal. It can occur as a new infection or a reactivation of latent infection because the drugs routinely used are effective against the proliferative stages, but they are ineffective in eradicating the encysted form of parasite. [3],[4]
Majority of T. gondii infections are asymptomatic or induce transitory and mild symptoms characterized by lymphadenopathy. [1] The most common site of reactivation is the central nervous system (CNS). Toxoplasmosis is the most common CNS opportunistic infection in AIDS patients. [4] It has been observed that the development of encephalitis due to T. gondii infection can occur in up to 40% of HIV-infected patients. [3] In immunocompromised patients, in contrast to immunocompetent patients, the course of disease can frequently be fatal if not recognized and treated early. [5]
In HIV-infected patients with encephalitis, they may present with cranial nerve abnormalities, visual defects, movement disorders, stroke, personality changes, and other neuropsychiatric abnormalities. [6] Previous studies have documented that the most common clinical manifestation of toxoplasmic encephalitis (TE) in HIV patients is headache (56%). CT scans findings showing multiple (96.4%), hypodense (66.7%) lesions, and in the parietal region (39.3%). [7] Compared with this patient, the CT findings are in concordance except for the site, which was predominantly in the basal ganglia. A CD4 count of <100 cells/microliter is also significantly associated with the development of TE. [6],[7] Chest abnormalities may also be present.
Neurologic imaging is frequently used in the diagnosis of CNS toxoplasmosis in combination with serology and clinical assessment. CT scans show multiple, bilateral, contrast-enhancing ("ring enhancing"), focal brain lesions in 70-80% of patients with CNS toxoplasmosis. [7],[8] Magnetic resonance imaging (MRI) is more sensitive than CT scan and may be particularly useful in patients without focal neurologic abnormalities and in those with one or no lesions detectable on CT scan. Occasionally, a single brain lesion on MRI may be found but such a finding suggests an alternative diagnosis like primary CNS lymphoma. However, findings on CT or MRI scans are not pathognomonic for toxoplasmosis. [8]
The definitive diagnosis of infection requires detection of the parasite or T. gondii DNA in body fluids or tissue biopsies and in practice, this may be difficult to get. Therefore, serologic studies by assaying immunoglobulin M antibody and immunoglobulin G titers are used. [3],[8]
Primary prophylaxis against toxoplasmosis is recommended in HIV-infected, toxoplasma seropositive (antibody positive) adults, and adolescents (including pregnant women) who have CD4 T-cell counts of <100 cells/μL regardless of their clinical status and in symptomatic (WHO stage 2, 3, and 4) and in HIV-positive patients who have CD4 T-cell counts of <200 cells/μL. [9],[10] The most common drugs used to treat toxoplasmosis are pyrimethamine and sulfadiazine, used in combination.
| References | |  |
| 1. | Dubey JP, Beattie CP, editors. Toxoplasmosis of Animals and Man. 2 nd ed. Boca Raton, FL, USA: CRC Press; 1988.  |
| 2. | Minkoff H, Remington JS, Holman S, Ramirez R, Goodwin S, Landesman S. Vertical transmission of toxoplasma by human immunodeficiency virus-infected women. Am J Obstet Gynecol 1997;176:555-9.  |
| 3. | Montoya JG, Remington JS. Toxoplasma gondii. In: Mandell G, Dolin A, Bennett J, editors. Principles and Practice of Infectious Diseases. Philadelphia: Churchill Livingston; 2000. p. 2858-88.  |
| 4. | Porter SB, Sande MA. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med 1992;327:1643-8.  |
| 5. | Wallace MR, Rossetti RJ, Olson PE. Cats and toxoplasmosis risk in HIV-infected adults. JAMA 1993;269:76-7.  |
| 6. | Renold C, Sugar A, Chave JP, Perrin L, Delavelle J, Pizzolato G, et al. Toxoplasma encephalitis in patients with the acquired immunodeficiency syndrome. Medicine (Baltimore) 1992;71:224-39.  |
| 7. | Post MJ, Kursunoglu SJ, Hensley GT, Chan JC, Moskowitz LB, Hoffman TA. Cranial CT in acquired immunodeficiency syndrome: Spectrum of diseases and optimal contrast enhancement technique. AJR Am J Roentgenol 1985;145:929-40.  |
| 8. | Nissapatorn V, Lee C, Quek KF, Leong CL, Mahmud R, Abdullah KA. Toxoplasmosis in HIV/AIDS patients: A current situation. Jpn J Infect Dis 2004;57:160-5.  |
| 9. | Low incidence of congenital toxoplasmosis in children born to women infected with human immunodeficiency virus. European Collaborative Study and Research Network on Congenital Toxoplasmosis. Eur J Obstet Gynecol Reprod Biol 1996;68:93-6.  |
| 10. | Liu AY, Kittredge PV, Vittinghoff E, Raymond HF, Ahrens K, Matheson T, et al. Limited knowledge and use of HIV post- and pre-exposure prophylaxis among gay and bisexual men. J Acquir Immune Defic Syndr 2008;47:241-7.  |
[Figure 1]
|