|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2013 | Volume
: 1
| Issue : 1 | Page : 22-26 |
|
Effects of maxillary expansion rate on the nasopharyngeal airway in the mixed dentition
Faruk Izzet Uçar1, Sabri Ilhan Ramoglu2, Mehmet Ali Öztürk3, Zafer Sari4
1 Private Practice, Kayseri, Department of Orthodontics, Bezmi Alem Vakif University, Istanbul, Turkey
2 Associate Professor, Department of Orthodontics, Bezmi Alem Vakif University, Istanbul, Turkey
3 Research Asistant, Department of Orthodontics, Katip Celebi University, Izmir, Turkey
4 Dean and Profesor, Department of Orthodontics, Akdeniz University, Antalya, Turkey
| Date of Web Publication | 18-May-2013 |
Correspondence Address:
Faruk Izzet Uçar
30 Agustos Mah. No: 5/36 38039, Kayseri
Turkey
 Source of Support: None, Conflict of Interest: None  | Check |
 
Objective: To evaluate the effects of maxillary expansion rate on nasopharyngeal airway in the mixed dentition period. Materials and Methods: Three groups of the patients were individually treated with semi-rapid maxillary expansion (SRME), rapid maxillary expansion (RME), and removable appliance without expansion (control group). Mean age values were 8.63 1.09 years for the SRME group (18 patients: 11 girls and 7 boys), 8.78 1.21 years for the RME group (17 patients: 11 girls and 6 boys), and 10.5 1.01 years for the control group (16 patients: 6 girls and 10 boys). Screw activation was conducted two-quarter turns per day during the treatment in RME group. Same activation order was used for SRME group for the first week, followed by one-quarter turn every 2 days. Intragroup comparisons were evaluated by paired samples t-test and intergroup changes were analyzed with an analysis of variance (ANOVA). Post-hoc multiple comparisons were done by Tukey's Honestly Significance Difference (HSD) test. Results: For both SRME and RME groups, changes in aerial and total airway measurements were statistically significant when compared to the control group (SRME vs. control: P = 0.049 in aerial, P = 0.038 total airway; RME vs. control: P = 0.048 in aerial, P = 0.011 total airway). When both treatment groups were compared, no statistically significant differences were found in any of the measurements. Conclusions: SRME and RME had significant effects on craniofacial airway dimensions when compared to initial values or untreated control values. Changes in airway dimension were similar in the SRME and RME groups. Keywords: Airway measurements, expansion rate, mixed dentition
How to cite this article:
Uçar FI, Ramoglu SI, Öztürk MA, Sari Z. Effects of maxillary expansion rate on the nasopharyngeal airway in the mixed dentition. J Orthod Res 2013;1:22-6 |
How to cite this URL:
Uçar FI, Ramoglu SI, Öztürk MA, Sari Z. Effects of maxillary expansion rate on the nasopharyngeal airway in the mixed dentition. J Orthod Res [serial online] 2013 [cited 2017 Apr 14];1:22-6. Available from: http://www.jorthodr.org/text.asp?2013/1/1/22/112251 |
| Introduction | |  |
Maxillary transverse deficiency, which is one of the most common skeletal problems in craniofacial region [1] associated with functional, esthetic, and occlusal problems including dental crossbites, [2] reduces nasal permeability owing to nasal stenosis and enlargement of nasal turbinates causing a decrease in nasal airway size. [3] The nasopharyngeal airway (NA) is a cone-shaped tube that contains muscles and mucosa. It also includes an adenoidal lymphatic tissue located in the posterior area.
Rapid maxillary expansion (RME) has been used as a routine clinical procedure in orthodontics, with its main purpose to expand the maxilla in young patients who had transverse maxillary deficiency accompanying posterior crossbite and crowding. [1],[2] The expansion screw is periodically activated every day, and the resulting force (0.9-4.5 kg) causes midpalatal suture to open and the maxillary bones to separate from each other. [4] Zimring and Isaacson [5] showed that the residual load exists with the activation of the appliance twice a day. In addition to the expansion force at the intermaxillary suture, high forces are generated in different parts of the craniofacial complex. [6] It was reported that slower expansion causes less tissue resistance in the nasomaxillary complex but more stable results. [7],[8]
According to the frequency of the activations and type of appliance, different expansion protocols were used in the literature. [9],[10] Iseri and Özsoy[8] reduced the rate of expansion to slow maxillary expansion immediately after the separation of the intermaxillary suture by RME and named this protocol as semi-rapid maxillary expansion (SRME) which was different from the SRME protocol firstly described by Mew. [11]
Ramoglu and Sari [12] treated their patients in mixed dentition using both RME and SRME protocols and reported that RME caused more inferior movement of posterior nasal spine (PNS) which is one of the common points used in NA measurements. For these purposes, the null hypothesis assumed that no significant differences were present in the NA dimensions in mixed dentition subjects treated by SRME and RME.
| Materials and Methods | |  |
The study comprised three groups: SRME, RME, and control. The SRME group included 17 patients (11 girls and 6 boys), whereas the RME group consisted of 18 patients (11 girls and 7 boys) who underwent treatment in the Department of Orthodontics of Selcuk University. The control group consisted of 16 patients (6 girls, 10 boys) who underwent treatment in the Department of Orthodontics of Erciyes University. The mean age values for SRME, RME, and control groups were 8.63 ± 1.09, 8.78 ± 1.21, and 10.5 ± 1.01 years, respectively. The inclusion criteria for maxillary expansion groups were existing functional unilateral or bilateral posterior crossbite depending on transverse deficiency and any sagittal skeletal problem. All parents signed an informative consent form.
Appliance and activation
A splint-type tooth-and-tissue-borne modified bonded RME appliance was used. [12],[13],[14],[15],[16] The activation was applied two-quarter turns per day for the first week, followed by one-quarter turn every 2 days in SRME group. The mean treatment time was 57.16 ± 21.52 days. In the RME group, the activation was applied two-quarter turns per day and the mean treatment time was 21.23 ± 8.36 days. Opening of midpalatal suture was monitored at the end of first week on occlusal radiographs. The screw was fixed by a ligature wire, and the same appliance was worn as fixed retainer for 14 days and was debonded after that period. A removable appliance, which was fabricated at the same appointment, was placed as retention appliance.
The control group was selected from the archive that had no sagittal or transverse deficiency and underwent removable appliance therapy for one or two anterior crossbite. The mean time of pre- and post-treatment records was 227.8 ± 58.12 days.
Records and measurements
The teeth were in centric occlusion, and the lips were lightly closed. Handlman and Osborne's method [17] was used for evaluating total, adenoidal, and aerial areas on the lateral cephalometric radiographs by one author (MAO). Reference line of this method were palatal plane (ANS-PNS), basion (Ba)-nasion (Na) plane, and two perpendicular lines to the palatal plane: one crosses the PNS while the other one crosses the anterior point of Atlas More Details vertebra. The resulting trapezoid was geometrically divided into two (aerial and adenoid) spaces. The sum of aerial and adenoidal areas was recorded as the total area [Figure 1].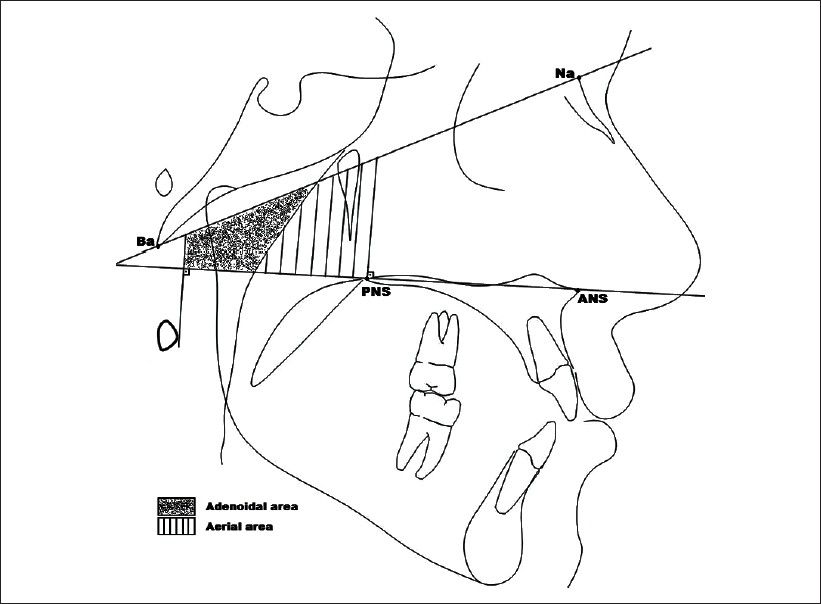 | Figure 1: Basion (Ba)– nasion (Na) plane, palatal plane (ANS-PNS), and two perpendicular lines to the palatal plane: one crosses the anterior point at atlas vertebra and the other one crosses the PNS were used
to determine nasopharyngeal areas; adenoidal area, aerial area, and total area; the sum of adenoidal and aerial areas
Click here to view |
Statistical analysis
All statistical analyses were performed by using the Statistical Package for Social Sciences (SPSS), version 13.0 for Windows (SPSS Inc., Chicago, IL, USA). The normality test of Shapiro-Wilk and Levene's variance homogeneity test were used regarding the data. Data were normally distributed, and homogeneity of variance was seen between the groups. Paired sample t-test was used for intragroup comparisons, and analyses of variance (ANOVAs) were used to analyze intergroup changes. Post-hoc multiple comparisons were evaluated by Tukey's Honestly Significance Difference (HSD) test. The statistical test was defined significant when P -value was lesser than 0.05. Ten radiographs were selected randomly and retraced 8 weeks after the first measurement by the same author to determine the possible errors associated with radiographic measurements. A Bland and Altman plot was used to assess the repeatability. No significant difference was found between the first and second measurements.
| Results | |  |
For statistical comparison of pre-treatment values of SRME and RME groups, the treatment groups were equally matched, but the control group had larger aerial and adenoidal area [Table 1].
In the SRME group, statistically significant changes were found in aerial area (P = 0.006) and total area (P = 0.009) measurements of airway after the treatment period. In the RME group, post-treatment measurements showed significant differences in aerial area (P = 0.008) and total area (P = 0.007) of airway measurements. In the control group, no statistically significant change was found in the measurements [Table 2].
Following the expansion in both groups, the changes in aerial and total airway measurements were statistically significant when compared to the control group (SRME vs. control: P = 0.049 in aerial, P = 0.038 total airway; RME vs. control: P = 0.048 in aerial, P = 0.011 total airway). No statistically significant differences were found when both treatment groups were compared [Table 3].
| Discussion | |  |
An interaction occurs between respiratory function and the maxillary [18] and mandibular growth pattern. [19] A significant relationship exists between airway space and facial morphology; [20] also, airway space may be affected by conditions such as functional anterior shifting, [21] sagittal [22] and vertical skeletal relation. [23] For these reasons, subjects who had no sagittal skeletal problems were selected in this study.
Lopatienλ and Babarska[24] reported tendency of higher nasal resistance in patients with posterior crossbite. There was no statistically significant difference between SRME and RME groups when the pre-treatment measurements were compared; however, aerial area was statistically greater in the control group. This might be due to maxillary transverse discrepancy in the treatment groups. The aim of this study was to compare the aerial, total, and adenoidal differences between the treatment and control groups. When SRME-control and RME-control groups were evaluated, it has been found that aerial and total area values were statistically increased in the treatment groups, but adenoidal areal value did not change.
An important limitation of the present cephalometric study was the use of a two-dimensional technique that does not represent exactly the NA space, which would have required a more complex three-dimensional cone-beam computed tomography (CBCT) and dynamic estimation. [25] Lateral cephalometric radiographs have been used for examining dentofacial structures, nasal airway, and related areas. [26],[27] Malkoc et al. [28] stated that cephalometric films are significantly reliable and reproducible in determining the airway dimensions. When computed tomography, magnetic resonance imaging (MRI), and cephalometric films were compared, there was a significant positive relationship between NA size on the cephalometric films and its true volumetric size as determined from CBCT or MRI scan in adolescents. [29],[30] This study was performed with two-dimensional cephalometric films to evaluate only the pharyngeal airway area, not the airway flow capacity.
Another limitation of this study was the obligation to select the control group to distinguish the normal growth effects from the treatment effects, while the expansion treatment time was too low to be affected by growth. For ethical reasons, no data can be collected from untreated patients who have constricted maxilla. Because of this limitation, the records of patients who underwent removable appliance therapy and have had pre- and post-treatment lateral cephalometric radiographs were collected from the archive. The control group patients' post-treatment records were taken 277.8 ± 58.12 days after their initial visit, which is almost 5 times longer than that of SRME group (57.16 ± 21.52 days) and almost 12 times longer than that of RME group (21.23 ± 8.36 days). However, the pre-post record interval is longer, whereas no statistically difference was observed in the control group.
A splint-type tooth-and-tissue-borne modified bonded RME, full-coverage acrylic appliance has been used in order to prevent tipping and extrusion of the maxillary posterior teeth, [31] occlusal intercuspation, [32] and control the vertical effects of expansion. [33],[34]
Expansion of the maxilla is a universal treatment protocol for constricted maxilla and arch length discrepancies. The concept of RME and SRME has been expanded to the nasal cavity and facial structures, as previous studies have suggested that expansion facilitates the breathing and an increase in nasal width and volume. [26],[27],[35],[36],[37],[38],[39],[40] Sökücü et al. [41] evaluated and compared the effects of RME and fan-type RME on nasal airway dimensions by using acoustic rhinomanometry, and reported that the dimensions improved after the RME. Many authors clearly explained that nasal airway resistance significantly decreased after RME. [27],[39],[42],[43] In this study, aerial area enlarged by RME. These findings are also supported by clinical studies about the effects on cross-sectional area [44] and nasal volume measurements. [27],[45] In previous studies; enlarged lower nasal width [8] and small, but statistically significant forward movement of the upper facial skeleton, and small increase in face height [40] were reported with SRME protocol. Ramoglu and Sari [12] evaluated and compared SRME and RME in mixed dentition patients and implied that both protocols resulted in increased nasal cavity width and inferior movement of PNS which was significantly greater for RME. However, PNS point is one of the points determining nasal, adenoidal, and total areas, and no significant difference was found in the NA between the SRME and RME groups in this study.
The present study did not evaluate the nasal cavity, but evaluated the NA. The effects of SRME and RME on airway dimensions in mixed dentition patients were evaluated in the present retrospective cephalometric study. Both SRME and RME increased total and aerial airway dimensions significantly, but no significant effects were observed in adenoidal area, when compared with the control group. But no difference was found in the amount of this enlargement between these methods. According to the present findings, the null hypothesis was rejected in this manner.
| Conclusion | |  |
Within the limitations of this study, the findings suggest that SRME and RME had both similar and significant effects on craniofacial airway dimensions.
| References | |  |
| 1. | McNamara JA. Maxillary transverse deficiency. Am J Orthod Dentofacial Orthop. 2000;117:567-70. 
|
| 2. | Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the mid-palatal suture. Angle Orthod 1961;31:73-90. 
|
| 3. | Lessa FCR, Enoki C, Feres MFN, Valera FCP, Lima WTA, Matsumoto MAN. Breathing mode influence in craniofacial development. Braz J Otorhinolaryngol 2005;71:156-60. 
|
| 4. | Bishara SE, Staley RN. Maxillary expansion: clinical implications. Am J Orthod Dentofacial Orthop 1987;91:3-14. 
|
| 5. | Zimring JF, Isaacson RJ. Forces produced by rapid maxillary expansion. III. Forces present during retention. Angle Orthod 1965;35:178-86. 
|
| 6. | Iseri H, Tekkaya AE, Oztan O, Bilgic S. Biomechanical effects of rapid maxillary expansion on the craniofacial skeleton, studied by the finite element method. Eur J Orthod 1998;20:347-56. 
|
| 7. | Memikoglu TU, Iseri H. Effects of a bonded rapid maxillary expansion appliance during orthodontic treatment. Angle Orthod 1999;69:251-6. 
|
| 8. | Iseri H, Ozsoy S. Semirapid maxillary expansion: a study of long term transverse effects in older adolescents and adults. Angle Orthod 2004;74:71-8. 
|
| 9. | Sandikçioglu M, Hazar S. Skeletal and dental changes after maxillary expansion in the mixed dentition. Am J Orthod Dentofacial Orthop 1997:111:321-7. 
|
| 10. | Usumez M, Uzel I. Evaluation of rapid maxillary expansion and quad-helix in the late mixed dentition period. Turkish J Orthod 2008;21:187-95. 
|
| 11. | Mew JR. Semi-rapid maxillary expansion. Br Dent J 1977;143:301-6. 
|
| 12. | Ramoglu SI, Sari Z. Maxillary expansion in the mixed dentition: rapid or semi-rapid? Eur J Orthod 2010;32:11-8. 
|
| 13. | Orhan M. High-angle özellikli bireylerde rapid maksiller ekspansiyonun etkileri, Master Thesis, Konya: 1999. 
|
| 14. | Basciftci FA, Karaman AI. Effects of a modified acrylic bonded rapid maxillary expansion appliance and vertical chin cap on dentofacial structures. Angle Orthod 2002;72:61-71. 
|
| 15. | Orhan M, Usumez S, Malkoc S. Modified bonded rapid maxillary expansion appliance. World J Orthod 2003;4:119-25. 
|
| 16. | Sari Z, Uysal T, Usumez S, Basciftci F. Rapid maxillary expansion. Is it better in the mixed or in the permanent dentition? Angle Orthod 2003;73:654-61. 
|
| 17. | Handelman CS, Osborne G. Growth of the nasopharynx and adenoid development from one to eighteen years. Angle Orthod 1976;46:243-59. 
|
| 18. | Gungor AY, Turkkahraman H. Effects of airway problems on maxillary growth: a review. Eur J Dent 2009;3:250-4. 
|
| 19. | Jena AK, Singh SP, Utreja AK. Sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage. Angle Orthod 2010;80:1061-7. 
|
| 20. | Jung HL, Cha KS, Chung DH. A study on the correlation between airway space and facial morphology in Class III malocclusion children with nasal obstruction. Korean J Orthod 2007;37:192-203. 
|
| 21. | Ucar FI, Kurt G, Ekizer A, Ramoglu SI. Effects of functional anterior shifting on skeletal and airway structures. Turkish J Orthod 2009;22:218-27. 
|
| 22. | Zhong Z, Tang Z, Gao X, Zeng XL. A comparison study of upper airway among different skeletal craniofacial patterns in nonsnoring Chinese children. Angle Orthod 2007;80:267-74. 
|
| 23. | Ucar FI, Uysal T. Orofacial airway dimensions in subjects with Class I malocclusion and different growth patterns. Angle Orthod 2011;3:460-8. 
|
| 24. | Lopatiene K, Babarska A. Malocclusion and upper airway obstruction. Medicina 2002;38:277-83. 
|
| 25. | Vig KW. Nasal obstruction and facial growth: the strength of evidence for clinical assumptions. Am J Orthod Dentofacial Orthop 1998;113:603-11. 
|
| 26. | Basciftci FA, Mutlu N, Karaman AI, Malkoc S, Kuçukkolbasý H. Does the timing and method of rapid maxillary expansion have an effect on the changes in nasal dimension. Angle Orthod 2002;72:118-23. 
|
| 27. | Doruk C, Sokucu O, Biçakçi AA, Yilmaz U, Tas F. Comparison of nasal volume changes during rapid maxillary expansion using acoustic rhinometry and computed tomography. Eur J Orthod 2007;29:251-5. 
|
| 28. | Malkoc S, Usumez S, Nur M, Donaghy CE. Reproducibility of airway dimensions and tongue and hyoid positions on lateral cephalograms. Am J Orthod Dentofacial Orthop 2005;128:513-6. 
|
| 29. | Aboudara C, Nielsen IB, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2009;135:468-79. 
|
| 30. | Pirilä-Parkkinen K, Löppönen H, Nieminen P, Tolonen U, Pääkkö E, Pirttiniemi P. Validity of upper airway assessment in children: a clinical, cephalometric, and MRI study. Angle Orthod 2011;81:433-9. 
|
| 31. | Memikoglu UT, Iseri H, Uysal ME. Comparison of dentofacial changes with rigid acrylic bonded and Haas type banded rapid maxillary expansion devices. Turkish J Orthod 1997;10:255-64. 
|
| 32. | Alpern MC, Yurosko JJ. Rapid palatal expansion in adults with and without surgery. Angle Orthod 1987;57:245-63. 
|
| 33. | Reed N, Ghosh J, Nanda RS. Comparison of treatment outcomes with banded and bonded RPE appliances. Am J Orthod Dentofacial Orthop 1999;116:31-40. 
|
| 34. | Wendling LK, McNamara JA, Franchi L, Baccetti T. A prospective study of the short-term treatment effects of the acrylic-splint rapid maxillary expander combined with the lower Schwarz appliance. Angle Orthod 2005;75:7-14. 
|
| 35. | Wertz RA, Dreskin M. Midpalatal suture opening: a normative study. Am J Orthod 1977;71:367-81. 
|
| 36. | Ceylan I, Oktay H, Demirci M The effect of rapid maxillary expansion on conductive hearing loss. Angle Orthod 1996;66:301-7. 
|
| 37. | Akkaya S, Gülsen A, Taner-Sarisory L, Balos B. Evaluation of the effects of maxillary expansion on the nasopharyngeal area. World J Orthod 2002;3:211-6. 
|
| 38. | Kilic N, Oktay H, Selimoðlu E, Erdem A. Effects of semirapid maxillary expansion on conductive hearing loss. Am J Orthod Dentofacial Orthop 2008;133:846-851. 
|
| 39. | Doruk C, Bicakci AA, Basciftci FA, Agar U, Babacan H. A comparison of the effects of rapid maxillary expansion and fan-type rapid maxillary expansion on dentofacial structures. Angle Orthod 2008;74:184-94. 
|
| 40. | Kiliç N, Oktay H. Effects of rapid-slow maxillary expansion on the dentofacial structures. Aust Orthod J 2010;26:178-83. 
|
| 41. | Sökücü O, Doruk C, Uysal OI. Comparison of the effects of RME and fan-type RME on nasal airway by using acoustic rhinometry. Angle Orthod 2010;80:870-5. 
|
| 42. | White BC, Woodside DG, Cole P. The effect of rapid maxillary expansion on nasal airway resistance. J Otolaryngol 1989;18:137-43. 
|
| 43. | Timms DJ. The effect of rapid maxillary expansion on nasal airway resistance. Br J Orthod 1986;13:221-8. 
|
| 44. | Bicakci AA, Agar U, Sokucu O, Babacan H, Doruk C. Nasal airway changes due to rapid maxillary expansion timing. Angle Orthod. 2005;75:1-6. 
|
| 45. | Babacan H, Sokucu O, Doruk C, Ay S. Rapid maxillary expansion and surgically assisted rapid maxillary expansion effects on nasal volume. Angle Orthod 2006;76:66-71. 
|
[Figure 1]
[Table 1], [Table 2], [Table 3]
|