|
 
 |
| CASE REPORT |
|
| Year : 2014 | Volume
: 2
| Issue : 1 | Page : 50-53 |
|
Maxillary advancement with rigid external distractor device and mandibular setback in a severe Class III adult patient
Erdem Ayyildiz, Ibrahim Erhan Gelgor
Department of Orthodontics, Faculty of Dentistry, Kirikkale University, Kurtulus Mahallesi, Kirikkale, Turkey
| Date of Web Publication | 29-Jan-2014 |
Correspondence Address:
Erdem Ayyildiz
Department of Orthodontics, Faculty of Dentistry, Kirikkale University, Kurtulus Mahallesi, Kirikkale
Turkey
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-3825.125933

Class III skeletal malocclusion, which is one of the most complainable anomaly by patients can be the result of mandibular prognathism and/or maxillary deficiency. With the advancements in surgical techniques and knowledge, today bimaxillary surgical procedures are frequently used to correct this anomaly so that only mandibular set back operations had been performed in the past. Distraction osteogenesis or callus distraction, which is a process of bone regeneration between the surfaces of vascularized bone segments separated by gradual distraction is a method of bone generation without using bone or soft-tissue grafts. The purpose of this report is to present the orthodontic-orthognathic treatment of a patient with severe Class III skeletal malocclusion having ankylosing spondylitis with the use of a rigid external distraction and mandibular set back technique. Keywords: Distraction osteogenesis, mandibular setback, rigid external distraction
How to cite this article:
Ayyildiz E, Gelgor IE. Maxillary advancement with rigid external distractor device and mandibular setback in a severe Class III adult patient. J Orthod Res 2014;2:50-3 |
How to cite this URL:
Ayyildiz E, Gelgor IE. Maxillary advancement with rigid external distractor device and mandibular setback in a severe Class III adult patient. J Orthod Res [serial online] 2014 [cited 2018 Apr 5];2:50-3. Available from: http://www.jorthodr.org/text.asp?2014/2/1/50/125933 |
| Introduction | |  |
Class III skeletal malocclusion, which is one of the most complainable anomaly by patients can be the result of mandibular prognathism and/or maxillary deficiency. [1] When the dental compansation therapy is not satisfactory choice in these anomalies, orthognatic surgery is unique treatment alternative. With the advancements in surgical techniques and knowledge, today bimaxillary surgical procedures are frequently used to correct this anomaly so that only mandibular set back operations had been performed in the past. [2] Although the mandibular set back is generally performed with sagittal splint osteotomy, maxillary advencement is applied with LeFort I osteotomy in one movement or distraction of maxillae intraorally and extraorally.
Distraction osteogenesis or callus distraction, which is a process of bone regeneration between the surfaces of vascularized bone segments separated by gradual distraction is a method of bone generation without using bone or soft-tissue grafts. It was first described by Codvilla [3] in 1905 and mechanical rules of this method were defined by Illizarov in 1988. [4] DO technique has gained popularity in the treatment of craniofacial dysplasias and supplies significant improvements in skeletal and soft-tissue changes.
The application of distraction osteogenesis for maxillary advancement was introduced in 1993 and today it is widely used in cases of skeletal Class III malocclusion caused by maxillary deficiency. [5],[6],[7],[8],[9],[10],[11],[1]2[,13],[14] Polley and Figueroa [12] reported the method called rigid external distraction (RED) system in 1997 firstly and this has been used for maxillary advancement for many years.
The purpose of this report is to present the orthodontic-orthognathic treatment of a patient with severe Class III skeletal malocclusion having ankylosing spondylitis with the use of a RED and mandibular set back technique.
| Case Report | |  |
Patient
This was a case report of a 32 year-old male presented with a severe maxillary transversal and sagittal deficiency, mandibular prognathi and anterior oppenbite was referred to our clinic for Maxillo-Oral Disorders at Kirikkale University, Faculty of Dentistry, Departmant of Orthodontics, Kirikkale [Figure 1]. 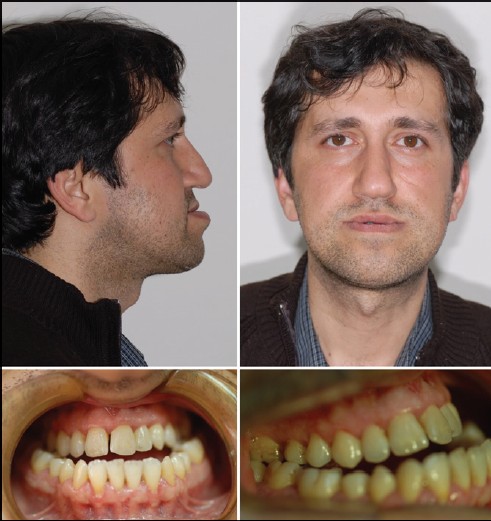 | Figure 1: Extraoral and intraoral photos of the patient before treatment
Click here to view |
The patient had ankylosing spondylitis, which is a chronic inflammatory disease of the axial skeleton and is under the control medically. The treatment plan was as follows:
- Dental decompensation in maxillary and mandibular arches by fixed orthodontic treatment.
- Maxillary advencement with RED.
- Mandiblar set back.
Treatment Progress
Correction of the maxillary transversal deficiency and upper midline discrepancy was ignored because of the longer treatment time and patient unwillingness about them. After all dental compensations were eliminated orthodontically and applying of rigid arch wires, intraoral part of RED system (KLS Martin, Tuttlingen, Germany) for maxillae was prepared [Figure 2]. Intraoral appliance was inserted to upper jaw and then complete high Le Fort I osteotomy including septal and pterygomaxillary disjunction with mobilization was applied.
The extraoral portion of the RED system was placed to the cranium using the scalp pins. Traction wires connecting to outer arms of the intraoral applance and apertura piriformis for midfacial advencement were attached to the adjustable distraction screws. After a latency period of 4 days, distraction was initiated forwardly at a rate of 0.5 mm twice a day. the distraction period was 10 days including overcorrection [Figure 3]. After the consolidation period of 6 weeks, second surgery was performed for mandibular set back and fixation of maxillae with miniplates. Lateral cephalometric radiography were utilized for pre- and post-treatment evaluations.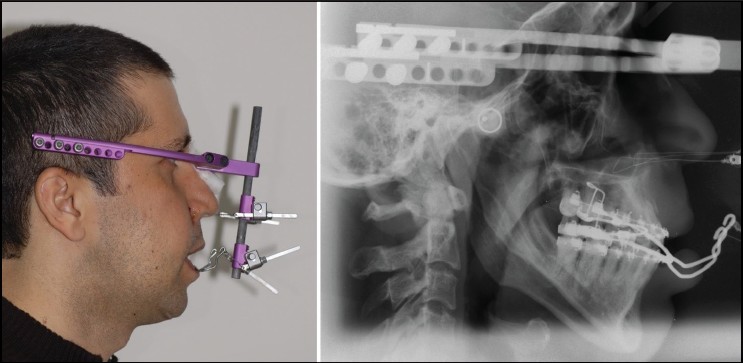 | Figure 3: Rigid external distraction system and cepholametric view of application
Click here to view |
Treatment Results
Because of using RED system [Figure 3], midfacial retrusion was satisfactorly disappeared from the infraorbital region to the upper lip. In addition, results of setting back and counter clockwise rotation of mandible as a secondary surgical operation demonstrated improvements in both skeletal convexity and maxillomandibular and dental relationships [Figure 4] and [Figure 5].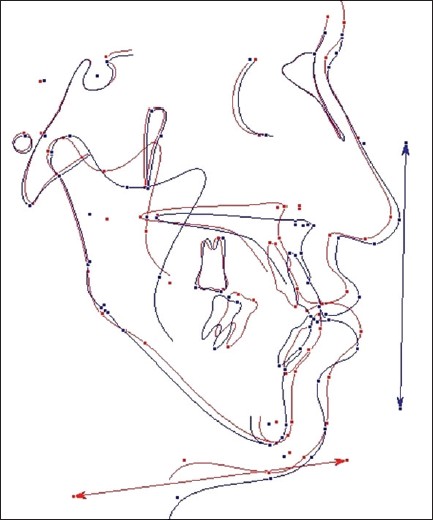 | Figure 4: Superimposition of pre-and post-treatment lateral cephalometric tracings. Red colored line represents pre-treatment lateral cephalometric tracing and blue colored line represents post-treatment cephalometric tracing, 6 months after removal of rigid external distraction device
Click here to view |
When the cephalometric analysis was performed after removal of RED, A point showed forward displacement of 13.0 mm. No relapse was noted within the first 3 months after removal of RED in maxillae and mandible.
| Discussion | |  |
The physical deformities associated with maxillary deficiency and mandibular prognathi lead to multiple functional deficiencies. These include severe malocclusions that result in compromised mastication and speech and nasal pharyngeal airway patency. The severe concave facial profile has negative psychosocial ramifications. [12] Distraction osteogenesis has been used recently to correct a wide range of these craniofacial defects. Many of reports indicated that DO is more suitable than conventional osteotomy. [15],[16],[17] Because the gradual stretching in soft-tissue by distraction osteogenesis, natural soft-tissue resistance can be overcome. With the simultaneous expansion of associated soft-tissues, relapse risk reduces. [18],[19] DO also supplies a greater amount of maxillary advancement than is noted with standard maxillary advancement, which was 13.0 mm in this case.
Using of RED device for advancement of maxillae allows predictable control over the distraction process. Due to adjustability of the device, clinician can change the vertical and horizontal vector of distraction at any time, without an interruption during the process, if necessary. Application of RED device at LeFort I level also provides complete versatility in both the amount of advancement and direction of the distraction process. Therefore, in this case we have used a commercially available face bow for preparing of the intraoral part of RED. In this way, one can adjust easily the tractional extraoral arms according to resistance centre of maxillae whatever if he wants.
When we look at the literature, researchers suggest that it is important to improve skeletal problems as soon as possible in childhood, for psychological and functional reasons. For this reason RED device was applied before growth termination in these studies. [11] Our patient was adult having ankylosing spondylitis with poor cortical bone quality and the amount of the maxillary advancement that needed was over. For all these reasons, we choose the distraction treatment for maxillary advencement. Treatment period in distraction osteogenesis allows the bone healing because of gradual activation and this is a good chance for our patient to reduce relapse. Furthermore, many of the reports also indicated that relapse rates after distraction were lower than after conventional osteotomy because of good soft-tissue adaptations. [20],[21],[22]
Mandibular set back is a way of correction of prognathi and gonial angle also. When we correct the gonial angle, counterclockwise rotation of mandible was occured simultaneously and this caused normal facial harmony and proper vertical dimension.
It is obvious that if indicated, application of RED in patients having severe maxillary sagittal deficiency can be a treatment alternative. Distraction osteogenesis supplies effective skeletal maxillar advancement and better adaptation in surruounding soft-tissue than convansionel osteotomy.
| Acknowledgment | |  |
The Author would like to thank the patient for providing consent to use her photograph in this article.
| References | |  |
| 1. | Obwegeser HL. Surgical correction of small or retrodisplaced maxillae. The "dish-face" deformity. Plast Reconstr Surg 1969;43:351-65. 
[PUBMED] |
| 2. | Chen F, Terada K, Hua Y, Saito I. Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am J Orthod Dentofacial Orthop 2007;131:372-7. 
[PUBMED] |
| 3. | Codivilla A. The classic: On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. 1905. Clin Orthop Relat Res 2008;466:2903-9. 
[PUBMED] |
| 4. | Ilizarov GA. The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst 1988;48:1-11. 
[PUBMED] |
| 5. | Burstein FD, Williams JK, Hudgins R, Graham L, Teague G, Paschal M, et al. Single-stage craniofacial distraction using resorbable devices. J Craniofac Surg 2002;13:776-82. 
[PUBMED] |
| 6. | Cohen SR, Holmes RE. Internal Le Fort III distraction with biodegradable devices. J Craniofac Surg 2001;12:264-72. 
[PUBMED] |
| 7. | Tate GS, Tharanon W, Sinn DP. Transoral maxillary distraction osteogenesis of an unrepaired bilateral alveolar cleft. J Craniofac Surg 1999;10:369-74. 
[PUBMED] |
| 8. | Nakagawa K, Ueki K, Takatsuka S, Marukawa K, Yamamoto E. A device for determining the position of intraoral distractors for protracting the maxilla. J Craniomaxillofac Surg 2003;31:234-7. 
[PUBMED] |
| 9. | Kitai N, Kawasaki K, Yasuda Y, Kogo M, Murakami S, Kreiborg S, et al. Rigid external distraction osteogenesis for a patient with maxillary hypoplasia and oligodontia. Cleft Palate Craniofac J 2003;40:207-13. 
[PUBMED] |
| 10. | Cohen SR, Rutrick RE, Burstein FD. Distraction osteogenesis of the human craniofacial skeleton: Initial experience with new distraction system. J Craniofac Surg 1995;6:368-74. 
[PUBMED] |
| 11. | Polley JW, Figueroa AA. Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device. J Craniofac Surg 1997;8:181-5. 
[PUBMED] |
| 12. | Figueroa AA, Polley JW. Management of severe cleft maxillary deficiency with distraction osteogenesis: Procedure and results. Am J Orthod Dentofacial Orthop 1999;115:1-12. 
[PUBMED] |
| 13. | Krimmel M, Cornelius CP, Roser M, Bacher M, Reinert S. External distraction of the maxilla in patients with craniofacial dysplasia. J Craniofac Surg 2001;12:458-63. 
[PUBMED] |
| 14. | Swennen G, Dujardin T, Goris A, De Mey A, Malevez C. Maxillary distraction osteogenesis: A method with skeletal anchorage. J Craniofac Surg 2000;11:120-7. 
[PUBMED] |
| 15. | Nout E, Cesteleyn LL, van der Wal KG, van Adrichem LN, Mathijssen IM, Wolvius EB. Advancement of the midface, from conventional Le Fort III osteotomy to Le Fort III distraction: Review of the literature. Int J Oral Maxillofac Surg 2008;37:781-9. 
[PUBMED] |
| 16. | Fearon JA. The Le Fort III osteotomy: to distract or not to distract? Plast Reconstr Surg 2001;107:1091-103. 
[PUBMED] |
| 17. | Cedars MG, Linck DL 2 nd , Chin M, Toth BA. Advancement of the midface using distraction techniques. Plast Reconstr Surg 1999;103:429-41. 
|
| 18. | Rachmiel A, Aizenbud D, Peled M. Long-term results in maxillary deficiency using intraoral devices. Int J Oral Maxillofac Surg 2005;34:473-9. 
[PUBMED] |
| 19. | Lauwers F, Mayorca-Guiliani A, Lopez R, Woisard-Bassols V, Paoli JR, Boutault F. Maxillofacial intraoral distraction osteogenesis followed by elastic traction in cleft maxillary deformity. Int J Oral Maxillofac Surg 2005;34:85-8. 
[PUBMED] |
| 20. | Fearon JA. Halo distraction of the Le Fort III in syndromic craniosynostosis: A long-term assessment. Plast Reconstr Surg 2005;115:1524-36. 
[PUBMED] |
| 21. | Iannetti G, Fadda T, Agrillo A, Poladas G, Iannetti G, Filiaci F. LeFort III advancement with and without osteogenesis distraction. J Craniofac Surg 2006;17:536-43. 
[PUBMED] |
| 22. | Kuroda S, Watanabe K, Ishimoto K, Nakanishi H, Moriyama K, Tanaka E. Long-term stability of LeFort III distraction osteogenesis with a rigid external distraction device in a patient with Crouzon syndrome. Am J Orthod Dentofacial Orthop 2011;140:550-61. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|