|
 
 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 3
| Issue : 1 | Page : 70-75 |
|
Treatment of Class III malocclusion in a young adult with reverse pull face mask
Zeeshan Iqbal Bhat1, Jayesh S Rahalkar2, Sonali Deshamukh2, Charu Dutta Naik2
1 Dahim Clinic, Al-Hasa, Dammam, Saudi Arabia
2 Department of Orthodontics and Dentofacial Orthopedics, Dr. D. Y. Patil Dental College and Hospital, Pimpri, Pune, Maharashtra, India
| Date of Web Publication | 29-Dec-2014 |
Correspondence Address:
Zeeshan Iqbal Bhat
Dahim Hospital, Al-Hasa, Dammam, 31982, Saudi Arabia
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-3825.147986

Class III malocclusions are usually growth-related discrepancies, which often become more severe until growth is complete. This case report describes the treatment of a young girl aged 11 years 3 months who had a skeletal Class III malocclusion with a flattening of mid facial region. She also had constricted maxillary arch and high labially placed canine. The treatment plan included a slow palatal expansion, reverse pull facemask appliance, and fixed edgewise appliances. The treatment resulted in skeletal Class I and dental Class I molar and canine occlusion, an ideal overjet, overbite, incisor angulation and facial esthetics was greatly improved after 21 months of treatment. Stability of the treatment result was excellent in 1 year 5 months follow-up at the age of 14 years and 7 months. Keywords: Class III malocclusion, labially placed canine, maxillary expansion, protraction face mask
How to cite this article:
Bhat ZI, Rahalkar JS, Deshamukh S, Naik CD. Treatment of Class III malocclusion in a young adult with reverse pull face mask. J Orthod Res 2015;3:70-5 |
How to cite this URL:
Bhat ZI, Rahalkar JS, Deshamukh S, Naik CD. Treatment of Class III malocclusion in a young adult with reverse pull face mask. J Orthod Res [serial online] 2015 [cited 2018 Sep 6];3:70-5. Available from: http://www.jorthodr.org/text.asp?2015/3/1/70/147986 |
| Introduction | |  |
Class III malocclusions may occur due to retrognathism of the maxilla, prognathism of the mandible, protrusive mandibular dentition, retrusive maxillary dentition, or combinations of these. For the treatment of Class III maxillary retrusion, the use of reverse pull headgear has been described. [1] This can produce forward movement of the maxilla and posterior rotation of the mandible. [2] Animal studies have shown that forward movement of the maxilla is a result of remodeling of the circum-maxillary sutures. [3] Due to its action in maxillary sutures, to enhance the protraction effect of reverse pull headgear, rapid maxillary expansion is generally used in the treatment of Class III patients. [4] Profit and Fields reported that maxillary expansion must be used before maxillary protraction to mobilize the maxillary sutures. [5]
Here, we present a case report of the treatment outcome of a patient with skeletal Class III who was treated using a maxillary protraction appliance.
Diagnosis and Etiology
An 11 year and 5 month-old young girl came with her parents worried about the unesthetic smile because of high labially placed canine on the left side of her maxillary dentition.
Her medical history was not contributory. Clinically her profile was straight with retrusive nasomaxillary area, prominent lower third of the face, the lips were competent, and no mentalis strain. Vertical facial proportions were normal and there were no significant asymmetries [Figure 1]. Full complements of permanent teeth were present. In both centric occlusion (CO) and centric relation (CR) molar relationship were Class III, and right canine and incisors were in Class I relationship. UL3 was labially placed, 4 mm of maxillary midline shift to the left side was present in relation to the mandibular and facial midline. She had asymmetric arches with mild to moderate mandibular crowding. The curve of Spee was moderate with a 2.5 mm overbite in both CO and CR. Both the maxillary and the mandibular arches exhibited moderate arch length discrepancies. Oral hygiene and gingival conditions was good [Figure 2]. The pretreatment lateral cephalometric and orthopantomogram showed highly placed UL3 and fully erupted dentition except third molars, which were in erupting phase. The cephalometric analysis showed she was in the third stage of cervical vertebrae maturation indicator, a skeletal Class III relationship (ANB −2°, Ao-Bo −3 mm) with a retrognathic maxilla and mandible in relation to the cranial base (SNA −77°, SNB −79°), vertically she presented a short face that is, a hypodivergent skeletal pattern (SN-GoGn −31°, FMA −24°), proclined maxillary incisors (U1-NA7 mm and 34°, U1-SN −111°, U1-APog 6 mm and 30°) and retroclined mandibular incisors (L1-NB, 3 mm and 20°, L1-APog −2 mm and 20°, IMPA −89°), length of the maxilla was short in relation to the cranial base (Ba-ANS 86 mm, Ba-PNS 39 mm, PNS-ANS 46 mm) [Figure 3] and [Table 1].
Treatment Objectives
Due to the patient's skeletal disharmony, it was informed to the parents about the skeletal discrepancy and need for management of the same by orthognathic surgery. However, we also informed them of the possibility of a nonsurgical approach.
Our treatment objectives were:
- To improve the skeletal jaw relationship as much as possible by increasing the length of maxilla and bringing the maxilla anteriorly in relation to the cranium,
- Maxillary expansion,
- To bring UL3 into the arch,
- To align arches,
- To correct symmetry of the arch,
- To correct midline deviation and
- To provide an esthetic smile.
Treatment Plan
Phase I: Expansion of the maxillary arch with fixed quad helix until lingual cusp of maxillary premolars and molars touches the buccal cusp of mandibular premolars and molars. Maintain the space for UL3. Petit type face mask with 400-450 g of force.
Phase II: Extraction of all four bicuspids. Simultaneous retraction and protraction of maxillary anteriors and posteriors. Retraction and intrusion of mandibular anteriors.
Treatment Progress
Treatment was started at the age of 11 years and 5 months with maxillary expansion with fixed quad helix, which was cemented on the first maxillary molars in order to uncross the bite and disarticulate the sutures of the nasomaxillary complex, facilitating the protraction, making it more efficient. Before cementation of the helix 4.5 mm of activation was done extra orally. Simultaneously, Full size metal brackets 0.018-inch MBT preadjusted appliance (American orthodontics) on maxillary anterior teeth were bonded. The opening arch wire was 0.014 nickel-titanium (NiTi). 2 months later maxillary premolars were bonded and 0.016 stainless steel (SS) A.J. Wilcock wire was put with open coil spring between UL2 and UL4 to open up the space to bring canine into the arch. Immediately, Petit type protraction face mask was installed, heavy elastics were applied between the maxillary molar hooks to the horizontal bar of the face mask, which liberated a force of 450 g/side. The traction level of the elastics (5/16 inch by 14 ounces) showed anteroinferior direction approximately 20-30° below of the occlusal plan; the distance between the elastic 1/2" heavy was far from 1 to 1.5 cm below of the labial commissure. The patient was instructed to use the face mask at least 18 h/ day. There evaluations were made fortnightly for a period of 4 months. After the full traction, the face mask was used as retention with the use of 10 h/day, for a period of 4 months.
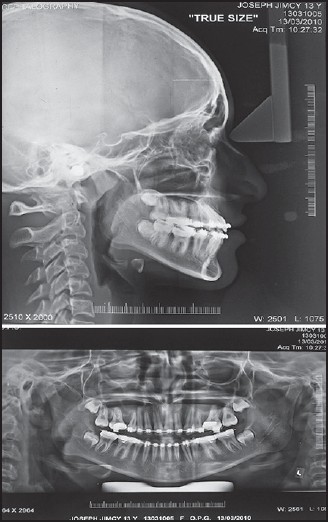
UL3 was bonded 1 month after biscupids bonding and 0.014 temperature-sensitive NiTi as a piggyback wire was fully engaged into it and was ligated on top of the main archwire (0.016 SS A.J. Wilcock) on the adjacent maxillary lateral incisors and maxillary first bicuspid brackets. 1 month later mandibular arch was bonded and 0.014 NiTi wire was given with lacebacks from LR3-LR6, LL3-LL6. 0.016 NiTi was placed for a month engaging the full maxillary dentition, followed by 16 × 22 NiTi and 16 × 22 SS in both maxillary and mandibular arch for the next 3 months. 10 months after the start of the Phase I reverse pull face mask therapy was stopped, quad helix was removed and records were made, all four bicuspids were extracted, lower second molars were included into the arch [Figure 4], [Figure 5] and [Figure 6]. 0.016 NiTi wire was placed for 1 month. Later on, for the next 5 months simultaneous retraction and protraction of the maxillary anteriors and posteriors and retraction and intrusion of mandibular anterior with omega loop in 16 × 22 SS was performed, along with Class III medium elastics. After the space closure 16 × 22 NiTi was placed for 1 month. Final records were made before debonding [Figure 7], [Figure 8] and [Figure 9]. Final bracket repositioning was done, [Figure 8] from UR6 to UL6 under 0.016 NiTi wire and posterior settling elastics were given for next 2 months followed by 16 × 22 SS for last 2 months.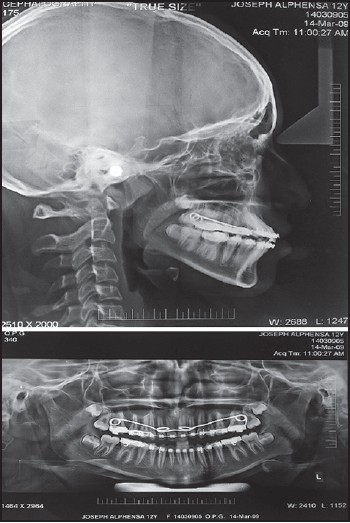 | Figure 6: Post Face Mask therapy (orthopantomogram, lateral cephalogram)
Click here to view |
 | Figure 9: Post fixed appliance therapy (orthopantomogram, lateral cephalogram)
Click here to view |
At the end of treatment at age 13 years and 2 months, the patient had a much improved aesthetic smile, which had been the primary reason for seeking treatment. The total treatment time was 21 months.
Growth treatment response vector analysis was performed on pre- and post-treatment lateral cephalograms, which showed the ratio was 0.71 which was good for treatment as further surgery might not be required. Overall superimpositions showed favorable growth of the maxilla and mandible [Figure 10].
After 1.5 years in retention, the occlusion was well maintained [Figure 11] and [Figure 12].
Lateral to lateral lingual bonded retainers in maxillary archand bicuspid to bicuspid lingual bonded retainer in the mandibular arch along with full time wear Hawley's retainer. Cephalometrically the measurements were close to ideal.
Patient compliance was excellent throughout the treatment.
Treatment Results
At the end of treatment, the cephalometric analysis showed a significant change in cranio-maxilla-mandibular relationship [Table 1] (SNA 77 → 81, SNB 79 → 80, ANB −2° → 1°, Ao-Bo - 4 mm → 0 mm), an increase in the maxillary length (CO-A 76 mm → 84 mm, Ba-PNS 39 mm → 42 mm, Ba-ANS 86 mm → 91 mm, PNS-ANS 46 mm → 49 mm) and there was a change in mandibular growth pattern as well (FMA 24° → 26°, GoGn-SN 31° → 31°).
As for the occlusal changes, a well-aligned dentition with Class I molar and canine relationship was achieved. The patient had a consonant smile arch, the teeth had good inter digitation, the proclination of the maxillary incisors was increased (30° → 32°), there was no reduction in the interincisal angulation (127°) due to a significant decrease in the projection of the lower incisors (L1-APg 3 mm → 1 mm, 23° → 21°). The maxillary and mandibular midlines were coincident with the facial midline. The posttreatment panoramic radiograph showed no apparent root resorption of the teeth [Figure 11] and [Figure 12].
| Discussion | |  |
The success of orthodontic treatment in a growing patient with a severe Class III malocclusion depends on his or her individual growth and the adequate timing of the treatment. Sung and Baik reported that comparison of treatment effects according to age showed no significant difference. [6] Kapust et al. divided subjects into three age groups and found minimal significant differences between the groups. [7] Here we treated this patient by a growth modification treatment with expansion of the maxillary arch, protraction face mask appliance followed by fixed orthodontic treatment.
Several studies have shown that 25-41% of Class III problems in children are primarily the result of a retrognathic maxilla. [8],[9] These studies, using cephalometrics and histologic techniques, showed that treatment with an anterior force on the maxilla is capable of causing disassociation of sutural articulations by a resorption and apposition process at the sutural interfaces. In recent years majority of studies have indicated that a simultaneous sutural expansion at the start of protraction headgear treatment facilitates the anterior movement of the maxillary dentition, a significant extrusion of the upper molars, anterior displacement of the maxillary dentition, 1-3 mm anterior displacement of the maxilla, and a significant rotation of the mandible downward and backward. In addition, the effect of the maxillary protraction by a face mask is usually a combination of skeletal and dental movements. [10],[11] The stability of the results seems to be associated with the posttreatment holding time, suggesting the use of the face mask for 10 h/day, during 4-6 months. [10],[12]
Maxillary arch was over expanded with an anticipation of possible relapse, she was asked to wear the face mask for 18 h/day for 4 months, followed by 4 months of retension 10 h/day. Also, for the maxilla to advance forward in each affected suture, numerous areas of resorption and apposition have to take place due to their tortuous nature, quite unlike the midpalatal suture. Thus, the sutural anatomy and age of the patient play a major role in determining the amount of force needed to bring the maxilla forward with protraction forces. Hickham recommends from 600 g to 800 g/side, [13],[14] while for Baccetti, from 225 g to 400 g/side would be enough for protraction. In this study, we used the level of force of 450 g/side.
In facemask therapy with tooth-borne anchorage, several studies [10] have reported counter clockwise rotation of the maxilla, clockwise rotation of the mandible, and increase in lower facial height. In the present study, there was a change in anteroposterior facial height ratio, counterclockwise rotation of the maxilla and increase in lower facial height was significant (posterior/anterior face height −62.3%, ANS-Me −49 → 53). This could be because an anterior force on the midface applies equal and opposite force on the forehead and chin. The direction of the force on the chin is distal and almost in a straight line, which can also cause a rotation of the mandible downward and backward.
Patient was treated with fixed appliances, in order to align the dentition 0.014 NiTi was kept in the ice cold water for some time to make the wire more flexible (austenite to martensite) and attached to UL3 which was later brought into the arch after sufficient expansion and opening the space between UL2 and UL4 with open coil spring. Simultaneous retraction and protraction of the maxillary anteriors and posteriors and retraction of mandibular anteriors with omega loop in 16 × 22 SS was performed, along with Class III medium elastics, this was to achieve the ideal labiao version of incisors, relieve the lip strain and to correct the Class III molar relationship. Class III elastics maintained the Class I skeletal correction achieved during Phase I.
There was a significant difference in the amounts of labioversion of the maxillary incisors, they were more pronounced than was at the start of the treatment which contributes in increase of overjet. Mandibular incisors were tipped lingually, which were in accordance with the results of a previous study. [11] Case was later finished with 16 × 22 SS wire for 2 months in both the arches to express sufficient torque.
Growth treatment response vector analysis was performed which showed the ratio was 0.71, calculation allows clinician to inform whether malocclusion can be camouflaged with orthodontic treatment or if surgical treatment will be required at a later age. [15] Tweed reported that when the FMA is between 28° and 35°, the vector of growth is not very favorable. However, if the angle approaches 28°, the prognostic is more favorable. [16] We agree with this finding since the patient had the FMA in 26°, what favored the success of the treatment.
Although camouflage treatment of skeletal Class III malocclusion is successful in some patients, careful attention should be paid until the end of growth. Moreover, the important benefits of early treatment should not be denied because of concerns that a few patients may still require further treatment.
| Conclusion | |  |
In properly selected cases, dentoalveolar camouflage for Class III malocclusion by growth modification with the maxillary expansion and protraction facemask appliance can be a useful modality of treatment.
The reported case was a young female with a straight profile and a normal vertical facial pattern, who had completed 45-65% of her growth. Class III malocclusion was corrected in 21 months using a maxillary protractor face mask, maxillary expansion and fixed orthodontic treatment and maintained during 1.5 years of fixed treatment. However, long-term observation of this patient will be necessary, since mandibular growth still occurs in adolescence. A reverse pull face mask was effective for the treatment of this young adult with skeletal Class III malocclusion.
| References | |  |
| 1. | Potpeschnigg H. A tooth straightening machine. German Quarter-Zahnheilk 1875;15:34-6.  |
| 2. | Irie M, Nakamura S. Orthopedic approach to severe skeletal Class III malocclusion. Am J Orthod 1975;67:377-92.  |
| 3. | Kambara T. Dentofacial changes produced by extraoral forward force in the Macaca irus. Am J Orthod 1977;71:249-77.  |
| 4. | McNamara JA Jr. An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod 1987;21:598-608.  |
| 5. | Proffit WR, Fields HW Jr. Contemporary Orthodontics. 3 rd ed. St Louis: Mosby; 1993. p. 508-15.  |
| 6. | Sung SJ, Baik HS. Assessment of skeletal and dental changes by maxillary protraction. Am J Orthod Dentofacial Orthop 1998;114:492-502.  |
| 7. | Kapust AJ, Sinclair PM, Turley PK. Cephalometric effects of face mask/expansion therapy in Class III children: A comparison of three age groups. Am J Orthod Dentofacial Orthop 1998;113:204-12.  |
| 8. | Guyer EC, Ellis EE 3rd, McNamara JA Jr, Behrents RG. Components of class III malocclusion in juveniles and adolescents. Angle Orthod 1986;56:7-30.  |
| 9. | Williams S, Andersen CE. The morphology of the potential Class III skeletal pattern in the growing child. Am J Orthod 1986;89:302-11.  |
| 10. | Ngan P, Hägg U, Yiu C, Merwin D, Wei SH. Treatment response to maxillary expansion and protraction. Eur J Orthod 1996;18:151-68.  |
| 11. | Nartallo-Turley PE, Turley PK. Cephalometric effects of combined palatal expansion and facemask therapy on Class III malocclusion. Angle Orthod 1998;68:217-24.  |
| 12. | Baccetti T, Franchi L, McNamara JA Jr. Treatment and posttreatment craniofacial changes after rapid maxillary expansion and facemask therapy. Am J Orthod Dentofacial Orthop 2000;118:404-13.  |
| 13. | Ngan PW, Hagg U, Yiu C, Wei SH. Treatment response and long-term dentofacial adaptations to maxillary expansion and protraction. Semin Orthod 1997;3:255-64.  |
| 14. | Hickham JH. Maxillary protraction therapy: Diagnosis and treatment. J Clin Orthod 1991;25:102-13.  |
| 15. | Ngan P. Early timely treatment of Class III malocclusion. Semin Orthod 2005;11:140-5.  |
| 16. | Tweed CH. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am J Orthod Oral Surg 1946;32:175-230.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10], [Figure 11], [Figure 12]
[Table 1]
|