|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 3
| Issue : 3 | Page : 181-187 |
|
The effect of corticotomy on tooth movements during canine retraction
Fatma Deniz Uzuner1, Emel Yücel1, Betül Göfteci2, Ayse Gülsen3
1 Department of Orthodontics, Faculty of Dentistry, Gazi University, Ankara, Turkey
2 Private Periodontolog, Istanbul, Turkey
3 Department of Plastic Reconstructive and Aesthetic Surgery, Faculty of Medicine, Gazi University, Ankara, Turkey
| Date of Web Publication | 11-Sep-2015 |
Correspondence Address:
Fatma Deniz Uzuner
Department of Orthodontics, Gazi University Faculty of Dentistry, Biskek Cd. (8.Cd.) 82.Sk., No: 4, 06510 Emek, Ankara
Turkey
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-3825.159548

Objectives: The objective was to evaluate the effect of corticotomy/corticectomy surgery combined with fixed appliances on tooth movement during the canine retraction phase. Materials and Methods: We assessed 13 postpubertal patients (3 males and 10 females) requiring extraction of both maxillary first premolars. One side of the upper dental arch was treated with a PG retraction spring as a control, while the other side was treated with combined corticotomy/corticectomy surgery and a PG spring. A force of 100 g was used for canine retraction on both sides, with activation of the spring monthly on the control side and once every 15 days on the combined treatment side. A paired t-test was used to assess the difference between the two sides. Results: There was a small but statistically significant reduction in the duration of canine retraction (P < 0.05) and an increase in the rate of canine retraction (P < 0.05) (mm/month) in the combined treatment group. No difference in anchorage loss was observed between the groups. Tipping per millimeter of retraction was significantly different between the groups (P < 0.05). Conclusion: Corticotomy-assisted orthodontics increased the rate of tooth movement during canine retraction in 20% ratio. Relative bodily tooth movement was achieved with the corticotomy combined treatment. Keywords: Canine retraction, corticotomy, dentoalveolar surgery, PG retraction spring
How to cite this article:
Uzuner FD, Yücel E, Göfteci B, Gülsen A. The effect of corticotomy on tooth movements during canine retraction. J Orthod Res 2015;3:181-7 |
How to cite this URL:
Uzuner FD, Yücel E, Göfteci B, Gülsen A. The effect of corticotomy on tooth movements during canine retraction. J Orthod Res [serial online] 2015 [cited 2018 Sep 6];3:181-7. Available from: http://www.jorthodr.org/text.asp?2015/3/3/181/159548 |
| Introduction | |  |
Incorporation of corticotomy into orthodontic treatment is claimed to allow faster tooth movement, thereby making it possible to shorten treatment time and increase the quality of orthodontic services to adult patients. [1],[2],[3],[4],[5] Acceleration in the rate of tooth movement may occur because the resistance of the dense cortical bone to orthodontic tooth movement is disrupted. [6],[7] Suya [1] described orthodontic tooth movement involving corticotomy as a process of moving blocks of bone rather than moving only the teeth themselves. Recently Wilcko et al. [4],[8] attributed this movement to a regional acceleratory phenomenon (RAP) which is characterized by alterations within the periodontal ligament (PDL) and an increase in bone turnover, as well as the demineralization process that occurs in the cancellous bone surrounding the tooth socket. Based on the histological results showing that RAP accelerates the appearance of macrophages 1 week after the initiation of orthodontic forces. In another view, Mathews and Kokich [9] proposed that the acceleration in the rate of tooth movement is due to the earlier removal of hyaline, which allows earlier bone resorption.
In addition, it is claimed that the teeth may be more stable after this type of combined treatment and that relapse is less likely because of the minimal disruption to the PDL by osteoclastic activity. [1],[2],[3],[6] In addition, the callus formed as the bone heals may further increase stability. [1],[2],[3] Wilcko et al. [8],[10] suggested that the stability of orthodontic treatment provided may be due to the increased thickness of the alveolar cortices caused by bone grafting of the facial and lingual cortical plates, as well as the loss of tissue memory resulting from the high tissue turnover of the periodontium.
These reported benefits suggest that surgery combined with orthodontic treatment during the canine retraction phase may be useful both for reducing the treatment time and the risk of root resorption. Combined treatment in canine retraction was first defined by Kole [11] in 1959. To improve canine retraction he applied a vertical cut to the mandibular canine's mesial interproximal cortex. Later on in their case report Gantes et al. [2] described the application of a U-shaped corticotomy to the maxillary canine, and an ostectomy both buccally and palatally to the first premolar extraction socket. In addition, Wilcko et al.[4],[8] applied bone grafting according to the periodontally accelerated osteogenic orthodontics protocol after corticotomy.
In the literature, different types of alveolar surgery techniques combined with orthodontic treatment were reported during canine retraction phase, [2],[3],[5],[8],[9],[10],[11],[12],[13],[14],[15] but few of them were clinical studies with statistical evaluations. [5],[12],[13],[14],[15] As suggested by Mathews and Kokich, [9] there is a need for further research measuring the quality of combined treatment relative to the time of treatment.
There is no clinical study evaluating the effects of U-shaped corticotomy combined canine retraction with sectional retraction springs.
The present study was designed to evaluate the effect on tooth movement of U-shaped corticotomy/corticectomy surgery combined with sectional retraction springs applied to canines during the canine retraction phase. It was hypothesized that with the surgery combined canine retraction method canine retraction would be achieved in a shorter period of time with reduced anchorage loss compared with conventional method.
| Materials and Methods | |  |
A total of 13 postpubertal adolescent patients (3 male, 10 female) with a mean age of 17 years 8 months (±1 year 10 months), whose upper first premolars were indicated to be extracted, were included in this study. Inclusion criteria were : n0 o requirement for maximum anchorage, no requirement for alignment in the posterior region, no skeletal anomalies, and no periodontal or systemic problems that may contraindicate surgery. The sample size of 13 patients per group, at α = 0.05, yielded a statistical power close to 0.80.
Written informed consent was obtained from each subject following a detailed explanation of the objectives and protocol of the study, which was conducted in accordance with the ethical principles stated in the Declaration of Helsinki and approved by the Ethics Committee of Gazi University.
Study design and procedures
One side of the upper dental arch was selected as the control side, to which only a retraction mechanism was applied; the other side (combined treatment side) was treated with combined corticotomy/corticectomy surgery and the same retraction mechanism.
Before the surgery, the root length of the canine was evaluated using a periapical radiograph taken with a reference arch bonded on the canine.
The same periodontist performed all surgery under sterile conditions. After infiltrative anesthesia, a buccal and palatal mucoperiosteal flap was reflected between the lateral incisors and first molar teeth on the combined treatment side. Using high speed fissure and round burs with generous irrigation, buccal and palatal corticotomy was undertaken to the canine tooth by creating two vertical cuts beginning 2-3 mm below the crest of the mesial and distal interproximal alveolar bone and extending 2 mm beyond the apex, and a horizontal cut connecting the vertical cuts [Figure 1]a and b. The depth of the cuts was limited to the cortical layer to preserve all the spongy bone. In addition, after extraction of the first premolar tooth, buccal and palatal corticectomy was applied to the cortical layer of the extraction socket [Figure 1]b. After surgery, antibiotics (Cliacin® 1,200,000 IU [2 × 1]), anti-inflammatory drugs (Dolorex® ), and chlorhexidine were given to patients for prophylaxis.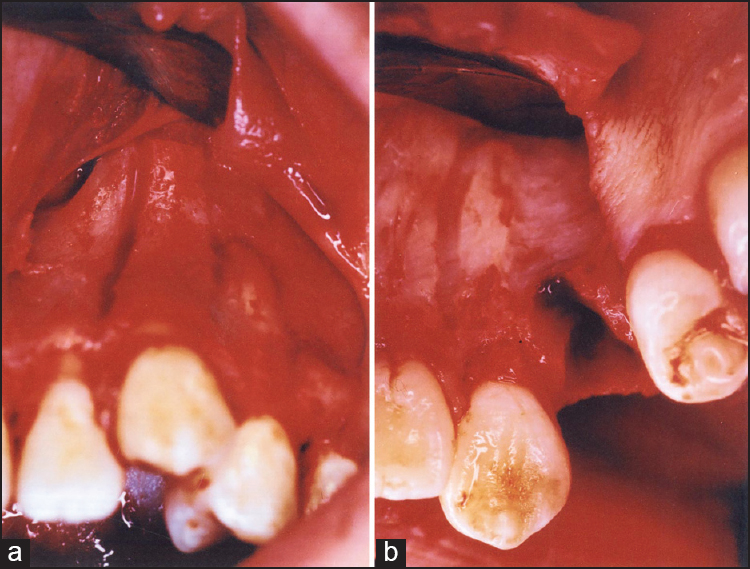 | Figure 1: (a) Corticotomy applied to the canine (b) corticectomy applied to the extraction socket
Click here to view |
One week after the first premolar extraction on the control side and surgery on the opposite side, Paul Gjessing's PG canine retraction spring [16],[17] was inserted and the helix strands were separated by 1 mm [Figure 2]. A force of 100 gas validated by a gauge was used for canine retraction on both sides. Activation of the PG spring was undertaken monthly on the control side and once every 15 days on the surgery side as recommended in each technique. [1],[2],[3],[16],[17],[18] At the end of the 1 st month, the springs on both sides were removed, the deformations were controlled and the springs were applied again. No further control was carried out during retraction.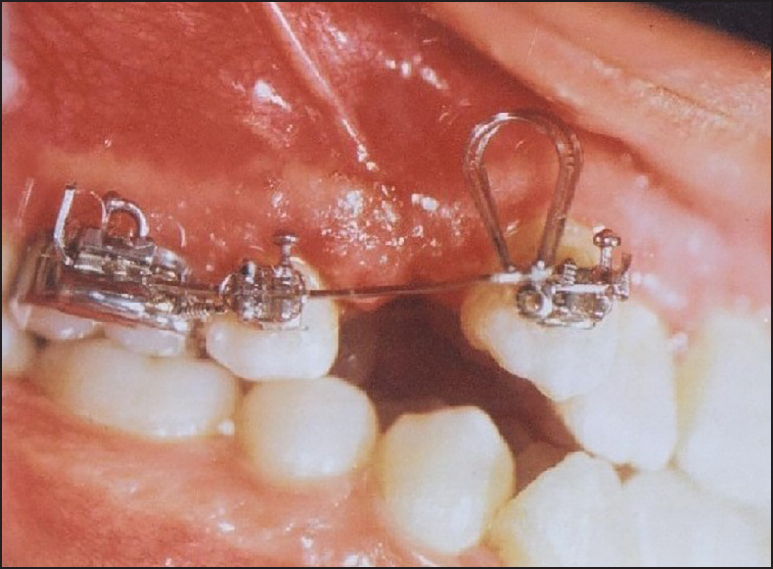 | Figure 2: Clinical application of the PG spring and the activation process
Click here to view |
The study was terminated when the required retraction of the canine was obtained. Model casts and lateral cephalometric and periapical radiographs were obtained before and after retraction.
Cephalometric radiographs were taken for left and right sides separately with the reference arches on the first molars and canines. Structures and reference points necessary for evaluation were traced and marked by the same investigator. Five linear and two angular parameters were measured [Figure 3]. The 8% magnification of the cephalographs that may have affected the measurements was disregarded.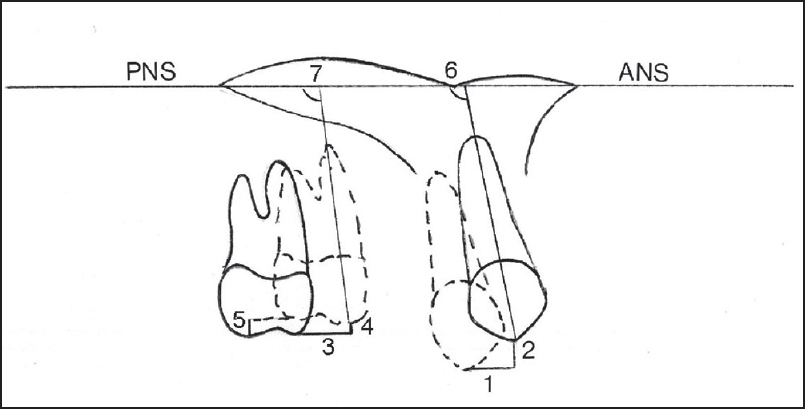 | Figure 3: Linear and angular measurements on lateral cephalographs. (1) 3csag, (2) 3cver, (3) 6 mtsag, (4) 6 mtver, (5) 6dtver, (6) 3/PP, (7) 6/PP
Click here to view |
On the model casts, two angular parameters were evaluated using the occlusogram method [19] [Figure 4].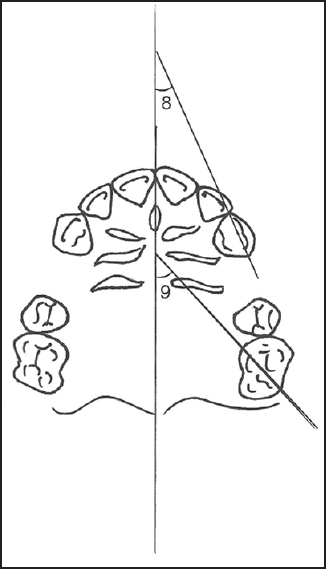 | Figure 4: Angular measurements on model photocopies. (8) Crot°, (9) Mrot°
Click here to view |
Three more parameters, mm/month, 3tip/ret (°/mm), and 6tip/anc (°/mm) were derived from those measured directly on the model casts and lateral cephalographs. [20],[21]
The dates for the start and end of canine retraction were also recorded.
After a 15-day interval 15 cephalographs and 15 model casts were randomly selected and all superimpositions and measurements were repeated.
Statistical analysis
Statistical analysis was undertaken by SPSS version 13.0 (SPSS Inc., Chicago, IL, USA). The error of the method and the intraobserver reliability were determined by the Dahlberg's formula [22] and paired t-test. Paired t-test was used to evaluate the intra- and inter-group differences as well. A level of P < 0.05 was considered statistically significant.
| Results | |  |
In this study, the sample size of 13 patients per group, at α = 0.05, yielded a statistical power close to 0.80.
The method error did not exceed 0.25 mm and 0.5° for any of the variables investigated and the duplicated measurements by the same investigator were not significantly different.
No complications occurred during or after the surgery. The periodontium returned to its healthy appearance within a week.
There were no differences in initial canine and molar positions and tips between the groups [Table 1].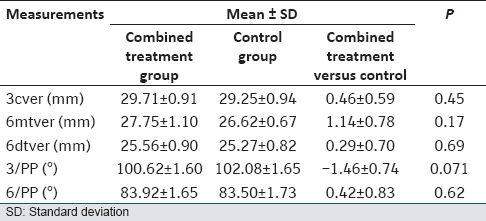 | Table 1: Mean values of the initial vertical position and tip of the canine and first molar at the beginning of canine retraction in control and combined treatment groups (n = 13)
Click here to view |
No significant difference was found for canine crown retraction (3csag) between the groups [Table 2].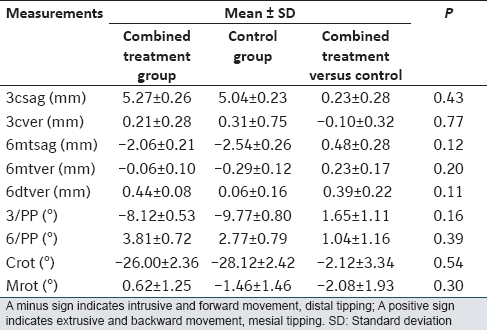 | Table 2: Mean changes during canine retraction in control and combined treatment groups (n = 13)
Click here to view |
The mean (standard deviation) duration of canine retraction was significantly shorter in the combined treatment group (153 days) compared with the control group (184.8 days) [P < 0.05; [Table 3]].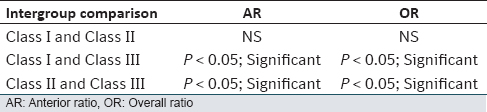 | Table 3: Mean retraction time and mean changes for the derived parameters in the combined treatment and control groups during canine retraction (n = 13)
Click here to view |
The rate of canine retraction (mm/month) was significantly higher in the combined treatment group (1.05 mm/month) than the control group (0.92 mm/month) [P < 0.05; [Table 3]].
In both groups, loss of anchorage occurred through mesial movement of the crown (6 mtsag) [Table 2].
When vertical movement of the canines (3cver) was evaluated; canine crowns were on average slightly extruded in both groups. First molar mesial cusp (6 mtver) was intruded in both groups. However, the distal cusp of the first molar (6dtver) was extruded. No significant differences were found in the vertical movement of the molar and canine crowns between the groups [Table 2]. The canines rotated (Crot°) mesiobuccally in both groups. In contrast, molars rotated (Mrot°) differently in each group. Although on average the molars showed 0.62° of mesiopalatal rotation in the combined treatment group, and 1.46° of mesiobuccal rotation in the control group, the difference was not statistically significant [Table 2].
On average, the canines tipped (3/PP) distally and the first molars tipped (6/PP) mesially in both groups. There were no significant differences in molar and canine tipping between the groups [Table 2]. While the mean degree of tipping per millimeter of canine retraction (3tip/ret) distally differed significantly between the combined treatment group (1.55°/mm) and the control group (1.96°/mm) (P < 0.05); no significant difference was found in tipping per millimeter of anchorage loss (6tip/anc) between the two groups [Table 3].
| Discussion | |  |
The aim of this study was to determine the extent to which cortical bone resistance affected tooth movement during the canine retraction phase. In view of the benefits of surgery to the dentoalveolar process combined with orthodontic treatment methods on postadolescents and adults, [1],[2],[3] corticotomy/corticectomy methods were used to decrease canine retraction time with desirable tooth movement.
The surgical technique used in this study was differed from the techniques of interseptal bone reduction, [12] micro-osteoperforations, [13] a series of small cortical perforations [5],[14] that were used by other researchers. In this study, buccal and palatal corticotomy was undertaken to the maxillary canine tooth by applying two vertical cuts and one horizontal cut connecting the vertical cuts, similar to the technique described by Gantes et al. [2] and Anholm et al. [3] However, unlike them buccal and palatal corticectomy rather than ostectomy was applied to the cortical layer of the extraction socket after extraction of the first premolar; because after ostectomy the socket osteogenesis could have been inadequate and bone loss could have occurred. Because corticotomy and corticectomy preserved the spongy bone, no bone loss was observed in this study. In addition, no grafting was applied over the corticated bone, unlike Wilcko et al. [4],[8]
Some authors [1],[2],[3],[5],[15] advocate applying the orthodontic force immediately after the corticotomy because osteoblastic activity starts 2 weeks to a month after surgery; in other words, the blocks of bone created by the corticotomy start to connect. Itoh et al., [23] however, advised that the orthodontic force application should commence after the reactive inflammation caused by the surgery disappears. Similarly, Kole [11] applied the force 8 days after the surgery. Wilcko et al. [8] advocate applying the force 1 month after the surgery and bone grafting procedure. In this study, in a similar procedure to those of Kole [11] and Itoh et al. [23] the force was applied 1 week after the surgery to allow wound healing to occur and to eliminate the discomfort caused by the surgery.
A non-frictional system was preferred for canine retraction because it exerts a more constant force than a frictional system, eliminating any effect of the incisors on tooth movement. In addition, friction may cause a delay in canine retraction, contradicting the principal aim of the present study which was the achievement of optimal speed of tooth movement. [16],[21] Differently, other researchers [5],[13],[14],[15] used frictional systems in which canines were retracted by closed coil springs or elastic chains on continuous arches.
Given that osteogenesis starts after the surgery [1],[13],[24] and despite Gjessing's [16],[17] recommendation, in this study the PG spring was applied without waiting for the leveling phase so as not to lose the advantages of surgery. As patients without severe alignment needs were included in this study, we encountered no problems with the construction of springs. Similarly, Gantes et al. [2] used sectional arches (reverse closing loops) for canine retraction without leveling after the corticotomy and ostectomy in their study, while others [5],[14],[15] waited for the completion of the leveling and alignment phase of the treatment, before undertaking the corticotomy and starting canine retraction.
If adjustment of the orthodontic force is undertaken at intervals of 3-4 weeks, the process of tooth movement will be delayed and healing of the alveolar bone may occur. [1] Therefore, as recommended [1],[3] the springs were activated every 15 days in the combined treatment group. However, for the control group it was thought that activation every 15 days could cause hyalinization [16],[17],[18] and delay tooth movement, so activation was carried out monthly. In another word in control group, conventional canine retraction process was applied with retractions springs. Every 15 days, the activation of the springs was evaluated and determined to be nearly deactivated in the combined treatment group although they were still active in the control group. It is claimed that corticotomy combined orthodontic treatment requires a greater magnitude of force than other treatment techniques. [1],[2],[3],[24] By contrast, Itoh et al. [23] maintained that because the main source of resistance was reduced by surgery and the remodeling of the surrounding bone was facilitated, a light force of 160 g was sufficient. Other researchers [5],[13],[14],[15] applied the range of 100-200 g force for maxillary canine retraction in their study. Higher levels of force could not be applied in this study design because of the risk of hyalinization on the control side. Therefore, in line with Gjessing's [17] recommendation, we used a light force of 100 g on both the combined treatment side and the control side.
The findings of this study revealed that U-shaped corticotomy combined with fixed orthodontic treatment significantly reduced the duration of canine retraction and significantly increased the speed of retraction (mm/month). Accordingly, retraction duration was significantly reduced in this study population in a 1/5 ratio as Ascher [25] reported, not in a 1/2 ratio as reported by others [1],[2],[3] who used greater force and different surgical techniques in their trials. The result of this study is also differentiated from the other studies who achieved tooth movement that was 2 or 3 times faster than the control with a force level 100-200 g. [5],[14],[15] The reduction in treatment time in this study may differ from other studies because of differences in the levels of force, retraction mechanics and surgical methods used. The rapid rate of the canine retraction in this study might be due to the RAP rather than bony block movement. Although bone blocks surrounding the canines were created, the force level was not high enough as recommended to move the block bones. However, further studies are needed; for evaluating the histological background and for evaluating the effect of higher forces.
This study was limited to evaluate the canine retraction time rather than total treatment time. The effect of this combined treatment to total treatment time was not tested.
It might be hypothesized that; surgery results in disruption of cortical bone resistance around the canine, while, in the posterior region the cortical bone resistance is unaffected and cortical anchorage is preserved. As differential anchorage is occurring during canine retraction, the segmental retraction spring will produce different effects in the anterior and posterior regions and the molar anchorage loss may be reduced. [16],[17],[21],[26],[27],[28] However, the results of this study did not support this hypothesis. In the combined treatment group, mesial movement of the molar crown was less than in the control group, but this difference was not significant. This result is inconcomitant with Abed and Al-Bustani [14] who reported no difference in molar anchorage loss between corticotomy and control sides. Differently, Aboul-Ela et al. [5] reported that no significant anchorage loss occurred on either side in their study. This result can most likely be attributed to the efficiency of the miniscrew implants used for anchorage control in their study rather than the effect of corticotomy.
During retraction, the canines showed extrusion on both sides in our study. Because no leveling was undertaken, the canines were mostly in the vestibulogingival position at the beginning of retraction. There was no significant difference in the vertical position of the canines between the two sides at the beginning of the study. During retraction, the canines moved disto-occlusally, which may explain the extrusion.
The mesiobuccal tubercle of the first molars was determined to be intrusive while the distobuccal tubercles were extrusive. The different vertical movement of the tubercles may be due to mesial tipping of the molars.
Despite preadjustment of the PG arches to produce anti-tipping and anti-rotation moments, this was not enough to counteract the rotation and tipping tendency in both canines and molars in this study. The canines exhibited distal tipping and the molars exhibited mesial tipping on both sides. However, there was a significant difference in tipping per millimeter of retraction between the combined treatment side and the control side. It seems that slightly more bodily tooth movement was achieved on the combined treatment side. No comparisons could have been done for other studies that as they had no measurements of tipping/mm.
On both sides, the canines exhibited mesiobuccal rotation, while the molars underwent different rotations on the combined treatment side and the control side. The Roth tubes used in our study have a prefabricated distal offset which can produce the mesiobuccal rotation that was found on the control side. However, mesiopalatal rotation was observed on the combined treatment side. These differences in rotation between the two sides may be a result of individual patient variation. On both sides, individual differences were seen in almost all parameters that may be due to variation in bone density or the metabolic activities of bone and periodontium (PDL turnover speed). [18],[19],[20],[21],[22],[23]
| Conclusion | |  |
- The duration of canine retraction was reduced significantly in a 20% ratio by the corticotomy combined treatment.
- No difference was evident between the groups in terms of anchorage loss.
- Relatively more bodily tooth movement was achieved by corticotomy combined retraction.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
| References | |  |
| 1. | Suya H. Corticotomy in orthodontics. In: Hösl E, Baldauf A, editors. Mechanical and Biological Basics in Orthodontic Therapy. Heidel-berg, Germany: Hüthig Buch Verlag; 1991. p. 207-26.  |
| 2. | Gantes B, Rathbun E, Anholm M. Effects on the periodontium following corticotomy-facilitated orthodontics. Case reports. J Periodontol 1990;61:234-8.  |
| 3. | Anholm JM, Crites DA, Hoff R, Rathbun WE. Corticotomy-facilitated orthodontics. CDA J 1986;14:7-11.  |
| 4. | Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int J Periodontics Restorative Dent 2001;21:9-19.  |
| 5. | Aboul-Ela SM, El-Beialy AR, El-Sayed KM, Selim EM, El-Mangoury NH, Mostafa YA. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. Am J Orthod Dentofacial Orthop 2011;139:252-9.  |
| 6. | Echchadi Mel M. The role of alveolar corticotomies in orthodontic anchorage management. Int Orthod 2014;12:171-87.  |
| 7. | Oliveira DD, Oliveria BF, Soares RV. Alveolar corticotomies in orthodontics indications and effects on tooth movement. Dent Press J Orthod 2010;15:144-57.  |
| 8. | Wilcko MT, Wilcko WM, Breindel-Omniewski K, Bouquot JE, Wilcko JM. The periodontally ′accelerated osteogenic orthodontics′ (PAOO) technique: Efficient space closing with either orthopedic or orthodontic forces. J Implant Adv Clin Dent 2009;1:45-68.  |
| 9. | Mathews DP, Kokich VG. Accelerating tooth movement: The case against corticotomy-induced orthodontics. Am J Orthod Dentofacial Orthop 2013;144:5-13.  |
| 10. | Wilcko MT, Wilcko WM, Bissada NF. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: A synthesis of scientific perspectives. Semin Orthod 2008;14:305-16.  |
| 11. | Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol 1959;12:515-29.  |
| 12. | Leethanakul C, Kanokkulchai S, Pongpanich S, Leepong N, Charoemratrote C. Interseptal bone reduction on the rate of maxillary canine retraction. Angle Orthod 2014;84:839-45.  |
| 13. | Alikhani M, Raptis M, Zoldan B, Sangsuwon C, Lee YB, Alyami B, et al. Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop 2013;144:639-48.  |
| 14. | Abed SS, Al-Bustani AI. Corticotomy assisted orthodontic retraction. J Bagh Coll Dent 2013;25:160-6.  |
| 15. | Al-Naoum F, Hajeer MY, Al-Jundi A. Does alveolar corticotomy accelerate orthodontic tooth movement when retracting upper canines? A split-mouth design randomized controlled trial. J Oral Maxillofac Surg 2014;72:1880-9.  |
| 16. | Gjessing P. Biomechanical design and clinical evaluation of a new canine-retraction spring. Am J Orthod 1985;87:353-62.  |
| 17. | Gjessing P. A universal retraction spring. J Clin Orthod 1994;28:222-42.  |
| 18. | Reitan K. Biomechanical principles and reactions. In: Graber TM, Swain BF, editors. Orthodontics: Current Principles and Techniques. St. Louis: Mosby; 1985. p. 101-92.  |
| 19. | Champagne M. Reliability of measurements from photocopies of study models. J Clin Orthod 1992;26:648-50.  |
| 20. | Dincer M, Eroglu E, Uzuner FD. Are there any differences between the reactions to Gjessing′s PG canine retraction spring in the two jaws. Kieferorthopädie 2000;14:135-44.  |
| 21. | Ziegler P, Ingervall B. A clinical study of maxillary canine retraction with a retraction spring and with sliding mechanics. Am J Orthod Dentofacial Orthop 1989;95:99-106.  |
| 22. | Dahlberg G. Statistical Methods for Medical and Biological Students. New York: Interscience Publications; 1940.  |
| 23. | Itoh T, Nakajima M, Arita S, Nakagawa M, Kawagoe H, Fujita N, et al. Experimental study on the tooth movement with corticotomy procedure. Nihon Kyosei Shika Gakkai Zasshi 1981;40:92-105.  |
| 24. | Nakanishi H. Experimental study on artificial tooth movement with osteotomy and corticotomy (author′s transl). Shikwa Gakuho 1982;82:219-52.  |
| 25. | Ascher F. Zurspaetbehandlung der Prognathie des oberkiefers. Dtsch Zahnarztl Z 1947;2:218-26.  |
| 26. | Marcotte MR. Biomechanics in Orthodontics. St. Louis: Mosby; 1990.  |
| 27. | Dinçer M, Iscan HN. The effects of different sectional arches in canine retraction. Eur J Orthod 1994;16:317-23.  |
| 28. | Isik Aslan B, Balostuncer B, Dinçer M. Are there differences on tooth movement between different sectional canine retractors? J Orofac Orthop 2013;74:226-35.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1], [Table 2], [Table 3]
|