|


 |
| ORIGINAL ARTICLE |
|
| Year : 2011 | Volume
: 3
| Issue : 1 | Page : 23-30 |
|
|
Total laryngectomy for laryngeal cancer in a Nigerian tertiary health center: Prognosis and outcome
Kufre Iseh
Department of Otorhinolaryngology, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
| Date of Web Publication | 30-Mar-2011 |
Correspondence Address:
Kufre Iseh
Department of Otorhinolaryngology, Usmanu Danfodiyo University Teaching Hospital, Sokoto
Nigeria
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.78467

 Abstract Abstract | | |
Background: Advanced laryngeal cancers presenting with upper airway obstruction are a common scenario in Sub-Saharan Africa, requiring operative intervention as a priority. Objective: To assess outcome of total laryngectomy as a treatment option in the surgical management of advanced laryngeal cancers in a tertiary health institution in northwestern Nigeria. Materials and Methods: A retrospective analysis of total laryngectomies for laryngeal cancers carried out by one surgeon from December 2000 to August 2009. Results: Out of 30 patients with histologically diagnosed laryngeal cancer, 18 were treated with total laryngectomy Fourteen (77.8%) were males, while 4 (22.2%) were females, with a male-to-female ratio of 3.5:1. The age range was 20-70 years with a mean age of 47years for males and 33.8 years for females. Total laryngectomy was carried out on T4 lesions (100%), with preoperative tracheostomy (100%) carried out as an emergency measure to relieve upper airway obstruction. Two female patients had safe vaginal deliveries after their surgeries. Although all patients were referred for radiotherapy, only 6 (33.3%) patients could afford postoperative radiotherapy, with a 5-year survival rate of 33.3%; while all others could not afford the cost of radiotherapy treatment, which was to be carried out at a center about 5 hours drive away from our center. Seven (38.9%) patients presented with recurrent neck nodal disease, while 3 (16.7%) had carotid blow-out hemorrhage that was fatal. Conclusion: Total laryngectomy remains an important surgical modality of treatment for advanced laryngeal cancers, as it affords the patient an opportunity of longer survival when combined with postoperative radiotherapy. It is superior to 'radiotherapy only' or 'surgery only' or nothing. Keywords: Advanced laryngeal cancer, radiotherapy total laryngectomy, treatment options
How to cite this article:
Iseh K. Total laryngectomy for laryngeal cancer in a Nigerian tertiary health center: Prognosis and outcome. J Surg Tech Case Report 2011;3:23-30 |
How to cite this URL:
Iseh K. Total laryngectomy for laryngeal cancer in a Nigerian tertiary health center: Prognosis and outcome. J Surg Tech Case Report [serial online] 2011 [cited 2016 Jun 12];3:23-30. Available from: http://www.jstcr.org/text.asp?2011/3/1/23/78467 |
 Introduction Introduction | |  |
Laryngeal cancer is the most common head and neck cancer and the eleventh most common cancer in men worldwide but is relatively uncommon in women. [1],[2],[3],[4] The American Cancer Society estimated that about 11,300 new cases of laryngeal cancer were diagnosed in the year 2007 in the United States, which is about 1% of new cancers diagnosed, and approximately one third (3,660) of these patients would die of the disease. [1],[2]
The treatment of laryngeal cancers is usually planned to provide optimal survival free of disease with maximum functional results. [5] The treatment for T 1 and T 2 lesions usually involves radiotherapy or endoscopic surgery with or without lasers. [5],[6],[7] Total laryngectomy alone or in combination with neck dissection and/ or radiotherapy with or without chemotherapy is used for advanced T 3 and T 4 lesions. [5],[6],[7] Billroth in 1873 performed the first total laryngectomy; and for much of the 20 th century, it was recognized as the gold standard treatment for advanced cancer of the larynx and hypopharynx. [5],[6]
One major difference in the Sub-Saharan Africa region is the late presentation, which invariably affects both intervention measures and the prognosis. This is due to ignorance of the nature of the disease among all levels of workers of the health-care and non-health-care sectors. At presentation, the tumor is often in stages III and IV of the TNM classification of both International union against cancer (UICC) and American Joint committee against cancer (AJC) classification systems. [8] Total laryngectomy is usually the only meaningful intervention measure, followed by radiotherapy 6 weeks after the surgery.
The aim of this study was to assess total laryngectomy as one of the treatment options in the surgical management of advanced laryngeal cancers practiced at our center.
 Materials and Methods Materials and Methods | |  |
A retrospective analysis of all cases of total laryngectomy carried out by one surgeon from December 2000 to August 2009 in a tertiary health facility in northwestern Nigeria is hereby presented. Clinical indications, histological diagnosis, surgical technique, outcome and bio data were analyzed. Diagnosis of laryngeal cancer was based on history; physical examination, including flexible nasopharyngoscopy in some cases; direct laryngoscopy; and biopsy for histological diagnosis. Consent was obtained for surgery, with patients confirming having knowledge of permanent tracheostomy for life. Patients were referred for radiotherapy 6 weeks after surgery.
Surgical technique
Preoperative evaluation
Patients are usually investigated fully, such as full blood count, Erythrocyte sedimentation rate (ESR), electrolytes, urea and creatinine. Grouping and cross-matching of blood (2 units), screening for retroviral and hepatitis B surface antigen were routinely carried out. Chest x-rays and electrocardiogram (ECG) for patients older than 35 years were done. Preoperative informed consent, especially for permanent tracheostomy, was obtained. Computerized tomographic (CT) scan or magnetic resonance imaging (MRI) was not routinely carried out. Ideally the patient getting to meet a laryngectomee is the most desirable and encouraging to the patient. But this may not always be feasible in our environment due to different domicile backgrounds of the patients. Preoperative speech therapy is also ideal in preparation for esophageal speech.
Operative technique
The patient is placed supine, and neck is cleaned thoroughly with antiseptics, spirit and dried from the chin down to the chest at the nipple level. A nasogastric tube is passed into the pharynx not too far so as not to transplant any tumor further down. Some surgeons and some centers prefer carrying out a feeding gastrostomy 1 week before total laryngectomy. We routinely use the nasogastric (NG) tube for feeding. A decision needs to be taken whether or not to carry out neck dissection along with the total laryngectomy as this will determine the type of incision. Neck is infiltrated at the site of incision with xylocaine-adrenaline preparation (1%, 1:1000). A transverse incision or Gluck-Sorenson or modified Gluck-Sorenson incision may be used and deepened to sub-plastysmal layer [Figure 1]. A transverse incision is carried out at the level of 2-finger breadth above the sternum or at the level of cricoid cartilage, about 8-10 cm long. Gluck-Sorenson incision begins as a U-shaped incision starting from the angle of the mandible above to the level of the cricoids or thyroid gland, both incisions meeting at the midline. The upper skin flap is either stitched to the skin at the chin to allow freer access to the neck structures or retracted from the operation site [[Figure 2]a and b]. Strap muscles are separated in the midline laterally to expose the larynx and the thyroid gland, if they have not been infiltrated by the tumor. Any muscle infiltrated by tumor should be excised.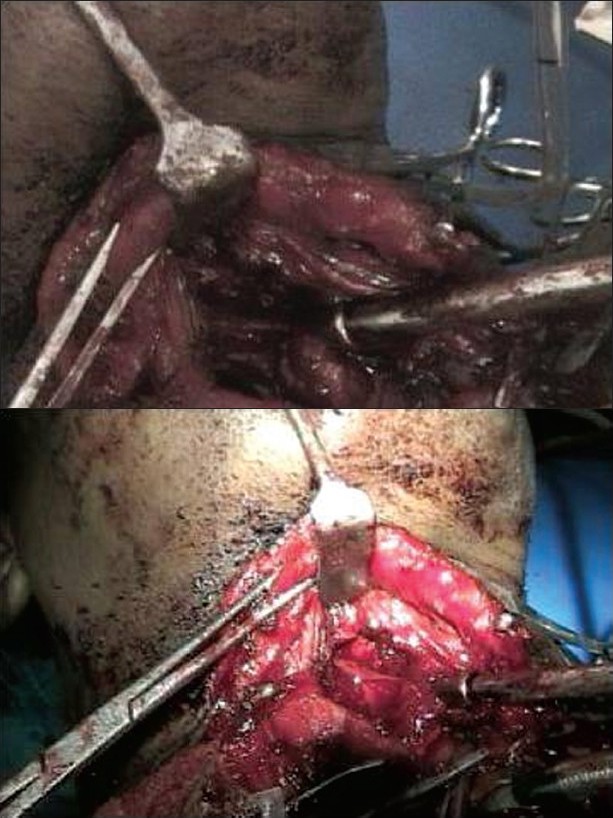 | Figure 2: (a)Neck-dissection total laryngectomy
Figure 2b: Neck-dissection total laryngectomy
Click here to view |
The thyroid gland is inspected to know which lobe will be preserved and which will be taken away with the specimen. The thyroid gland is then separated at the isthmus by ligation with 3/0 or 2/0 chromic catgut and division at the center. At this juncture, a permanent tracheostomy is carried out. The permanent tracheostomy stoma is created through a transverse stab skin wound on the lower skin flap, about 2-4 cm long. The trachea is transected from the cricoid cartilage with a scalpel blade of size 15 or 11; and using Allis tissue forceps, the trachea is pulled out through the stab wound and stitched to the skin after the endotracheal tube has been secured in the new tracheostomy. The permanent tracheostomy is carried out in two layers. The first layer is from subcutaneous tissue to the external layer of the trachea in interrupted fashion using either 3/0 or 4/0 absorbable sutures (chromic catgut), and the second layer is from mucosa to the skin using 3/0 nylon or nonabsorbable suture (nylon).
The larynx is delivered either from above to below or from below to above. If delivered from below, the larynx above the transected trachea is dissected free from the tracheo-esophageal groove along with the side of the thyroid gland to be removed taking special precaution to avoid the neurovascular bundles. Any visible lymph node (prelaryngeal, paratracheal, etc.) is carefully excised. The hypopharynx is entered on the side opposite to the site of the tumor after the muscles attached to the hyoid bone are divided. The epiglottis is grasped with tissue-grasping forceps after entry into the hypopharynx. Thereafter the whole specimen is removed along with the hyoid bone, epiglottis and the arytenoids. If the hypopharynx or upper esophagus is involved, then pharyngectomy or cervical esophagectomy is carried out. The pharynx is repaired either by direct mucosal closure if there is sufficient mucosa; or by using local or regional flaps or free and distant flaps after an appropriate sized nasogastric tube has been passed. Direct closure requires continuous mucosal closure with 3/0 chromic catgut either as a straight-line closure; or as a T closure, the horizontal arm of the T being at the base of the tongue at the pharyngeal inlet. The second layer is interrupted with the external covering of muscle layers with 3/0 catgut. Suturing must not be too tight to cause stenosis of the pharynx or too loose to avoid pharyngo-cutaneous fistula. A tracheoesophageal puncture (TEP) may be carried out and a Foleys catheter inserted if there are facilities for one-way valves for improved speech. A neck drain may be inserted but is optional to some surgeons. The skin is closed with nonabsorbable sutures [[Figure 3]a]. A neck dressing is applied. | Figure 3: (a)Immediate Post operative wound after total laryngectomy with endotracheal tube at the tracheostomy
Figure 3b: No leakage after testing with oral milk drink on 9th postoperative day
Click here to view |
Postoperative care
The patient is nursed head up with nil per oral for 9-12 days. Intravenous broad-spectrum antibiotics are prescribed based on the preference of the surgeon and the local antibiotic sensitivity pattern. Intravenous fluids are given as appropriate, along with routine analgesics for pain management. NG tube feeding is commenced 24 hours after surgery. The care of the tracheostomy tube is given appropriate attention. Materials are provided for written communication until the patient has acquired esophageal speech. Nasogastric tube feeding is continued for 9 to 12 days. On the 9 th or 10 th day, oral feeding is attempted with methylene blue or milk drink to see if there is leakage from the neck or wound site [[Figure 3]b]; if there is none, fluids are continued in graded fashion with the NG tube in place; and if after 24 hours there is still no leakage, the NG tube is removed. Graded fluid-form high-protein diet is continued for 1 week before semisolids are commenced in a graded manner before introduction of solids. At our center, local high-protein foods are blended to fluid form after being thoroughly cooked, such as beans and beans products, fish, boiled eggs and all kinds of fruits and some carbohydrates. Drugs are usually given crushed through the NG tube 48 hours after surgery. Stitches are removed on the sixth to seventh postoperative day. If there is any pharyngo-cutaneous fistula, oral feeding is suspended and NG tube feeding is continued for a while to allow closure of the fistula. If the fistula persists for 2 months, reconstructive procedures may be carried out with pectoralis major myocutaneous flap or any flap based on the preference of the surgeon and the circumstances surrounding the patient. Patient is referred for postoperative radiotherapy, generally 6 weeks after surgery [Figure 4]. Electrolarynx, where facilities are available, may be used to improve speech, but at our center we rely mainly on acquisition of esophageal speech.
 Results Results | |  |
A total number of 18 (60%) patients underwent total laryngectomies for advanced laryngeal cancers out of the 30 cases of histologically confirmed laryngeal cancers during the same period (26 males, 4 females; M-F ratio, 6.5:1). Twelve (40%) patients declined total laryngectomy, preferring either no further intervention or radiotherapy. One patient who opted for radiotherapy returned with very unsatisfactory results and eventually succumbed to the disease within 1 year [Figure 5]. Others were lost to follow-up. | Figure 5: Neck node recurrence in a patient who declined postoperative radiotherapy
Click here to view |
Clinical features and indications for total laryngectomy
All were transglottic tumors (T3 and T4) that presented with upper airway obstruction as emergencies at either the Accident and Emergency Department or the ENT outpatient clinic [[Figure 6]a and b]. Hoarseness of voice was another common clinical symptom for a variable period (3 months to 1 year). Dysphagia for advanced lesions to the hypopharynx or cervical esophagus was a clinical feature in 10 (55.6%) patients. | Figure 6: (a)Postoperative transglottic laryngeal specimen
Figure 6b: Postoperative transglottic laryngeal specimen
Click here to view |
Sex and age
Out of the 18 operated patients, 14 (77.8%) were males while 4 (22.2%) were females, with a male-to-female ratio of 3.5:1. The age range for both males and females was 20-70 years with a mean age of 47 years. For males the age range was 30-70 years (mean, 50.8 years); while for females, age range was 20-50 years (mean, 33.8 years approximately). Females therefore had laryngeal cancer at an earlier age than males.
Alcohol and cigarette smoking
All male patients had a positive history of heavy cigarette smoking. None of the females smoked but were wives to chain smokers. None had positive history of alcohol ingestion. Alcohol consumption amongst the indigenous population is not very common in this region.
Occupation
All female patients were housewives with no occupational exposure to injurious chemicals or agents. For the males, none was exposed to known carcinogenic agents. Most were farmers except 1, who was a retired soldier.
Histology
All (100%) cases were of squamous cell carcinoma.
Preoperative tracheostomy
This was carried out on all (100%) patients due to upper airway obstruction that presented as an emergency.
Method of pharyngeal closure
Direct mucosal closure was carried out in 15 (83.3%) patients; full-thickness skin graft, in 3 (16.7%); and pectoralis major myocutaneous flap, in 1 (5.6%) patient.
Immediate postoperative feeding method
NG tube was used in 16 (88.9%) patients, while feeding gastrostomy was carried out in 2 (11.1%) patients.
Outcome
- A. ComplicationPharyngocutaneous fistula: There were 3 (16.7%) cases of pharyngocutaneous fistula. These were patients who had lesions advanced beyond the larynx. Two patients were managed conservatively, while 1 patient required pectoralis major myocutaneous flap closure.
- Carotid "blow-out" hemorrhage: Three (16.7%) patients had carotid blow-out hemorrhage; all the 3 cases were fatal. One of these cases occurred 4 years after total laryngectomy and radiotherapy (the other 2 cases occurred within 6 months and 2 years, respectively, after total laryngectomy), with recurrence; these patients did not opt for radiotherapy. These were patients that reported back to the teaching hospital. We do not have adequate access to other patients, who are living in remote areas without any communication facilities.
- Pharyngeal stenosis: This was found in 1 (5.6%) patient requiring dilatation.
- Nodal recurrence after total laryngectomy: A total of 7 (38.9%) patients presented with nodal recurrence after total laryngectomy. After total laryngectomy and radiotherapy, for lesions without palpable cervical lymph nodes, or neck mass, recurrence in the form of neck mass usually appeared between 4 and 7 years of disease-free interval (1 case, within 4 years). With only total laryngectomy without follow-up radiotherapy, recurrence of neck or nodal lesion occurred in the period varying from 1 year to 2½ years (6 cases, 33.3%).
Survival
The longest survival period after total laryngectomy and postoperative radiotherapy in this study without nodal recurrence so far is 7 years, and the patient is still alive. Only 6 (33.3%) patients were able to attain a minimum disease-free period of 4-7 years with follow-up radiotherapy; while the rest, who did not follow up with radiotherapy, eventually succumbed to recurrent disease within 2½ years.
 Discussion Discussion | |  |
Total laryngectomy in this study was carried out in cases of advanced laryngeal cancers, which were all transglottic in the much younger age group (range, 20-70 years; mean, 47 years); the corresponding age group for total laryngectomy in the Leeds Teaching Hospital, UK, is 41-82 years. [2],[5] These were patients who presented with upper airway obstruction necessitating emergency tracheostomies to save life. The most important adverse prognostic factors for laryngeal cancers include increasing tumor (T) stage and nodal (N) stage. Other prognostic factors may include sex, age, performance status and a variety of pathologic features of the tumor, including grade and depth of invasion. [9] Prognosis for small laryngeal cancers that have not spread to lymph nodes is very good, with cure rates of 75% to 95% depending on the site, tumor bulk, and degree of infiltration. [10] Although most early lesions can be cured by either radiation therapy or surgery, radiation therapy may be a reasonable choice to preserve voice, leaving surgery for salvage [11] because at our center, laryngeal cancers present late; some patients with fungating anterior neck lesions hardly have any other option than total laryngectomy with follow-up radiotherapy to prolong life. This trend is in contrast to that in the western world, where T1, T2 lesions are generally detected early and appropriate intervention measures are carried out and cure is achieved.
Although the 5-year survival in this study is quite low when compared to several reports, performing total laryngectomy in these patients is significant. It afforded the patients a better opportunity for improved living, namely, swallowing and oral feeding, absence of difficulty in breathing, absence of unsightly neck swelling. Two out of the 4 female patients conceived and delivered normally before succumbing to the disease. But regrettably not all availed themselves the opportunity for postoperative radiotherapy, which prolonged survival (in 33.3% of the cases) when compared to cases wherein no radiotherapy (66.7% of the cases) was carried out. Poverty and ignorance are reasons cited for late presentation. For example, all patients received one form of treatment for upper respiratory tract infection and for bronchial asthma for a variable period until severe respiratory distress set in before being referred for emergency tracheostomy. Some patients could not afford postoperative radiotherapy; that were located at a distance of about 5 hours drive from our center. Lilly-Tariah et al. found a recurrence rate of 47.5% within 9 months of total laryngectomy without a follow-up radiotherapy, in Jos, middle belt of Nigeria; they found this operation to be unsatisfactory without a follow-up radiotherapy. [12] The study by Somefun et al. revealed a higher rate of radiotherapy (86%) in Lagos, southwestern part of Nigeria, with poor outcome. [13] They reported 4-year survival in only 1 patient post radiotherapy but did not state the T level out of the 36 patients reviewed.
Patients with a pre-radiation hemoglobin level higher than 13 g/dL have higher local control and survival rates than patients who are anemic. [14] This observation is being evaluated in a randomized clinical trial. At our center, the patients in general were not healthy. Some were anemic and malnourished, with other comorbid disorders. These patients had to be certified fit for any elective operation. There was therefore a variable period between the time of the emergency tracheostomy and definitive surgery. This delay was not a healthy development for malignant cases as tracheostomy is well known to cause local spread of malignant lesions without definitive surgery and therefore to worsen the prognosis.
Early diagnosis, flexible nasopharyngolaryngoscopy, early tissue biopsy and prompt treatment with lasers, endoscopic resection, radiotherapy at centers abroad with such facilities, along with chemotherapy, photodynamic therapy and targeted gene therapy, have greatly improved survival in well-developed centers with adequate facilities. [1],[2],[3],[4],[5],[9],[10],[11] Absence of these facilities remains a major challenge in the Sub-Saharan Africa regions; and total laryngectomy, coupled with pharyngeal reconstruction, becomes a major concern to address. [15] Selective neck dissection was carried out along with the total laryngectomy. No radical or functional neck dissection was carried out. The evidence provided by the Brazilian Head and Neck Cancer Study Group favors selective neck dissection for laryngeal cancer as opposed to radical or functional neck dissection. [16]
In Nigeria, laryngeal cancer has been reported as the second most common otolaryngological cancer in Usmanu Danfodiyo University Teaching Hospital, located in northwestern Nigeria; and in Lagos University Teaching Hospital, in southwestern Nigeria. [17],[18] However, it is the third most common cancer in the otolaryngological clinic in University College Hospital, Ibadan, and the sixth most common cancer in Ibadan. [19] Laryngeal cancer is the third most common cancer in the ENT clinic of University of Maiduguri Teaching Hospital, located in northeastern Nigeria; second most common ENT cancer and fifth most common head and neck cancer in Jos University Teaching Hospital, located in north central Nigeria. [20],[21],[22] Laryngeal cancer has also been reported as the third most common cause of hoarseness among adult Nigerians in Lagos and in Enugu in southeastern Nigeria. [23],[24] Therefore, total laryngectomy will continue to be a major challenge to address in the treatment of laryngeal cancers as long as late presentation is the trend in Sub-Saharan Africa. It must be acknowledged that the 18 (60%) patients so far operated were the ones who accepted operative intervention, which is the basis of this study. Some (40%) declined any further surgery after a tracheostomy was carried out to relieve upper airway obstruction. Some declined tracheostomy and died at home. Some accepted direct laryngoscopy and biopsy but preferred radiotherapy to surgery, which they either did not opt for or could not complete the full course of this treatment. Non-acceptability of permanent tracheostomy accounted for high rejection rate for total laryngectomy. Total laryngectomy was carried out without voice- or speech-improving procedures such as tracheoesophageal puncture (TEP). There were no facilities for electrolarynx. Only esophageal speech was developed in these patients. Testing for postoperative pharyngocutaneous fistula was done mainly with milk drink, and this has been found effective not only at our center but also by other researchers. [25] The recent setting up of a radiotherapy unit at our center will hopefully address the issue of traveling long distances and will encourage more patients to avail themselves of this treatment at an affordable rate, and more patients will survive longer than the present trend.
Currently laryngeal transplant is advocated for patients of total laryngectomy who had postoperative radiotherapy, with a 5-year disease-free period following the success of the first laryngeal transplant in Cleveland, Ohio, USA, in 1998 for traumatic injury to the larynx with laryngeal stenosis. [26],[27] No center has yet done this in the entire world, and this may be very difficult to achieve in this environment due to several mitigating factors.
In conclusion, total laryngectomy in combination with postoperative radiotherapy affords a longer period of survival for patients of advanced laryngeal cancers as compared to radiotherapy alone or total laryngectomy alone or no treatment.
 References References | |  |
| 1. | Birchall MA, Pope L. Tumours of the larynx. In: Gleeson M, Browning GG, Burton MJ, Clarke R, editors. Scott-Brown′s Otorhinolaryngology, Head and Neck Surgery. 7 th ed. Vol 2. London: Hodder Arnold; 2008. p. 2598-622. 
|
| 2. | Watkinson JC, Gaze MN, Wilson JA. Tumours of the larynx. In Stell and Maran′s Head and Neck Surgery. 4 th ed. Oxford: Butterworth-Heinemann; 2000. p. 233-73. 
|
| 3. | American Cancer Society. Cancer Facts and Figures 2007. Atlanta, GA: American Cancer Society; 2007. 
|
| 4. | Concus AP. Malignant laryngeal lesions. In: Lalwani AK, editor. Current Diagnosis and Treatment in Otolaryngology-Head and Neck Surgery. New York: Lange; 2004. p. 455-73. 
|
| 5. | Bajay Y, Shayah A, Sethi N, Harris AT, Bhatti I, Awobem A, et al. Clinical outcomes of total laryngectomy for laryngeal carcinoma. Kathmandu Univ Med J 2009;7:258-62. 
|
| 6. | Johnson JT, Myers EN, Hao S, Wagner RL. Outcome of open surgical therapy for glottis carcinoma. Ann Otol Rhinol Laryngol 1993;102:752-5. 
|
| 7. | Hall FT, O′Brien CJ, Clifford AR, McNeil EB, Bron L, Jackson MA. Clinical outcome following Total Laryngectomy for cancer. Aust N Z J Surg 2003;73:300-5. 
|
| 8. | Sobin LH, Wittekind CH. UICC-AJC TNM classification of malignant tumours. New York: Willey and Sons; 2002. 
|
| 9. | Yilmaz T, Hoºal S, Gedikoglu G, Turan E, Ayas K. Prognostic significance of depth of invasion in cancer of the larynx. Laryngoscope 1998;108:764-8. 
|
| 10. | Reddy SP, Mohideen N, Marra S, Marks JE. Effect of tumor bulk on local control and survival of patients with T1 glottic cancer. Radiother Oncol 1998;47:161-6. 
[PUBMED] [FULLTEXT] |
| 11. | National cancer institute. Available from: http://www.cancer.gov/cancertopics/pdq/treatment/laryngeal/HealthProfessional/page2. [Last accessed on 2010 June 15]. 
|
| 12. | Da-Lilly-Tariah OB, Somefun OA. Outcome of total laryngectomy in the treatment of cancer of the larynx in the middle belt plateau of Nigeria. Nig J Surg 2002;2:35-9. 
|
| 13. | Somefun OA, Nwawolo CC, Okeowo PA, Alabi SB, Abdulkareem FB, Banjo AF, et al. Prognostic factors in the Management outcome of carcinoma of the larynx in lagos. Nig Postgrad Med J 2003;10:103-6. 
|
| 14. | Fein DA, Lee WR, Hanlon AL, Ridge JA, Langer CJ, Curan WJ, et al. Pretreatment hemoglobin level influences local control and survival of T1-T2 squamous cell carcinomas of the glottic larynx. J Clin Oncol 1995;13:2077-83. 
|
| 15. | Iseh KR, Legbo JN. Pharyngeal reconstruction after total laryngectomy:options in a developing country. Nig J Plast Reconst Surg 2009;5:2-7. 
|
| 16. | Brazilian Head and Neck Cancer Study Group. End results of a prospective trial on elective lateral neck dissection vs type 111 modified radical neck dissection in the management of supraglottic and transglottic carcinomas. Head and Neck 1999;21:694-702. 
[PUBMED] [FULLTEXT] |
| 17. | Iseh KR, Malami SA. Patterns of head and neck cancers in sokoto. Niger J Otolaryn 2006;3:77-83. 
|
| 18. | Nwawolo CC, Ajekigbe AT, Oyeneyin JO, Nwankwo KC, Okeowo PA. Pattern of head and neck cancers among Nigerians in Lagos. West Afr J Med 2001;20:111-6. 
[PUBMED] |
| 19. | Nwaorgu OG, Onakoya PA, Usman MA, Abdu A. Laryngeal carcinoma: clinical features seen at University college hospital Ibadan. Trop Doct 2002;32:236-7. 
[PUBMED] |
| 20. | Ahmad BM, Pindiga UH. Malignant neoplasms of the ear, nose and throat in North eastern Nigeria. Highland Med Res J 2004;2:45-8. 
|
| 21. | Lilly-Tariah OB, Nwana EJ, Okeowo PA. Cancer of ear, nose and throat. Niger J Surg Sci 2000;10:52-6. 
|
| 22. | Bhatia PI. Head and neck cancer in plateau state. West Afr J Med 1990;9:304-10. 
|
| 23. | Okeowo PA. Hoarseness in Nigerians. Nig Med J 1976;7:458-60. 
|
| 24. | Okafor BC. Otolaryngology in South Eastern Nigeria II. Pattern of Throat diseases. Nig Med J 1983;1:31-41. 
|
| 25. | Galli J, Valenza V, Parrilla C, Galla S, Marchese MR, Castaldi P, et al. Pharyngocutaneous fistula onset after total laryngectomy: Scintigraphic analysis. Acta Otorhinolaryngol Ital 2009;29:242-4. 
[PUBMED] [FULLTEXT] |
| 26. | Strome M, Stein J, Esclamado R, Hicks D, Lorenz RR, Braun W, et al. Laryngeal transplantation and 40-month follow-up. N Engl J Med 2001;344:1676-9. 
[PUBMED] [FULLTEXT] |
| 27. | Birchall MA, Lorenz RR, Berke GS, Genden EM, Haughey BH, Siemionow M, et al. Laryngeal Transplantation in 2005: A Review. Am J Transplant 2006;6:20-6. 
[PUBMED] [FULLTEXT] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6]
|