|


 |
| LETTER TO EDITOR |
|
| Year : 2013 | Volume
: 5
| Issue : 1 | Page : 60-61 |
|
|
Unusual cause of shock: inferior vena cava obstruction complicating pyogenic liver abscess
Debajyoti Mohanty1, Pankaj Kumar Garg1, Bhupendra Kumar Jain1, Shuchi Bhatt2
1 Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi - 110 095, India
2 Department of Radiology, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi - 110 095, India
| Date of Web Publication | 21-Sep-2013 |
Correspondence Address:
Pankaj Kumar Garg
Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi - 110 095
India
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.118635

How to cite this article:
Mohanty D, Garg PK, Jain BK, Bhatt S. Unusual cause of shock: inferior vena cava obstruction complicating pyogenic liver abscess. J Surg Tech Case Report 2013;5:60-1 |
How to cite this URL:
Mohanty D, Garg PK, Jain BK, Bhatt S. Unusual cause of shock: inferior vena cava obstruction complicating pyogenic liver abscess. J Surg Tech Case Report [serial online] 2013 [cited 2016 May 25];5:60-1. Available from: http://www.jstcr.org/text.asp?2013/5/1/60/118635 |
Sir,
A 10-year-old boy presented with pain in right hypochondrium, continuous high-grade fever, and dry cough for 10 days. He did not report to have jaundice or altered bowel movements. He was febrile, having pulse rate of 110 beats/min, blood pressure of 86/66 mmHg, and bilateral pedal edema. Abdominal examination revealed enlarged tender hepatomegaly (liver span 15 cm) and positive shifting dullness for free fluid in peritoneal cavity. Hematological investigations revealed hemoglobin of 8.8 g/dL and white blood cells count of 8600/mm 3 . The biochemical investigations showed blood urea of 48 mg/dL and serum creatinine of 1.2 mg/dL. Liver functions tests showed a total bilirubin of 1.3 mg/dL, serum alkaline phosphatase of 248 IU/L (normal range, 40-280 IU/L), aspartate aminotransferase 38 IU/L, and alanine aminotransferase 42 IU/L. Chest roentgenogram showed blunting of right costophrenic angle suggestive of right pleural effusion. Ultrasonography (USG) of the abdomen revealed an enlarged liver containing an area of altered echotexture appearing heterogeneously hypoechoic with well defined margins involving the segment IV, VII, VIII, and II liver. The lesion measured approximately 1000 mL in volume and was seen to compress the 7 cm long segment of infrahepatic inferior vena cava (IVC). Color Doppler showed minimal low velocity flow within the compressed segment of IVC (anteroposterior diameter of 3 mm) [Figure 1]a. The IVC proximal to compression demonstrated monophasic slow flow with loss of normal phasic variation (anteroposterior diameter of 7 mm). The hepatic veins confluence was seen of normal size, and with normal color and Doppler signals. The intra hepatic biliary radicals were not dilated. The liver lesion also caused displacement and minimal compression of the right portal vein. There was mild right pleural effusion and ascites as well. A diagnosis of right lobe liver abscess was made and urgent USG-guided aspiration was undertaken. Only 15-20 mL of thick pus could be aspirated, which was thick, creamy, and brownish in color. Microscopic examination of the pus showed Gram positive cocci in groups but it did not grow any organism on culture. The patient was prescribed broad spectrum antibiotics. However, the hypotension was not responding to fluid challenge as well as to vasopressors. Therefore, he underwent exploratory laparotomy and open drainage of the abscess cavity. Postoperatively, the vasopressors were weaned off on second postoperative day. The abdominal drain was removed on third postoperative day. Repeat ultrasound Doppler examination done on fourth postoperative day showed decrease in the abscess cavity size as well as compression effect on IVC [Figure 1]b. The patient was discharged on 11 th postoperative day in stable condition. He is well on routine follow up after 1 year.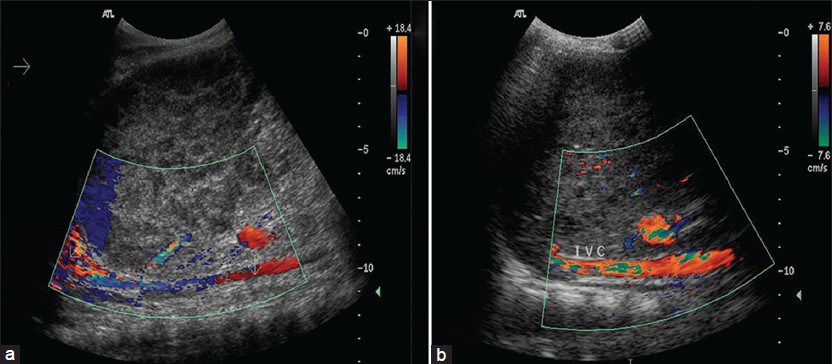 | Figure 1: Ultrasound color Doppler examination; (a) Space occupying liver lesion compressing the infra hepatic part of inferior vena cava and (b) Smaller liver lesion with a patent inferior vena cava following surgical drainage
Click here to view |
Pyogenic liver abscess usually presents with high grade pyrexia with chills, pain in right hypochondrium, and tender hepatomegaly. Presence of hypotension in a patient of liver abscess should raise the suspicion of septicemic shock, peritonitis and massive pleural effusion secondary to rupture, and rarely IVC obstruction decreasing the venous return to the heart. [1],[2]
Thrombus formation and extrinsic compression are the two mechanisms that cause hepatic venous outflow/IVC obstruction in patients of liver abscess. The clinical picture depends on whether the compression is complete or incomplete. Patients having complete obstruction have a fulminant course with high mortality. In the present case, the course was not fulminant due to incomplete obstruction. However, our patient presented with shock that resulted from decreased preload (venous return) due to IVC obstruction due to large liver abscess. This is further evident by the fact that his blood pressure improved following drainage of the abscess resulting in increased venous return.
Children with liver abscess are more prone to develop this complication as they have a relatively small liver tissue mass thus putting the IVC at a greater risk of being compressed by a large abscess. The location of the abscess on USG appears to be more important than its volume or size as a large abscess in the vicinity of IVC is more likely to compress it than the one away from it. [2] Diagnosis can be confirmed with Doppler (sensitivity of 85-95% [3] ) by demonstrating the reduced IVC/hepatic vein caliber and flow.
Since this condition is associated with a high mortality, [4] early intervention is mandatory and can be life saving. Percutaneous aspiration under USG guidance should be carried out complemented with broad spectrum antibiotic therapy. Open surgical drainage, as in this case, is indicated in the event of failure of percutaneous aspiration due to organized pus or inaccessibility, multiple abscess cavities, and ascites due to intraperitoneal rupture. [5] Recognizing IVC obstruction as a cause of shock in patients with liver abscess is essential for effective management of this potentially life threatening condition.
 References References | |  |
| 1. | Schmid BD, Lalyre Y, Sigel B, Kiani R, Layden TJ. Inferior vena cava obstruction complicating amebic liver abscess. Dig Dis Sci 1982;27:565-9. 
[PUBMED] |
| 2. | Sharma MP, Sarin SK. Inferior vena caval obstruction due to amoebic liver abscess. J Assoc Phys India 1982;30:243-4. 
|
| 3. | Valla DC. Hepatic vein thrombosis (Budd Chiari syndrome). Semin Liver Dis 2002;22:5-14. 
[PUBMED] |
| 4. | Zeitoun G, Escolano S, Hadengue A, Azar N, El Younsi M, Mallet A, et al. Outcome of Budd Chiari syndrome: A multivariate analysis of factors related to survival including surgical portosystemic shunting. Hepatology 1999;30:84-9. 
[PUBMED] |
| 5. | Strong RW. Pyogenic liver abscess. In: Blumgart LH, editor. Surgery of the liver, biliary tract and pancreas. Philadelphia: Saunders Elsevier; 2007. p. 927-34. 
|
[Figure 1]
|