|


 |
| SURGICAL DEBATE |
|
| Year : 2014 | Volume
: 6
| Issue : 1 | Page : 39-42 |
|
|
Treatment of pseudoarthrosis after minimally invasive hallux valgus correction
Marco Cianforlini, Cristina Rosini, Mario Marinelli, Luigi de Palma
Department of Orthopaedic, Clinical Orthopaedics, School of Medicine, Universitą Politecnica delle Marche, Ospedali Riuniti, Ancona, Italy
| Date of Web Publication | 24-Jun-2014 |
Correspondence Address:
Marco Cianforlini
Clinical Orthopaedics, School of Medicine, Universitą Politecnica delle Marche, Ospedali Riuniti, via Conca 71/60126, Ancona, Marche
Italy
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.135153

 Abstract Abstract | | |
Objective: Treatment of mild and moderate hallux valgus deformities. Discussion: Minimally invasive technique enables surgeons to treat mild and moderate hallux valgus deformities with excellent and good results in the majority of patients. Nonunion of first metatarsal, moreover, has only rarely been reported. Summary: We describe the essential steps of a surgical technique for the treatment of nonunions after miniinvasive subcapital first metatarsal osteotomy reconstructed using a tricortical iliac crest bone graft. Keywords: Bone graft, hallux valgus, miniinvasive, osteotomy, pseudoarthrosis
How to cite this article:
Cianforlini M, Rosini C, Marinelli M, de Palma L. Treatment of pseudoarthrosis after minimally invasive hallux valgus correction. J Surg Tech Case Report 2014;6:39-42 |
How to cite this URL:
Cianforlini M, Rosini C, Marinelli M, de Palma L. Treatment of pseudoarthrosis after minimally invasive hallux valgus correction. J Surg Tech Case Report [serial online] 2014 [cited 2016 May 10];6:39-42. Available from: http://www.jstcr.org/text.asp?2014/6/1/39/135153 |
 Introduction Introduction | |  |
Minimally invasive subcapital osteotomy of the first metatarsal is indicated for correction of mild to moderate hallux valgus deformities with a valgus angle (HVA) ≤40° and an intermetatarsal angle (IMA) of 10-20°. A Kirschner wire is used to help guide and stabilize the correction. The osteotomy is performed through a 3-5 mm incision using a corticotomy technique and no associated soft tissue procedures. Advantages include shorter operation time and hospital stay, fewer complications, and earlier weight-bearing. [1]
Giannini et al., [2] reported the outcomes and 36-month follow-up data (range: 22-52 months) of the first 54 consecutive feet treated with their minimally invasive simple, effective, rapid, and inexpensive technique. They measured HVA, IMA, and distal metatarsal articular angle on the x-rays before and after the operation. All but four patients (7.4%) were satisfied with their outcome. The postoperative clinical evaluation, based on the American Orthopedic Foot and Ankle Society (AOFAS) score, gave a mean score of 81, with 64.8% excellent results (35 feet), 18.5% good results (10 feet), 9.2% fair results (5 feet), and 7.4% poor results (4 feet). All osteotomies healed well, with radiographic evidence of callus formation after an average of 3 months. Remodeling was documented for all metatarsal bones, including those exhibiting marked offset at the time of osteotomy. [3] Magnan et al., described the results of 118 consecutive percutaneous subcapital distal osteotomies (82 patients; mean follow-up 35.9 months) for mild to moderate hallux valgus deformity and reported a mean AOFAS score of 88.2 ± 12.9. Complications included three recurrent valgus deformities (2.5%), eight stiff first metatarsophalangeal joints (6.8%), and a deep infection that resolved with antibiotic therapy (0.8%). The majority of patients (91%) were satisfied with the operation.
A large body of data supports the claim that minimal access techniques enable correction of 80-90% of hallux valgus deformities solely via hallux manipulation without removal of the eminence or open lateral release yielding more than 90% excellent and good results. [2],[4],[5] Nonunion is rarely reported. We describe our operative technique for nonunion following minimally invasive subcapital osteotomy of the first metatarsal [Figure 1]a and b]. | Figure 1: Computed tomography: Axial (a) and Sagittal (b) Scans documenting the nonunion site after subcapital osteotomy of the first metatarsal
Click here to view |
 Discussion Discussion | |  |
The procedure involves the use of a tricortical iliac crest autograft to restore the length of the first metatarsal and its proportion to the lesser metatarsals, aligning the center of the first and second metatarsal heads so that they lie on the same line.
The patient is placed supine, with a small sandbag under the pelvis. The donor site on the ipsilateral iliac crest and the site of the miniincision on the dorsomedial aspect of the foot are marked with a surgical pen. The two operative fields are then are separately prepared and draped. A tourniquet is applied at mid thigh.
The miniincision is performed and the nonunion site is cleared and identified [Figure 2]a]. Possible scar tissue from the previous procedure may prevent adequate visualization of the dorsal nerve. The dissection should not extend to the lateral aspect of the first metatarsal head, to avoid potential injury to the vascular supply of the distal stump. The proximal and distal stump are gently curetted to obtain two concave surfaces that will accommodate the graft. The diaphyseal canal is cleaned of fibrous tissue and reamed to host the proximal peg.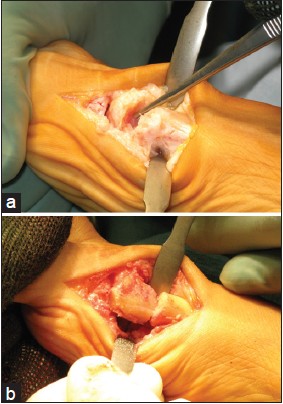 | Figure 2: Intraoperative photographs: (a) Nonunion site (b) The proximal peg is inserted into the metatarsal shaft
Click here to view |
The bone graft is harvested. Graft preparation is a key step. The tricortical autograft measures between 20 and 35 mm, depending on the bone length to be restored. Cortical bone is removed on two sides, exposing the trabecular bone [Figure 2]b]. The graft is then shaped to fit the surfaces of the proximal and distal stump [Figure 3]a and b] firmly inserted and finally fixed with a 3.5 mm compression screw from medial proximal to distal lateral [Figure 4]a and b].
Graft size is designed to obtain maximal hallux lengthening without impairing wound closure or the vascular supply to the toe. Tenotomy may be required to correct the length of the extensor digitorum longus of the first ray. A regional popliteal nerve block may be applied during admission and removed before discharge.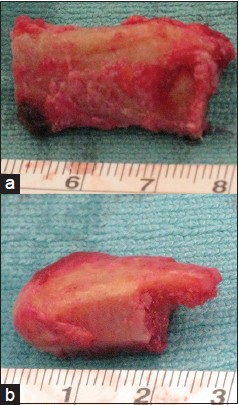 | Figure 3: Intraoperative photographs: The graft (a) Before and (b) After modeling
Click here to view |
 | Figure 4: Plain radiographs: Postoperative anteroposterior and oblique views of the proximal peg firmly fitted into the metatarsal shaft
Click here to view |
The patient is discharged on the 2 nd or 3 rd postoperative day. A short leg cast is applied for 12 weeks and walking is allowed after its removal. Low molecular weight heparin (4000 IU/day) is given for 12 weeks. Radiographs are taken at 4 weeks and 3 and 6 months [Figure 5]a and b], until radiographic healing is documented. | Figure 5: Plain radiographs: Weight-bearing (a) and Lateral (b) Views documenting graft viability
Click here to view |
 Summary Summary | |  |
The surgical procedure can be summarized into five steps which are as follows:
- Dorsomedial incision and identification of nonunion site [Figure 6]a and b]
- Curetting of nonunion site to obtain two concave surfaces that will accommodate the graft [Figure 7]a and b]
- Collection of an ipsilateral iliac crest tricortical autograft measuring 20-35 mm [Figure 8]
- Graft fashioning, with a convex distal surface and a small proximal peg [Figure 9]
- The peg is firmly inserted into the metatarsal shaft and the graft is fixed with a 3.5 mm compression screw from medial proximal to distal lateral [Figure 10].
 | Figure 10: The proximal peg is shaped for firm placement into the metatarsal shaft and the graft is fixed with a 3.5 mm compression screw from medial proximal to distal lateral
Click here to view |
 References References | |  |
| 1. | Lin JS, Bustillo J. Surgical treatment of hallux valgus: A review. Curr Opin Orthop 2007;18:112-7. 
|
| 2. | Giannini S, Ceccarelli F, Bevoni R, Vannini F. Hallux valgus surgery: The minimally invasive bunion correction (SERI). Tech Foot Ankle Surg 2003;2:11-20. 
|
| 3. | Magnan B, Pezzè L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. J Bone Joint Surg Am 2005;87:1191-9. 
|
| 4. | Giannini S, Faldini C, Vannini F, Digennaro V, Bevoni R, Luciani D. The minimally invasive osteotomy "S.E.R.I." (Simple, effective, rapid, inexpensive) for correction of bunionette deformity. Foot Ankle Int 2008;29:282-6. 
|
| 5. | Lin YC, Cheng YM, Chang JK, Chen CH, Huang PJ. Minimally invasive distal metatarsal osteotomy for mild-to-moderate hallux valgus deformity. Kaohsiung J Med Sci 2009;25:431-7. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10]
|