|


 |
| CASE REPORT |
|
| Year : 2014 | Volume
: 6
| Issue : 2 | Page : 64-66 |
|
|
Pediatric thymoma with a difference: Report of a case and review of literature
Sudipta Saha1, Suhani Suhani1, Animesh Basak2, Nitin Agarwal2, Pooja Dewan3
1 Department of Surgery, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India
2 University College of Medical Sciences and Guru Tegh Bahadur Hospital, New Delhi, India
3 Department of Paediatrics, University College of Medical Sciences and Guru Tegh Bahadur Hospital, New Delhi, India
| Date of Web Publication | 18-Dec-2014 |
Correspondence Address:
Sudipta Saha
Department of Surgery, Lady Hardinge Medical College and Associated Hospitals, New Delhi
India
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.147263

 Abstract Abstract | | |
Thymoma represents <1% of all mediastinal tumors in children. Less than 50 cases of pediatric thymoma are reported in the literature. Thymomas are considered to be highly aggressive in pediatric patients, especially when age is <10 years. Paraneoplastic syndromes, of which around 70% are myasthenia gravis, correlate with poor prognosis. In this article, we report a case of a thymoma in an 8-year-old boy, who had favorable histopathology (Masaoka stage I, WHO type B2), despite the presence of young age and necrosis along with absence of myasthenia gravis. We have also reviewed the available literature on pediatric thymoma. Keywords: Masaoka, mediastinum, myasthenia gravis, thymoma
How to cite this article:
Saha S, Suhani S, Basak A, Agarwal N, Dewan P. Pediatric thymoma with a difference: Report of a case and review of literature
. J Surg Tech Case Report 2014;6:64-6 |
How to cite this URL:
Saha S, Suhani S, Basak A, Agarwal N, Dewan P. Pediatric thymoma with a difference: Report of a case and review of literature
. J Surg Tech Case Report [serial online] 2014 [cited 2016 May 10];6:64-6. Available from: http://www.jstcr.org/text.asp?2014/6/2/64/147263 |
 Introduction Introduction | |  |
Thymomas are lympho epithelial neoplasm characterized by admixture of epithelial cells and mature lymphocytes. In adults, thymoma is the most common primary tumor of the anterior mediastinum, comprising 20-30% of all mediastinal masses. [1] Seventy percent of thymomas occur in patients over the age of 40 years, and nearly all thymomas occur over the 20 years of age. [2],[3] Clinical presentation may vary; from asymptomatic mediastinal masses detected on chest radiographs to compressive symptoms like dysphagia, venous congestion or dyspnea. Some tumors are associated with paraneoplastic syndromes like myasthenia gravis, pure red cell aplasia, acquired hypogammaglobulinemia, and connective tissue disorders. [4]
In children, mediastinal neoplasms are mainly lymphomas or neurogenic tumors. Thymoma is extremely rare in children and adolescents, with less than 50 cases of pediatric thymoma reported in the literature. [2],[5] As a result of this rarity, it is difficult to predict prognosis or formulate treatment guidelines for these patients. In a comprehensive review, Liang et al. have attempted the same in patients of pediatric thymoma reported over the past 3 decades. They found that younger (<10 years) and male patients had a worse prognosis. [5] We report a case of thymoma in an 8-year-old boy with early tumor stage and favorable clinical and histopathological features.
 Case report Case report | |  |
An 8-year-old boy presented to the pediatric clinic with a 3-month history of intermittent cough and occasional pain in the right upper chest. There was no history of dysphagia or dyspnea. General physical and systemic examination, including lymph nodes and genitalia were normal. The chest radiograph revealed a right perihilar shadow with mediastinal widening. Computed tomography (CT) chest revealed a large, (maximum diameter 7.2 cm) lobulated, homogenous soft tissue mass in the anterior mediastinum arising from the right side of the thymus gland. The mass was overlying the superior vena cava and brachiocephalic vein; however, the fat planes were maintained. The posterior surface of the mass was partly abutting the pericardium. There was no lymphadenopathy or pleural effusion, and both the lungs were normal [Figure 1]. Serum levels of markers for germ cell tumors, that is, α-fetoprotein, β-human chorionic gonadotropin and lactate dehydrogenase were within the normal range. Image-guided fine-needle aspiration cytology from the lesion showed a lymphoepithelial lesion, suggestive of a thymoma or thymic hyperplasia. Serum levels of anti-acetylcholine receptor antibodies were normal.
With a provisional diagnosis of thymoma, the boy underwent a midline sternotomy. There was a solitary, well-encapsulated, multi septated mass measuring around 7.5 cm × 3.5 cm × 3 cm arising from the thymus and overlying the superior vena cava and brachiochephalic vein. The lower part was abutting the pericardium; however, the lesion could be easily separated from the pericardium and the great vessels. Complete resection was performed. The patient had an uneventful recovery and was discharged on the seventh postoperative day. On cut-section, there were cystic areas containing necrotic material [Figure 2]. Microscopy revealed a well-encapsulated tumor arranged in lobules and nests separated by fibrous septa, along with extensive areas of necrosis. In high-power (×100), an admixture of round to oval epithelial cells devoid of atypia admixed with small lymphocytes in even proportions, could be appreciated [Figure 3]. A final diagnosis of thymoma (Masaoka stage I, WHO type B2) with extensive areas of necrosis was made. The patient is asymptomatic during his follow-up visits. | Figure 1: Computed tomography chest showing a large, lobulated, homogenous soft tissue anterior mediastinal mass (marked T). Fat planes with the superior vena cava, brachiocephalic vein and pericardium are maintained
Click here to view |
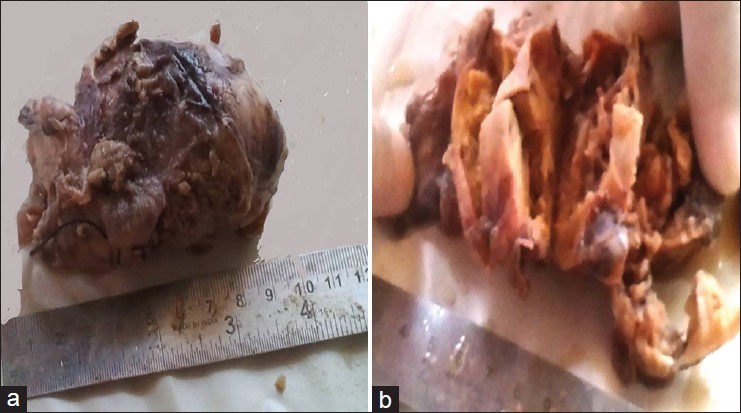 | Figure 2: Gross images show (a) A well-circumscribed mass with intact capsule (b) cut-surface shows cystic change with extensive necrosis
Click here to view |
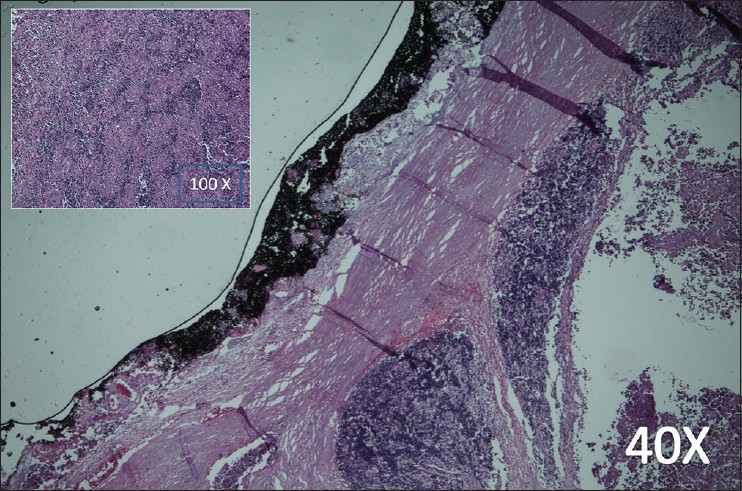 | Figure 3: Photomicrograph shows encapsulated tumor with extensive necrosis with few preserved areas (H and E, ×40). High-power (inset) shows admixture of epithelial cells and small lymphocytes (H and E, ×100)
Click here to view |
 Discussion Discussion | |  |
Thymomas and thymic carcinomas are epithelial tumors of the thymus. In children, thymic lesions comprise only 2-3% of all mediastinal tumors, with thymomas still rarer (<1%). [2],[3] The presenting symptoms may vary widely; from vague chest discomfort, to florid compressive symptoms like dyspnea and superior vena cava syndrome. Some children may have an incidentally-detected soft tissue mass with calcifications, on chest radiograph. Approximately, 20% of children with thymomas have paraneoplastic syndromes, of which around 70% are myasthenia gravis. [5] Myasthenia gravis is also mostly seen in children with thymoma who are <10 years of age, and in 70% of patients with the B2 subtype. [5] All patients with suspected thymoma should have serum antiacetylcholine receptor antibody levels measured before surgery. However, despite having these features, our patient had negative antibody test.
Contrast-enhanced CT is the imaging modality of choice in the evaluation and staging of thymoma. Resectable lesions which are unequivocally thymomas on imaging do not mandate preoperative biopsy.
The most widely used thymoma classification is the Masaoka staging system which is based on the presence of invasion into surrounding organs, completeness of resection, association with myasthenia gravis, tumor size, and involvement of great vessels, to determine postoperative survival. [6],[7] The WHO system, based on the morphology of epithelial cells as well as the lymphocyte-to-epithelial cell ratio, was developed in 1999 to include histological features as prognostic factors. [8] Both these systems have been evaluated in large series; the clinical value of both has been validated. [7],[9] Liang et al. reviewed 32 cases of pediatric thymoma in English literature and found that younger patients (<10 years old) were predominantly male, presented with a more advanced tumor stage (Masaoka stage III/IV), had a less favorable outcome and were more likely to have paraneoplastic syndromes. [5] The unusual features in our patient were the absence of adverse prognostic factors like local invasion and autoimmune disorders (myasthenia gravis), despite the young age (<10 years). Extensive necrosis is seldom seen in thymoma with only a few reports mentioning necrosis in adult patients. However, none reported the same in children. [10],[11] Moran et al. studied 25 cases of thymoma with necrosis; the authors do not consider it an adverse prognostic factor. [11] This may explain the simultaneous presence of necrosis and other favorable factors in our case.
Surgical resection is the mainstay of treatment for epithelial lesions of the thymus. Radiation and chemotherapy are reserved for treatment of invasive and malignant disease. In children, treatment protocols have not been clearly defined due to paucity of cases; however, most authors have favored regimens similar to adult regimens, that is, based on cisplatin, doxorubicin, prednisolone, and cyclophosphamide. [5] Tumor stage and complete surgical resection are significant prognostic factor in pediatric patients. Complete resection is also a significant predictor of 5-year survival in Masaoka stage I, II and III. [12] Despite the fact that WHO type B2 disease has poorer long-term survival (~60%), most authors do not recommend adjuvant therapy for these patients after complete resection. [13] Since our case had all favorable factors and one doubtful factor (B2 disease), we did not prescribe adjuvant treatment. The patient is, however, on long-term surveillance for recurrence and detection of second malignancies like non-Hodgkin lymphoma and soft tissue sarcomas, which are known to occur. [14]
 Conclusion Conclusion | |  |
Thymoma in young children is a rare entity and carries an unfavorable prognosis. Complete surgical excision is the treatment modality of choice. Due to its common association with myasthenia gravis, serum antiacetylcholine receptor levels should be measured before surgery in all patients.
 References References | |  |
| 1. | Lewis JE, Wick MR, Scheithauer BW, Bernatz PE, Taylor WF. Thymoma. A clinicopathologic review. Cancer 1987;60:2727-43.  |
| 2. | Furman WL, Buckley PJ, Green AA, Stokes DC, Chien LT. Thymoma and myasthenia gravis in a 4-year-old child. Case report and review of the literature. Cancer 1985;56:2703-6.  |
| 3. | Santana L, Givica A, Camacho C, Armed Forces Institute of Pathology. Best cases from the AFIP: Thymoma. Radiographics 2002;22:S95-102.  |
| 4. | Riedel RF, Burfeind WR Jr. Thymoma: Benign appearance, malignant potential. Oncologist 2006;11:887-94.  |
| 5. | Liang X, Lovell MA, Capocelli KE, Albano EA, Birch S, Keating AK, et al. Thymoma in children: Report of 2 cases and review of the literature. Pediatr Dev Pathol 2010;13:202-8.  |
| 6. | Masaoka A, Monden Y, Nakahara K, Tanioka T. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92.  |
| 7. | Masaoka A. Staging system of thymoma. J Thorac Oncol 2010;5:S304-12.  |
| 8. | Rosai J. Histological typing of tumours of the thymus. In: World Health Organization International Classification of Tumours. 2 nd ed. Berlin: Springer; 1999.  |
| 9. | Sonobe S, Miyamoto H, Izumi H, Nobukawa B, Futagawa T, Yamazaki A, et al. Clinical usefulness of the WHO histological classification of thymoma. Ann Thorac Cardiovasc Surg 2005;11:367-73.  |
| 10. | Cui W, Zhang D, Tawfik O. Thymoma with extensive necrosis: A case report and review of literature. Pathologica 2006;98:652-4.  |
| 11. | Moran CA, Suster S. Thymoma with prominent cystic and hemorrhagic changes and areas of necrosis and infarction: A clinicopathologic study of 25 cases. Am J Surg Pathol 2001;25:1086-90.  |
| 12. | Davenport E, Malthaner RA. The role of surgery in the management of thymoma: A systematic review. Ann Thorac Surg 2008;86:673-84.  |
| 13. | Okumura M, Ohta M, Tateyama H, Nakagawa K, Matsumura A, Maeda H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer 2002;94:624-32.  |
| 14. | Pan CC, Chen PC, Wang LS, Chi KH, Chiang H. Thymoma is associated with an increased risk of second malignancy. Cancer 2001;92:2406-11.  |
[Figure 1], [Figure 2], [Figure 3]
|