|


 |
| CASE REPORT |
|
| Year : 2015 | Volume
: 7
| Issue : 1 | Page : 4-6 |
|
|
Persistent mullerian duct syndrome with transverse testicular ectopia
P Naresh Kumar, Kandgal Venugopala
Department of General Surgery, Sri Manakula Vinayagar Medical College and Hospital, Madagadipet, Pondicherry, India
| Date of Web Publication | 29-Jun-2016 |
Correspondence Address:
P Naresh Kumar
B52, Srinivas Towers, Oulgaret, Moolakulam, Pondicherry - 605 010
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2006-8808.184940

 Abstract Abstract | | |
Persistent Mullerian duct syndrome (PMDS) is a rare form of male pseudohermaphroditism characterized by the presence of Mullerian duct structures in a normal male with 46, XY karyotype. Transverse testicular ectopia (TTE) is rare form of testicular ectopia in which two testes are located on one inguinal side. The opposite scrotum is empty. PMDS with TTE is rare. We report a case of PMDS with TTE discovered during surgery for a right inguinal hernia in a 25-year-old male. Keywords: Mullerian inhibiting factor, persistent Mullerian duct syndrome, transverse testicular ectopia
How to cite this article:
Kumar P N, Venugopala K. Persistent mullerian duct syndrome with transverse testicular ectopia. J Surg Tech Case Report 2015;7:4-6 |
How to cite this URL:
Kumar P N, Venugopala K. Persistent mullerian duct syndrome with transverse testicular ectopia. J Surg Tech Case Report [serial online] 2015 [cited 2018 Jul 1];7:4-6. Available from: http://www.jstcr.org/text.asp?2015/7/1/4/184940 |
 Introduction Introduction | |  |
The Mullerian duct regresses in male due to a glycoprotein secreted by the developing testes called Mullerian inhibiting factor (MIF). Failure to regress may be due to lack of MIF or defective MIF receptor, resulting in various disorders of regression, and one such disorder is persistent Mullerian duct syndrome (PMDS). PMDS is a rare form of male pseudohermaphroditism characterized by the presence of uterus and fallopian tubes in phenotypically and genotypically normal male (46, XY), with testosterone production and responsiveness.[1]
The association between PMDS and transverse testicular ectopia (TTE) is even more uncommon.
 Case Report Case Report | |  |
A 25-year-old male presented with absent left testis since birth and right sided inguinal swelling for 5 years, and pain in swelling for 2 days. On physical examination, the left scrotum was empty, and right side revealed indirect inguinal hernia with right testis at the root of the scrotum. The penis was well developed. The patient was phenotypically male, exhibiting normal secondary sexual characteristics. The past history indicated primary infertility.
Semen analysis revealed azoospermia. Ultrasonography showed right inguinal hernia with undescended testis in the right inguinal canal and an absent testis on the left side.
Surgical exploration revealed indirect sac with the right testis. While retrieving the testis, we noticed a complex mass resembling uterus-like structure, and gonad (left) with the fimbria-like structure [Figure 1].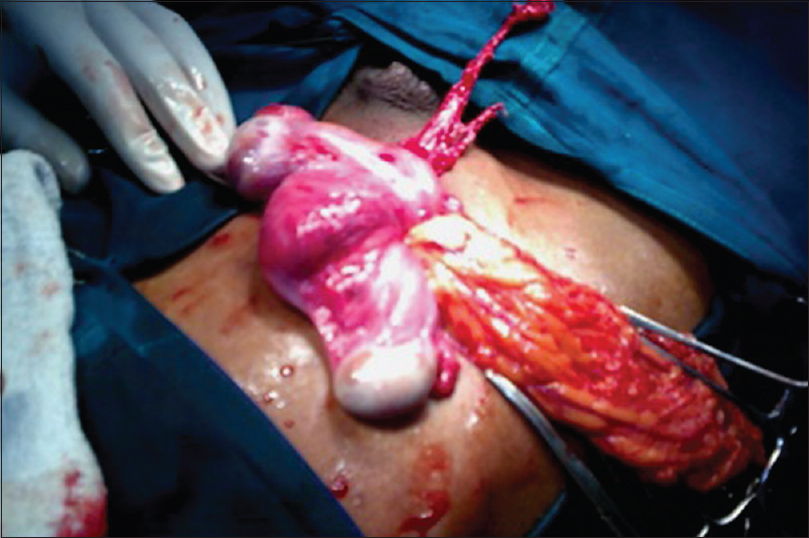 | Figure 1: Gonad with Fimbria-like structure (above), uterus like structure (middle), and testis (below)
Click here to view |
Both the gonads had vas deferens and vascular supply. Orchiopexy was done on the right side. The uterus like structure was removed along with left gonad as it was atrophic and sent for histopathology. Right inguinal hernioplasty was done.
Histopathological study proved it to be uterus [Figure 2] and left gonad like structure proved to be testis which was atrophic without spermatogenesis [Figure 3].
Chromosomal analysis revealed normal male genotype – 46 XY [Figure 4].
 Discussion Discussion | |  |
Embryologically, between 7th and 8th week of gestation, masculinization occurs in a male fetus. Testosterone secreted by the Leydig cells in the testis helps in the development of Wolffian duct in to vas deferens, epidydimis and seminal vesicle. MIF secreted by Sertoli cells in the testis, acts locally to suppress the Mullerian ducts and causes their regression by 8th and 10th weeks of gestation. PMDS results from failure of synthesis of MIF, or failure of end organs to respond to MIF.[2] MIF gene has been mapped to chromosome 19. Receptor for MIF is expressed in Sertoli cells, granulosa cells and Mullerian duct.[3] MIF does not have direct role in the descent of testes. The mechanical effect of persistent Mullerian duct structures might produce cryptorchidism by preventing normal testicular descent.[4]
Male pseudohermaphroditism results from the defective formation or action of androgens or MIF. PMDS represents a small fraction of this broad spectrum of male pseudohermaphroditism, characterized by the presence of well-developed or rudimentary uterus, cervix, vagina and fallopian tube in normal 46 XY male. Patients with PMDS have normal androgen production, male external genitalia and normal penile development. Testis show features of atrophy due to cryptorchidism. Infertility is common but fertility has been reported in a few.[5]
Normally the testis is located in the scrotum at birth. Failure of the testis to descend in to the scrotum at birth results in undescended testis. Ectopic testis have been reported at various sites including superficial inguinal pouch, suprapubic, femoral, perineal region and the base of penis. Migration of the testis to the opposite side where both testis pass through the same inguinal canal is known as TTE.
PMDS occurs as:
- Partially descended testicles (80– 90% of cases) with unilateral cryptorchidism and contralateral inguinal hernia. The term “hernia uteri inguinalis” is used when uterus is found in the hernia sac
- Sometimes the contralateral testis is found in the hernia sac due to abnormal mobility of the Mullerian derivatives, known as TTE
- Bilateral cryptorchidism with uterus fixed in pelvis and both testes embedded in round ligaments.[4],[6]
The undescended gonads have a high risk of malignancy.[1],[7]
A rare form of clear cell adenocarcinoma of the Mullerian duct in PMDS [8] has been reported. Diagnosis is usually made incidentally during surgery for an inguinal hernia or exploration for cryptorchidism. TTE is suspected preoperatively in patients with unilateral inguinal hernia and contralateral nonpalpable testis.[4],[9] Laparoscopy, ultrasonography, and MIF detection using bioassay techniques is helpful in diagnosing the syndrome.[1] The diagnosis is confirmed with testicular biopsies and chromosomal studies.[6],[9]
Removal of these structures may damage the vas deferens which lies in close proximity. Hysterectomy is indicated when the Mullerian structures limit intrascrotal placement of testis. Orchidectomy is indicated when testes cannot be mobilized to a palpable location. Otherwise orchiopexy is done and patient kept on long-term follow-up.[6],[9]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Berkmen F. Persistent müllerian duct syndrome with or without transverse testicular ectopia and testis tumours. Br J Urol 1997;79:122-6.  |
| 2. | Thompson ST, Grillis MA, Wolkoff LH, Katzin WE. Transverse testicular ectopia in a man with persistent Müllerian duct syndrome. Arch Pathol Lab Med 1994;118:752-5.  |
| 3. | Lane AH, Lee MM. Clinical applications of Müllerian inhibiting substance in patients with gonadal disorders. Endocrinologist 1999;9:208-15.  |
| 4. | Karnak I, Tanyel FC, Akçören Z, Hiçsönmez A. Transverse testicular ectopia with persistent müllerian duct syndrome. J Pediatr Surg 1997;32:1362-4.  |
| 5. | Sheehan SJ, Tobbia IN, Ismail MA, Kelly DG, Duff FA. Persistent Müllerian duct syndrome. Review and report of 3 cases. Br J Urol 1985;57:548-51.  |
| 6. | Vandersteen DR, Chaumeton AK, Ireland K, Tank ES. Surgical management of persistent müllerian duct syndrome. Urology 1997;49:941-5.  |
| 7. | Eastham JA, McEvoy K, Sullivan R, Chandrasoma P. A case of simultaneous bilateral nonseminomatous testicular tumors in persistent müllerian duct syndrome. J Urol 1992;148:407-8.  |
| 8. | Shinmura Y, Yokoi T, Tsutsui Y. A case of clear cell adenocarcinoma of the müllerian duct in persistent müllerian duct syndrome: The first reported case. Am J Surg Pathol 2002;26:1231-4.  |
| 9. | Buchholz NP, Biyabani R, Herzig MJ, Ali A, Nazir Z, Sulaiman MN, et al. Persistent Müllerian duct syndrome. Eur Urol 1998;34:230-2.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|