|
 
 |
| CASE REPORT |
|
| Year : 2013 | Volume
: 15
| Issue : 1 | Page : 33-36 |
|
Herniated mobile descending colon
JG Makama1, P Enesi1, J Jibrin2
1 Department of Surgery, Ahmadu Bello University Teaching Hospital, Shika-Zaria, Nigeria
2 Department of Radiology, National Ear Care Center, Kaduna, Nigeria
| Date of Web Publication | 22-Sep-2014 |
Correspondence Address:
J G Makama
Department of Surgery, Ahmadu Bello University Teaching Hospital, Shika-Zaria
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/1595-1103.141394

Persistent descending mesocolon is a congenital anomaly that has been shown, in most cases, to be asymptomatic because of its short length. To the best of our literature review and knowledge, no case of internal herniation of the mobile descending colon into either gastrocolic or splenocolic recesses have been reported. We therefore wish to report a case of herniated mobile descending colon in a middle-aged woman. HA was a 54-year-old female with a 2-year history of recurrent episodes of left upper quadrant pain of the abdomen. The pain, which was initially dull aching, suddenly became sharp in nature and so severe that it precluded her from doing her domestic activities. She had undergone clinical evaluation and work up previously but no etiology for her pain was found. After resuscitation, she consented to exploratory laparatomy for an acute on-chronic abdominal pain of unknown etiology. The intraoperative findings were a portion of the wall of the left colon seen to have herniated into a small band of tissue on the left posterior wall. The whole descending colon was unattached to the posterior peritoneum. The trapped portion (4 cm in length) of the wall of the colon was released and a warm pack was applied to the segment of large bowel so released. Following this maneuver, the portion was found to be viable and so a left colopexy was performed and the adhesion band that was placed obliquely from the spleen toward the midline was excised. Postoperative period was uneventful and since then the patient's abdominal pain has been abated over the past 1 year. The morbidity of a mobile descending colon includes internal herniation. Therefore, early detection and colopexy is necessary. Keywords: Colon, descending colon, herniation, hernia, mobile-descending, mobile
How to cite this article:
Makama J G, Enesi P, Jibrin J. Herniated mobile descending colon. Niger J Surg Res 2013;15:33-6 |
| Introduction | |  |
Mobile descending colon is uncommon. [1] Mobile cecum and ascending colon appear to occur more frequently. [2] Embryologically, the ascending and the descending colon are usually plastered to the posterior peritoneum. However, when this normal process of development fails, the colon may appear at the adult age with a well-formed mesentery of the ascending and/or descending colon. Persistent descending mesocolon is a congenital anomaly that has been shown, in most cases, to be asymptomatic because of its short length. [2],[3] Only a few cases of volvulus of the descending colon have been reported. [1],[3],[4] Similarly, internal herniation of the mobile descending is uncommon. We report a case of herniated mobile descending colon in a middle-aged woman.
| Case Report | |  |
HA was a 54-year-old female trader who presented with a 2-year history of recurrent episodes of left upper quadrant pain of the abdomen. The pain has been dull aching and recurrent in the past. However, the left abdominal pain suddenly became sharp in nature and so severe that it precluded her from engaging in her trading in the preceding 1 week and centered mainly in the left side of the abdomen. The pain was associated with nausea and a feeling of blotted abdomen. However, the patient did not have obvious abdominal distension and no constipation or vomiting. No other associated symptoms were noted. She had extensive evaluation and work up previously in a peripheral hospital, but no etiology for her pain was found.
Physical examination revealed a middle-aged woman, who was well nourished and not pale. She was afebrile with a temperature of 37.1°C. The cardiopulmonary status was normal with a pulse rate of 89/min, blood pressure of 120/88 mmHg, and lung fields were clear.
The abdomen was full soft with marked tenderness in the left upper quadrant. However, there was no palpable mass. Digital rectal examination was normal.
Hemogram was within normal limits. Abdominopelvic ultrasound was essentially normal too. Erect and supine abdominal X-ray studies done were within normal limits. After resuscitation, she consented to exploratory laparatomy for an acute on-chronic abdominal pain of unknown etiology. The intraoperative findings or abnormalities were a portion of the wall of the left colon was seen to have herniated [Figure 1] into a small band of tissue on the left posterior wall and the whole descending colon unattached to the posterior peritoneum [Figure 2] have entirely a well form mesentery. The trapped portion of the wall of the colon was released and application (for 5 min) of gauze soaked in warm saline [Figure 3] done. Following this maneuver, the portion was found to be viable [Figure 4] and so a left colopexy, using a lateral peritoneal flap was performed. The small band of tissue was then excised. Postoperative period was uneventful and since then the patient's abdominal pain has been abated over the past 1 year.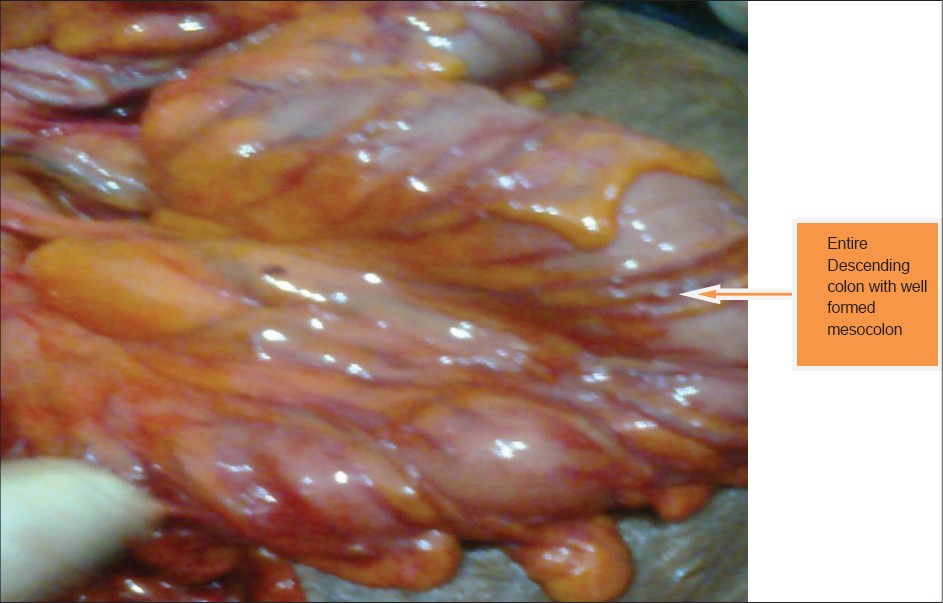 | Figure 4: Entire mobility of the descending colon and showing
viability of the wall
Click here to view |
| Discussion | |  |
The descending colon is usually surrounded by peritoneum on three sides: The left lateral, the anterior surface, and the medial sides of the colon. The posterior side is devoid of peritoneum and thus the descending colon is a retroperitoneal structure without a mesocolon. [2],[4] This process usually occurs in the fourth through the fifth month of gestation. [4]
The primitive dorsal mesocolon has failed to fuse with the parietal peritoneum in few instances as reported previously. [1],[2],[3],[4],[5] This often results in a persistent descending mesocolon. This failure permits mobility of the descending colon, resulting in considerable variation in its position. Despite relative high incidence of anatomic variant of the cecum and ascending colon, abnormal cecal mobility and ascending colon is an uncommon cause of an acute clinical entity. [1],[2],[5],[6] The descending colon that has a lower incidence of this kind of anatomic variation, expectedly, should have a much lower incidence of acute clinical entity. Commonly, it is thought that the descending colon with an intact mesocolon swings to the midline or slightly to the left of the midline. [3] This action will create a space into which all or a part of the small bowel may migrate to. However, contrary to this, they have been found to, usually, reside in a normal anatomic position. [5],[6] This, probably, may explain the reason why the repeated abdominal ultrasounds and barium studies done on this patient in the past have often appeared normal. Probably, a superior investigation such as abdominal computed tomography (CT) scan could have enhanced the preoperative detection, as previously reported [7] of the herniated wall of the colon but in this case the non-availability of CT scan and the need to cut down the cost of treatment precluded us from doing it. In addition, chronic constipation may result in a markedly redundant dilated colon that is often associated with an elongated mesocolon. Thus, further increase the mobility of the colon. Our patient had a long redundant segment of descending colon and an associated large mesocolon even though the history of recurrent episodes of constipation was lacking in her.
It has been reported that this configuration (intact mesocolon) of the descending colon could allow quite a number of things to have happened. [1],[3],[4] The colon may undergo repeated torsion and probably detorsion, and it has been reported [5],[8],[9] that this could give rise to chronic transient abdominal pain that is usually associated with these patients. Our patient had repeated episodes of abdominal pain on the left side of the abdomen. Perhaps these episodes of pains may be due to repeated torsion and detorsion of the descending colon. In some cases, the torsion may lead to a closed-loop large intestinal obstruction in which it is often referred to as volvulus of the descending colon. [4],[5],[10],[11] Often times the patient will present with features of large bowel intestinal obstruction. In the index case, there was only history of feeling of a bloated abdomen, no obvious abdominal distension as reported by patient and was further confirmed during the physical examination of this patient. Intraoperative findings revealed non-obstruction of the lumen of the colon. This of course explains the absence of features of large bowel obstruction as seen in a classic volvulus.
The increase mobility in situations like this could also create high risk of internal herniation [3] of whole or part of the wall of the colon as it was found in this patient. Even though there are well-known recesses through which internal herniation have been reported, in this patient, it was through a band of tissue running obliquely from the tip of spleen toward the midline in the upper posterior abdominal cavity separate from the usual gastrocolic and splenocolic recesses. The patient was lucky, at operation, the wall, which was about 4 cm in length, of the colon was found to be viable after application of warm pack to the segment of large bowel and so did not warrant resection and anastomosis.
The band of tissue that caused the herniation was excised completely and left colopexy done. Colopexy, which was first described by Dixon and Meyers in 1948, [12] is said to be the surgical technique of choice. First, the peritoneum lateral to the unattached portion of the colon is incised. A flap of peritoneum is then carefully raised, with care being taken not to injure any retroperitoneal structure. The descending colon is placed under the peritoneal flap and the free edge of the flap is sutured to the taenia coli using interrupted non-absorbable sutures. [12] The colon is thereby fixed partially to the retro peritoneum. This technique has stood the test of time and has shown to achieve a better fixation of the mobile cecum, ascending and in this case descending colon. Cecopexy, [12] right colopexy, [11] and right cecocolopexy [2] have been reported and currently laparoscopic [13],[14],[15] fixation is gradually gaining acceptability. In this case, the descending colon was involved, thus left lateral colopexy was done.
| Conclusion | |  |
The rare causes of chronic left abdominal pain may include problems related to a mobile descending colon. It is usually accompanied by a diagnostic dilemma. Diagnostic laparotomy may suffice in extremely difficult cases. For mobile descending colon due to intact mesocolon, left colopexy (open or laparoscopically), using the lateral peritoneal flap, is an effective method of fixing the descending colon and prevents subsequent morbidity.
| References | |  |
| 1. | Vyas KC, Joshi CP, Misra S. Volvulus of descending colon with anomalous mesocolon. Indian J Gastroenterol 1997;16:34-5. 
|
| 2. | Makama JG, Ahmed A, Ukwenya Y, Mohammed I. Mobile caecum and ascending colon syndrome in a Nigerian adult. Ann Afr Med 2009;8:133-5. 
[PUBMED]  |
| 3. | Liew KL, Choong CS, Shiau GF, Yang WC, Su CM. Descending mesocolon defect herniation: Case report. Changgeng Yi Xue Za Zhi 1999;22:133-7. 
|
| 4. | Chen A, Yang FS, Shih SL, Sheu CY. Case report. CT diagnosis of volvulus of the descending colon with persistent mesocolon. AJR Am J Roentgenol 2003;180:1003-6. 
|
| 5. | Tirol FT. Cecocolic torsion: Classification, pathogenesis, and treatment. JSLS 2005;9:328-34. 
[PUBMED] |
| 6. | Pirro N Corroller LE, Solari C, Merad A, Sielezneff I, Sastre B, et al. Caecal volvulus: Anatomical bases and physiopathology. Morphologie 2006;90:197-202. 
|
| 7. | Macari M, Spieler B, Babb J, Pachter HL. Can the location of the CT whirl sign assist in differentiating sigmoid from caecal volvulus? Clin Radiol 2011;66:112-7. 
|
| 8. | Rogers RL, Harford FJ. Mobile caecum syndrome. Dis Colon Rectum 1984;27:399-402. 
[PUBMED] |
| 9. | Lepage-Saucier M, Tang A, Billiard JS, Murphy-Lavallée J, Lepanto L. Small and large bowel volvulus: Clues to early recognition and complications. Eur J Radiol 2010;74:60-6. 
|
| 10. | Delabrousse E, Sarliève P, Sailley N, Aubry S, Kastler BA. Cecal volvulus: CT findings and correlation with pathophysiology. Emerg Radiol 2007;14:411-5. 
|
| 11. | Lee YJ, Lee YA, Liu TJ, Chang TH. Mobile caecum syndrome: A report of two cases. Zhonghua Yi Xue Za Zhi (Taipei) 1996;57:380-3. 
|
| 12. | Dixon CF, Meyer AC. Volvulus of the caecum. Surg Clin North Am 1948;28:953-63. 
[PUBMED] |
| 13. | Tsushimi T, Kurazumi H, Takemoto Y, Oka K, Inokuchi T, Seyama A, et al. Laparoscopic cecopexy for mobile cecum syndrome manifesting as cecal volvulus: Report of a case. Surg Today 2008;38:359-62. 
|
| 14. | Thanapongsathron W, Kanjanabut B, Vaniyapong T, Thaworncharoen S. Chronic right lower quadrant abdominal pain: Laparascopic approach. J Med Assoc Thai 2005;88:S42-7. 
|
| 15. | Cartwright-Terry T, Phillips S, Greenslade GL, Dixon AR. Laparoscopy in the management of closed loop sigmoid volvulus. Colorectal Dis 2008;10:370-2. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|