|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 9
| Issue : 1 | Page : 39-43 |
|
Clinical profile and management of aerodigestive foreign bodies in North - western Nigeria
Abdullahi Musa Kirfi, Garba Mainasara Mohammed, Tijjani Sa'idu Abubakar, Abimiku Solomon Labaran, Musa Thomas Samdi, Mohammed Bello Fufore
Department of Clinical Services, National Ear Care Centre, PMB 2438, Kaduna, Nigeria
| Date of Web Publication | 13-Nov-2014 |
Correspondence Address:
Abdullahi Musa Kirfi
Department of Clinical Services, National Ear Care Centre, Golf Course Road, Off Independence Way PMB 2438, Kaduna
Nigeria
  | Check |
DOI: 10.4103/1858-5000.144663 
Background: Aeordigestive tract emergences in Nigeria occur in all age groups. They sometimes have dreaded outcome if lodged in air passages. Objective: The aim is to present the results of this problem in a 5-year retrospective survey of cases in the Emergency Unit of the National Ear Care Centre, Kaduna, Nigeria, from January 2009 to December 2013. Methods: Retrieved cases were studied noting the clinical history, examination and intervention. The study included all patients diagnosed with aerodigestive foreign bodies within the period stated. Results: Fifty-seven thousand nine hundred and four patients were studied. Fifteen thousand eight hundred and fifty were emergencies. The hospital prevalence was 0.61% and the average annual incidence was 0.13%, male preponderance with male to female ratio of 2.24-1.00. All patients were symptomatic. Mortality was recorded in one patient who had a co-morbidity of esophageal perforation. Conclusion: Aerodigestive foreign bodies pose a serious challenge in a setting of poor resources and scarcity in diagnostic and interventional facilities Keywords: Aerodigestive foreign bodies, emergency ear care, Nigeria
How to cite this article:
Kirfi AM, Mohammed GM, Abubakar TS, Labaran AS, Samdi MT, Fufore MB. Clinical profile and management of aerodigestive foreign bodies in North - western Nigeria. Sudan Med Monit 2014;9:39-43 |
How to cite this URL:
Kirfi AM, Mohammed GM, Abubakar TS, Labaran AS, Samdi MT, Fufore MB. Clinical profile and management of aerodigestive foreign bodies in North - western Nigeria. Sudan Med Monit [serial online] 2014 [cited 2018 Mar 31];9:39-43. Available from: http://www.sudanmedicalmonitor.org/text.asp?2014/9/1/39/144663 |
| Introduction | |  |
Aerodigestive tract emergencies are not uncommon in developing countries like Nigeria and can occur in all age groups. [1] They present great difficulties for parents, patients, and the few Otorhinolaryngologists. [2] However, aerodigestive foreign bodies may turn out uneventful depending on its type, size, and location in the aerodigestive tract. Whatever the location, the most dreaded outcome of the event is seen when the foreign body is lodged in the air passage. [2] The most commonly ingested foreign bodies by children include coins, screws, buttons, and toys. [3],[4],[5],[6] An estimated 1500-2750 individuals die annually in the United States following the ingestion of foreign objects. [7] Significant proportion of impaction particularly in the elderly occurs at the site of benign or malignant strictures. [8] There are several reported serious and sometimes fatal complications associated with impacted pharyngo-esophageal foreign objects due either too late diagnosis, late referral to the hospital, or mismanagement. [7] A number of foreign bodies that are impacted in the throat are associated with acute symptoms calling for prompt removal. [9] Some of the swallowed foreign bodies pass harmlessly through the gastrointestinal tract. [10]
Rigid esophagoscopy for the removal of foreign bodies remains the best mode of treatment. [11],[12],[13] Others of importance include the use of flexible esophagoscopy, cervical esophagotomy, open thoracotomy, [14],[15] and the use of Foley's catheter under fluoroscopic guidance. [11],[16],[17] Morbidity and mortality observed in cases of impacted aerodigestive foreign bodies in developing countries mainly stem from late presentation, late diagnosis, late referral to hospital, lack of adequate skills as well as nonavailability of relevant equipment in the hospitals. [18] Complications such as esophageal perforations, abscesses formation, pneumonia, may occur. [19],[20],[21],[22],[23] There might be associated anesthetic complications and sometimes mortality from either the foreign body or the procedure adopted for its removal. [24]
| Materials and methods | |  |
This is a 5-year retrospective study of all patients who presented to the emergency unit of the National Ear Care Center Kaduna Nigeria with diagnosis of aerodigestive foreign bodies from 1st January 2009 to 31st December 2013. Ethical clearance was obtained from the Research Ethics Committee of the study center.
The case notes of patients diagnosed with aerodigestive foreign body were retrieved. Demographics (age, gender, occupation, and tribe), clinical histories (duration of ingestion/aspiration, cough, drooling of saliva, dyspnea, Dysphagia, odynophagia, chocking), examination findings (respiratory distress, fever, clinical status of the chest), investigations (X-ray soft tissue neck antero-posterior and lateral views, chest X-ray, serum electrolytes, packed cell volume) as well as intervention given (resuscitation, operative procedure, and intraoperative findings) were extracted. The data was analyzed using simple descriptive statistics. Results obtained from the analyzed data are as shown.
Inclusion criteria
All patients with a diagnosis of aerodigestive foreign bodies within the period under review.
Exclusion criteria
Patients with incomplete records in their file.
| Results | |  |
Fifty-seven thousand nine hundred and four patients were seen at the study center during the period. Fifteen thousand eight hundred and fifty were emergencies out of which 96 presented with aerodigestive foreign bodies. The calculated hospital prevalence was 0.61%. The average annual incidence was 0.13%. Two patients did not meet the inclusion criteria and were excluded.
The minimum age at presentation was 3 months; maximum age was 80 years, with a mean age of 17.36 ± 20.03 years. [Table 1] shows the different age groups where aerodigestive foreign bodies were seen. Aerodigestive foreign bodies among Nigerians showed male preponderance, with a male to female ratio of 2.24:1. All our patients were symptomatic, having more than one symptom; the most common symptom was chocking seen in 60 (%) of the patients, while the less common was fever seen in 14%. Predominantly, the aerodigestive foreign bodies were lodged in the digestive tract while the airway foreign bodies constitute 30%.
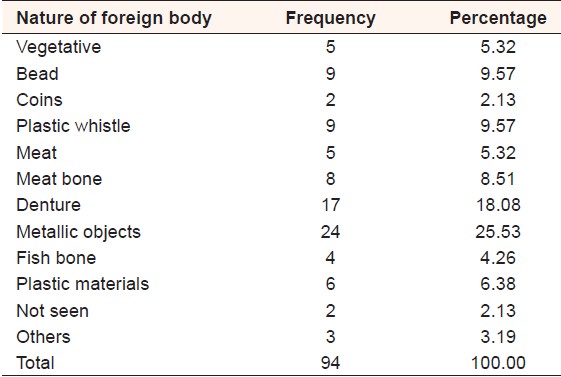
Depending on the suspected site of impaction, an appropriate procedure was conducted. [Table 2] shows esophagoscopy and foreign body removal as the most frequent procedure performed. Various objects and items were retrieved from the aerodigestive tracts of the patients. Intraoperatively, via rigid and flexible esophagoscopies, no foreign body was seen in 2 (2.13%) patients. [Table 3] shows that the majority of the foreign bodies were of metallic origin, especially in the pediatric age groups, while denture was the predominant aerodigestive foreign body in adults.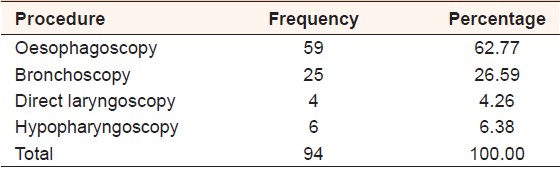 | Table 2: Procedures performed for retrieval of aerodigestive foreign bodies among Nigerians
Click here to view |
 | Table 3: Nature of aerodigestive foreign bodies retrieved among Nigerians
Click here to view |
Mortality was recorded in 1 (1.06%) patient who has co-morbidity. Esophageal perforation from denture impaction was seen in 3 (3.19%), post-operative pyrexia, cardiac arrest, and death was recorded each in 1 (1.06%) of the patients. Importantly, 88 (93.62%) of our patients did not develop any complication from either the impacted foreign body or the procedure performed.
| Discussion | |  |
Fifty-seven percent of those presented with aerodigestive foreign bodies to our center were children under 9 years of age. It shows another peak at 50-59 age group (11%). This finding is in consonance with the work of Alabi et al. [3] in Ilorin, Nigeria where the most common age group at presentation was 9 months to 3 years, also the work of Higo et al. [4] in Tokyo Japan, Mahafza et al. [5] and Al-Qudah et al. [23] in Jordan, Fatma et al. [15] in Turkey found the most affected age group to be under 3 years of age. Fifty-nine per cent of patients presenting with foreign bodies in Benin Nigeria were under 10 years of age in the work of Onyegwara et al. [2] It is not surprising that children under 9 years constitute the majority of our patients bearing in mind that children are so adventurous and usually do want to explore their facial orifices by inserting objects. However, most of the plastic whistles we encountered in this study were seen in children below 9 years of age. The second peak seen among those in the 50-59 years age bracket could be explained possibly by the increasing benign and or malignant esophageal conditions seen in the age bracket, especially in the developing world where malignancy age is observed to be about 10 years less than what is obtainable in the developed world.
Aerodigestive foreign bodies in Kaduna Nigeria showed male to female ratio of 2.2:1. This finding agrees with the work of Iseh et al. [7] in Sokoto Nigeria where the ratio approaches 2:1, as well as the works of Gulshan et al. [8] in Pakistan, Alabi et al. [3 ] in Ilorin Nigeria, Nwaorgu et al. [21] in Ibadan Nigeria and Onotai and Ibekwe [1] in Port Harcourt Nigeria. However, Al-Qudah et al. [23] in Jordan, Onyegwara et al. [2] in Benin Nigeria, Mahafza et al. [5] in Jordan as well as Fatma et al. [15] in Turkey did not find significant gender difference in their studies. No documented female preponderance was found in our literature search. The male preponderance found in this study could be attributed to the aggressiveness of the males.
Sixty-five (69.1%) of our patients had esophageal foreign bodies, 6 (9.23%) of which were located in the hypopharynx. Anatomically, the esophagus has its narrowest part at the region of the cricopharyngeus, demarcating the hypopharynx and the esophagus; the narrowing makes the area susceptible for foreign body impaction. This finding agrees with the work of Onotai and Ibekwe [1] in Port Harcourt Nigeria who found 66% in their series being esophageal foreign bodies. Similarly, our finding is in agreement with the works of Alabi et al. [3] in Ilorin Nigeria where over 50% of the aerodigestive foreign bodies were impacted in the pharyngo-esophageal region. However, Onyegwara et al. [2] in Benin Nigeria found only 8.3% of ENT foreign bodies in the esophagus. The low number of esophageal foreign bodies in the work of Onyegwara et al. could be the inclusion of aural and nasal foreign bodies within the study population.
Sixty (63.83%) of the patients presented to the health facility within the first 24 h of ingestion of the foreign body, that was quite impressive while 3 (3.19%) patients presented after the first 24 h, probably due to the distance from the facility. Charles et al. [14] reported the time of presentation of an esophageal foreign body after about 4 days of ingestion, associated with mortality as a complication. Iseh et al. [7] reported the maximum duration of 7 years from impaction of esophageal foreign body to presentation. However, Umana et al. [10] in Calabar Nigeria reported 7 weeks period from ingestion of foreign body to presentation for care. Complications may arise from late presentation. However, due to awareness campaign on the services of the study center, majority of the patients enrolled for the study presented to the facility within the first 24 h of ingestion. In the same vein, of 29 patients with airway foreign bodies, 28 (96.55%) of them presented for care within the first 24 h of inhalation. A patient was referred from a peripheral hospital after 72 h of inhalation of a plastic material. It is documented [12],[13],[15],[16],[17] that patients present earlier due to symptoms such as the stridor and respiratory embarrassment.
The symptomatology of our patients is in line with the findings of Majori et al. [20] Fidkowski et al. [24] and Onotai and Ibekwe. [1] Esophageal foreign bodies were found to be associated with choking especially in children, likely due to the small caliber of their esophageal lumen.
Fifty (53.19%) of our patients were dehydrated, only one (1.06%) was clinically pale, 70 (76.1%) were normothermic, 8 (8.7%) were cyanosed, necessitating <6 h of resuscitation in 77 (83.7%) of the patients, the remaining 44 (46.81%) were resuscitated for 6-12 h. It is worthy of note that the majority of the dehydrated patients presented with impacted esophageal foreign bodies, with associated drooling of saliva. Our findings agree with those of Onotai and Ibekwe [1] who resuscitated all his patients. An oropharyngeal foreign body was seen in 1 (1.06%), which was impacted in the tonsils.
Ninety-three (98.94%) patients had roentgenograms of the soft tissue neck (anteroposterior and lateral views) and the chest. X-ray of the soft tissue neck was suggestive of an aerodigestive foreign body in 58 (61.70%), while chest X-ray was suggestive of aerodigestive foreign body in 23 (24%) of the patients. Plain radiographs proofed very useful in the evaluation of patients with suspected aerodigestive foreign bodies, especially in developing countries where the full gamut of radiologic facilities are not, usually, available in health centers. Akazawa et al. [6] reported the sensitivity and specificity of plain radiographs in evaluating esophageal foreign body to be 54.8% and 100%, respectively.
Seventeen (18.09%) of the patients had preliminary emergency tracheostomy to secure the airway before the definitive procedure. In Port Harcourt Nigeria, Onotai and Ibekwe [1] performed emergency tracheostomy in 50 (35.2%) of his patients. This is higher than what we found in our study. This is likely due to late presentations in their series, as in both studies esophageal foreign bodies predominate.
Direct laryngoscopy and foreign body removal was done in 4 (4.23%) patients, hypopharyngoscopy and foreign body removal in 6 (6.38%), bronchoscopy and foreign body removal in 25 (26.59%) patients while esophagoscopy and foreign body removal was performed in 59 (62.77%) patients. The two patients with missing esophageal foreign bodies were referred to cardiothoracic surgeons for an open procedure. Rigid scopes, though not encouraged for removal of aerodigestive foreign bodies are found handy in Nigeria. Keith [22] and Majori et al. [20] both posited that Fiberoptic scopes are the only acceptable intervention for objects that have been impacted for more than a few hours, sharp objects such as flange of dentures, button batteries, and those that are not smooth or inert. Thus, flexible scopes are superior to rigid scopes in the setting of distally wedged foreign bodies; however, the scopes are in most instances, not available in most healthcare facilities in the developing countries.
In this study, metallic objects accounted for a larger proportion of the aerodigestive foreign bodies, followed by impacted denture materials. This finding contradicts the report put forward by Gulshan et al. [8] in Pakistan where coins (55.6%) and meat bolus (20.7%) accounted for the foreign bodies, and those of Iseh et al. [7] Mahafza et al. [5] Fatma et al. [15] and Al-Qudah et al. [23] who found coins, peanuts, toys among the most commonly ingested or aspirated foreign bodies. Reason for denture being a significant contributor of impacted foreign bodies in our series could be because our study population consisted of both the adults and pediatric age groups.
Retrieval of aerodigestive foreign bodies could be with complications. In this study, complication rate of 6.38% was recorded, about 50% of which was from impacted denture material. This appears to be slightly higher than what is reported by Mahafza et al. [5] Shraga et al. [16] who reported 2-6%. Iseh et al. [7] Al-Qudah et al. [23] did not report any complication. However, Onyegwara et al. [2] reported complication rate of 14%, which was attributed to late presentation. Singh et al. [17] found out that there is increased the incidence of complications with advancing age over 10 years of age.
Eighty-nine (94.68%) patients were discharged after an uneventful postoperative recovery. A patient that had cardiac arrest on the table was resuscitated and referred for intensive care. Three patients with esophageal perforations were referred to cardiothoracic surgeons for open operative treatment.
Hospital stay ranged from a day to 29 days; mean duration was 4 ± 4.08 days. Nwaorgu et al. [21] reported the maximum period of hospitalization as 32 days, with a mean of 9.4 days.
| Conclusion | |  |
Aerodigestive foreign bodies pose a serious challenge in the setting of a poor resource country with death of diagnostic and interventional facilities. Late presentation and advancing age are associated with complications.
| Acknowledgments | |  |
We wish to acknowledge the efforts of the Medical Director and also the records staff of the study center.
| References | |  |
| 1. | Onotai LO, Ibekwe MU. A Survey of upper aerodigestive tract emergencies seen in a Nigerian tertiary hospital. Int J Med Med Sci 2012;2:92-6.  |
| 2. | Onyegwara N, Okhahku A, Emokpaire E, Ogisi F. Dynamics in the trend of foreign bodies in ENT practice in Nigeria: Any change? Internet J Otorhinolaryngol 2012;14:2.  |
| 3. | Alabi BS, Oyinloye OI, Omokanye HK, Afolabi OA, Dunmade AD, Akande HJ. Foreign bodies in the upper aerodigestive tract of Nigerian children. Niger J Surg 2011;17:78-81.   |
| 4. | Higo R, Matsumoto Y, Ichimura K, Kaga K. Foreign bodies in the aerodigestive tract in pediatric patients. Auris Nasus Larynx 2003;30:397-401.  |
| 5. | Mahafza T, Batieha A, Suboh M, Khrais T. Esophageal foreign bodies: A Jordanian experience. Int J Pediatr Otorhinolaryngol 2002;64:225-7.  |
| 6. | Akazawa Y, Watanabe S, Nobukiyo S, Iwatake H, Seki Y, Umehara T, et al. The management of possible fishbone ingestion. Auris Nasus Larynx 2004;31:413-6.  |
| 7. | Iseh KR, Oyedepo OB, Aliyu D. Pharyngo-oesophageal foreign bodies: Implications for health care services in Nigeria. Ann Afr Med 2006;5:52-5.  |
| 8. | Gulshan H, Mahid I, Ihsanulla H, Mohammed H, Sharafat A. Esophageal foreign bodies: An experience with rigid esophagoscope. Gomal J Med Sci 2010;8:218-20.  |
| 9. | Dunmade AD, Segun BS, Olajide TG, Ologe FE. An Unusual Foreign Body: A Whole Fish in The Throat; A Paper Presented at the 12th Annual Scientific Conference of Otorhinolaryngological Society of Nigeria held in Abuja Nigeria; 2002.  |
| 10. | Umana AN, Offiong ME, Atana UE, Francis P, Adekanye GA, Mgbe RB, et al. Foreign body (Disk Battery) in the oesophagus mimicking respiratory problem in a 13 months old baby- delayed diagnosis. J Med Med Sci 2011;2:714-7.  |
| 11. | Onotai LO, Ebong EJ. Impacted fishing hook in the upper cervical esophagus of two Nigerians: Case reports. J Med Med Sci 2012;3:365-70.  |
| 12. | Kelly SM, Marsh BR. Airway foreign bodies. Chest Surg Clin N Am 1996;6:253-76.  |
| 13. | Henry KK, Karla B, Trevor M, Margaret AK, Dennis PL, Gerald BH. Airway foreign bodies; a 10-year review. Int J Pediatr Otorhinolaryngol 2000;56:91-9.  |
| 14. | Charles MD, Shabino L, Arthur NF. Esophageal perforation secondary to alkaline battery ingestion. J Am Coll Emerg Physicians 1979;8:360-2.  |
| 15. | Fatma O, Agop C, Emin U, Sidal M. Airway foreign bodies in childhood. Int J Pediatr Otorhinolaryngol 2000;52:11-6.  |
| 16. | Shraga B, Yehezkel N, Abraham F. Foreign bodies in the airway: A review of 200 cases. Am J Dis Child 1980;134:68-71.  |
| 17. | Singh B, Kantu M, Har E, Lucente FE. Complications associated with 327 foreign bodies of the pharynx, larynx and esophagus. Ann Otol Rhinol Laryngol 1997;106:301-4.  |
| 18. | Nabil A, Ohikuaiteme DA, Mustafa F, Hisham A, Sameeh SG. An unusual case of impacted esophageal foreign body. Saud Med J 2000;21:202-3.  |
| 19. | ASGE Standards of Practice Committee, Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc 2011;73:1085-91.  [ PUBMED] |
| 20. | Majori M, Fecci L, Monica M, Casalini AG. Airway foreign bodies. Monaldi Arch Chest Dis 2011;75:86-8.  |
| 21. | Nwaorgu OG, Onakoya PA, Sogebi OA, Kokong DD, Dosumu OO. Esophageal impacted dentures. J Natl Med Assoc 2004;96:1350-3.  |
| 22. | Keith MR. Esophageal foreign bodies. Am Fam Physician 2014;44:824-31.  |
| 23. | Al-Qudah A, Daradkeh S, Abu-Khalaf M. Esophageal foreign bodies. Eur J Cardiothorac Surg 1998;13:494-8.  |
| 24. | Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: A literature review of 12,979 cases. Anesth Analg 2010;111:1016-25.  |
[Table 1], [Table 2], [Table 3]
|