|
 
 |
| CASE REPORT |
|
| Year : 2016 | Volume
: 11
| Issue : 2 | Page : 59-61 |
|
Capillary hemangioma of the breast in a Sudanese child
Saadeldin Ahmed Idris1, Kamal Elzaki Elsiddig2
1 Department of Surgery, Faculty of Medicine, Alzaiem Alazhari University, Khartoum, Sudan
2 Department of Surgery, Faculty of Medicine, University of Khartoum, Khartoum, Sudan
| Date of Web Publication | 1-Jul-2016 |
Correspondence Address:
Saadeldin Ahmed Idris
Department of Surgery, Faculty of Medicine, Alzaeim Alazhari University. P.O. Box: 6691, Postal Code 11113, Khartoum
Sudan
  | Check |
DOI: 10.4103/1858-5000.185231 
Capillary hemangiomas of the beast in female children is a very rare pathology. In the literature, there are only three cases reported with this pathology. We report an 11 months girl presented with an enlarged left breast (or areola) and was initially diagnosed as a case of an inadequately treated neonatal mastitis, but later on, on performing an incisional biopsy it proved to be a capillary hemangioma. Keywords: Angiosarcoma, breast parenchyma, capillary hemangioma
How to cite this article:
Idris SA, Elsiddig KE. Capillary hemangioma of the breast in a Sudanese child. Sudan Med Monit 2016;11:59-61 |
| Introduction | |  |
Vascular tumors of the breast are very rare. Most can be classified as either benign lesions such as hemangiomas or malignant lesions such as angiosarcomas.[1],[2],[3] Angiosarcomas are more common than benign hemangiomas which are very rare.[4],[5]
We could find only three cases of capillary hemangioma of the female child breast in the literature.[6]
This paper reports a rare case of capillary hemangioma in a female child presents with breast mass disfiguring the nipple areola complex, successfully diagnosed by wedge biopsy and treated conservatively.
| Case Report | |  |
An 11-month-old Sudanese female child presents to the Surgery Department because of her parent's concern about the child's left breast. The child was noticed to have an abnormally large breast since she was 1 month of age. It was gradually increasing in size. However, the growth was rapid over the last 3 months preceding the presentation. This was associated with the appearance of a dark-red crust in the middle of the lump from time to time. At one stage, the condition was diagnosed as a case of chronic neonatal mastitis because of the long duration and unresponsive to several courses of antibiotics. On examination, all systems were found to be normal apart from a circumferentially enlarged areola on the left breast with a diameter of 4 cm. The skin of the areola was puckered and appeared darker than the normal right breast. There was an invagination at the center with a crust overlying it, resembling the crater of a volcano as shown in [Figure 1]. A wedge biopsy from the areola was performed and proven to be capillary hemangioma histopathologically as shown in [Figure 2] and [Figure 3]. Then after, the follow-up to 1 year showed no changes in the clinical feature of the swelling. | Figure 1: Circumferentially enlarged areola on the left breast with a diameter of 4 cm
Click here to view |
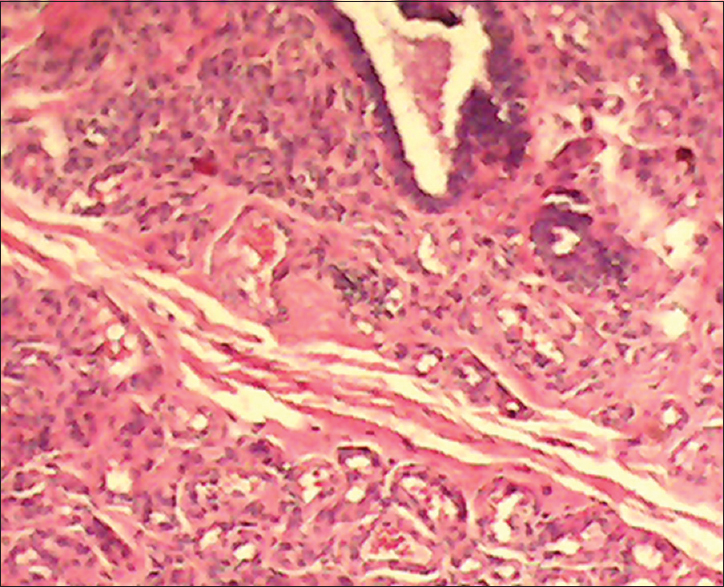 | Figure 2: Haemangioma of the breast showing breast ducts at the top right-hand corner with many blood vessels at the bottom of the figure (H and E, ×10)
Click here to view |
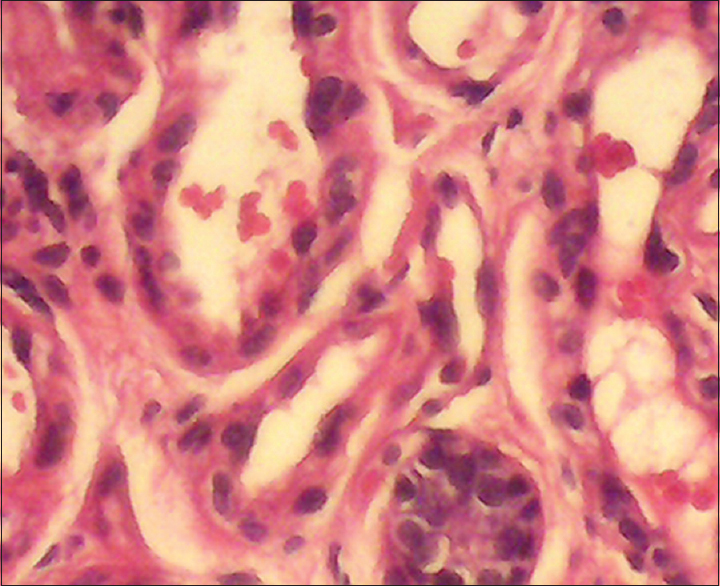 | Figure 3: Haemangioma of the breast showing several blood vessels and a duct of the breast at the bottom right-hand corner (H and E, ×40)
Click here to view |
| Discussion | |  |
Hemangiomas of the breast are subdivided into four types: Perilobular, parenchymal, nonparenchymal or subcutaneous, and venous. Perilobular hemangiomas always occur in the extralobular stroma in the form of microscopic lesions. Parenchymal or intraparenchymal hemangiomas are microscopically composed of dilated channels filled with red blood cells, and individual vessels of hemangiomas vary in size from capillary to cavernous. Venous hemangiomas are composed largely of venous channels with disorderly vascular proliferation.[4],[7] Nonparenchymal/extra-parenchymal or subcutaneous hemangiomas are located superficial to the anterior pectoral fascia in the subcutaneous fat with or without dermal involvement.[8],[9],[10] Both capillary and cavernous hemangiomas appear as thin walled, blood-filled vascular spaces, separated by fibrous septa, with extensive fibrosis, and sometimes phleboliths.[10]
Extraparenchymal vascular masses tend to occur in pediatric breast, and are generally benign,[6],[9],[10] responds well to simple excision,[6] whereas most intraparenchymal lesions tend to present in adult breast and prove to be malignant angiosarcomas.[6],[9],[10]
The term hemangioma was originally used to describe any vascular tumor both present around birth and/or appearing later in life. Mulliken and Glowacki [11] separated these conditions into a family of self-involuting tumors (growing lesions that eventually disappear) from the family of malformations (enlarged or abnormal vessels present at birth and essentially permanent). The importance of this separation is that it allows us to differentiate early in life between lesions that will resolve versus those that are permanent. Examples of permanent malformations include port-wine stains (capillary vascular malformation) and masses of abnormally swollen veins (venous malformations). In the literature, we do not see such separation system, creating great confusion.
The cause of hemangioma is currently unknown; however, several studies have suggested the importance of estrogen signaling in hemangioma proliferation. Kleinman et al.[12] in their study revealed that localized soft tissue hypoxia coupled with increased circulating estrogen after birth may be the stimulus. There is also a hypothesis concludes that maternal placental embolizes to the fetal dermis during gestation resulting in hemangioma genesis.[13],[14] So that, in genetic analyses of small nucleotide polymorphisms in hemangioma tissue compared to the mother's DNA that contradicted this notion.[15]
Both capillary and cavernous hemangiomas are benign vascular tumors of the endothelium so that even at an early stage, endothelial cells express phenotypic markers of mature endothelium, such as CD31, factor VII-related antigen, Ulex europaeus lectin I, and vascular endothelial cadherin (VE-cadherin).[16]
From literature, we found that capillary hemangioma of the breast parenchyma is a rare finding in the pediatric age group, and until recent time there are only three cases reported in the literature.[6]
In our case, the correct diagnosis could not be made preoperatively. Although mammary capillary hemangiomas are benign, radical surgery for complete excision is recommended to exclude the possibility of underlying malignant neoplasm. This is because some well-differentiated angiosarcomas are often difficult to differentiate from benign hemangiomas.[17]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Siewert B, Jacobs T, Baum JK. Sonographic evaluation of subcutaneous hemangioma of the breast. AJR Am J Roentgenol 2002;178:1025-7.  |
| 2. | Hoda SA, Cranor ML, Rosen PP. Hemangiomas of the breast with atypical histological features. Further analysis of histological subtypes confirming their benign character. Am J Surg Pathol 1992;16:553-60.  |
| 3. | Aurello P, Cicchini C, Mingazzini P. Hemangioma of the breast: An unusual lesion without univocal diagnostic findings. J Exp Clin Cancer Res 2001;20:611-3.  |
| 4. | Rosen PP, Jozefczyk MA, Boram LH. Vascular tumors of the breast. IV. The venous hemangioma. Am J Surg Pathol 1985;9:659-65.  |
| 5. | Mariscal A, Casas JD, Balliu E, Castellà E. Breast hemangioma mimicking carcinoma. Breast 2002;11:357-8.  |
| 6. | Nagar H, Marmor S, Hammar B. Haemangiomas of the breast in children. Eur J Surg 1992;158:503-5.  |
| 7. | Shousha S, Theodorou NA, Bull TB. Cavernous haemangioma of breast in a man with contralateral gynaecomastia and a family history of breast carcinoma. Histopathology 1988;13:221-3.  |
| 8. | Glazebrook KN, Morton MJ, Reynolds C. Vascular tumors of the breast: Mammographic, sonographic, and MRI appearances. AJR Am J Roentgenol 2005;184:331-8.  |
| 9. | Jozefczyk MA, Rosen PP. Vascular tumors of the breast. II. Perilobular hemangiomas and hemangiomas. Am J Surg Pathol 1985;9:491-503.  |
| 10. | Rosen PP. Vascular tumors of the breast. V. Nonparenchymal hemangiomas of mammary subcutaneous tissues. Am J Surg Pathol 1985;9:723-9.  |
| 11. | Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22.  |
| 12. | Kleinman ME, Greives MR, Churgin SS, Blechman KM, Chang EI, Ceradini DJ, et al. Hypoxia-induced mediators of stem/progenitor cell trafficking are increased in children with hemangioma. Arterioscler Thromb Vasc Biol 2007;27:2664-70.  |
| 13. | Barnés CM, Huang S, Kaipainen A, Sanoudou D, Chen EJ, Eichler GS, et al. Evidence by molecular profiling for a placental origin of infantile hemangioma. Proc Natl Acad Sci U S A 2005;102:19097-102.  |
| 14. | North PE, Waner M, Brodsky MC. Are infantile hemangiomas of placental origin? Ophthalmology 2002;109:633-4.  |
| 15. | Pittman KM, Losken HW, Kleinman ME, Marcus JR, Blei F, Gurtner GC, et al. No evidence for maternal-fetal microchimerism in infantile hemangioma: A molecular genetic investigation. J Invest Dermatol 2006;126:2533-8.  |
| 16. | Mulliken JB, Fishman SJ, Burrows PE. Vascular anomalies. Curr Probl Surg 2000;37:517-84.  |
| 17. | Page DL, Anderson TJ. Diagnostic Histopathology of the Breast. Edinburgh: Churchill Livingstone; 1987. p. 335-41.  |
[Figure 1], [Figure 2], [Figure 3]
|