|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2017 | Volume
: 12
| Issue : 1 | Page : 1-7 |
|
Fractional exhaled nitric oxide along with a reduced force expiratory volume are conclusive prognostic biomarkers to alert for asthma exacerbation
Mohamed Abdelrahman Mohamed Iesa1, Hiba A Awooda2, Emadeldin Hassan E Konozy3
1 Department of Physiology, Faculty of Medicine, Umm Al-Qura University, Al Qunfudhah, Makkah, Saudi Arabia
2 Department of Physiology, Faculty of Medicine, Al-Neelain University, Khartoum, Sudan
3 Biotechnology Park, Africa City of Technology, Khartoum, Sudan
| Date of Web Publication | 18-May-2017 |
Correspondence Address:
Mohamed Abdelrahman Mohamed Iesa
Department of Physiology, Faculty of Medicine, Umm Al-Qura University, P. O. Box: 203, Al Qunfudhah, Makkah 21912
Saudi Arabia
  | Check |
DOI: 10.4103/summ.summ_13_17 
Background: Asthma is a multidimensional disease with noticeable heterogeneity in its presentation and reaction to treatment. Noninvasive biomarkers to determine disease progression are highly desirable. This study sought to identify fractional exhaled nitric oxide (FeNO), FeNO as a prognostic biomarker for asthma exacerbations, as well as a predictive biomarker for change in other known asthma indicators. Materials and Methods: A prospective, longitudinal study was conducted with a cohort of adult patients with severe asthma who required daily treatment with inhaled corticosteroids. Patients underwent lung function testing using spirometry, sputum samples were taken for inflammatory cell count, and sputum supernatant and exhaled respiration were taken for FeNO, FeNO measurement. Forced expiratory volume levels were measured, along with immunoglobulin E (IgE), eosinophil count, asthma-specific health-related quality of life, asthma-exact signs scores, and time to treatment failure. These indicators were measured over the 22-week study period. Results: A total of 1800 participants were recruited, 56.7% were female, and 70% of the participants were aged 18–27 years. FeNO was valuable prognostic biomarker for asthma exacerbations, along with forced expiratory volume in 1 s reduction. A greater quantity of eosinophils was correlated with a reduced risk of exacerbation in females, with no correlation in males. Elevated serum IgE levels were correlated with an increased risk of lung fibrosis. We found no significant relationships between the investigated indicators and hospitalization. Conclusion: FeNO, in conjunction with other biomarkers, is a useful prognostic indicator of exacerbations of symptoms in asthma patients. Keywords: Asthma, biomarkers, force expiratory volume, fractional exhaled nitric oxide, validation
How to cite this article:
Iesa MA, Awooda HA, Konozy EH. Fractional exhaled nitric oxide along with a reduced force expiratory volume are conclusive prognostic biomarkers to alert for asthma exacerbation. Sudan Med Monit 2017;12:1-7 |
How to cite this URL:
Iesa MA, Awooda HA, Konozy EH. Fractional exhaled nitric oxide along with a reduced force expiratory volume are conclusive prognostic biomarkers to alert for asthma exacerbation. Sudan Med Monit [serial online] 2017 [cited 2018 Jul 22];12:1-7. Available from: http://www.sudanmedicalmonitor.org/text.asp?2017/12/1/1/206560 |
| Introduction | |  |
Asthma is a multidimensional disease with noticeable heterogeneity in its presentation and reaction to treatment. Therefore, there is an increasing need for useful biomarkers with predictive and prognostic value for the progression of the disease in asthmatic patients, and their link with clinical treatments. Fractional exhaled nitric oxide (FeNO), FeNO has been identified previously as a useful biomarker for asthmatic patients who will benefit from anti-interleukin-13 (IL-13) treatment,[1],[2] and while several studies have elucidated the role of FeNO in asthma-associated mechanisms, such as the regulation of goblet cell metaplasia,[3] and eosinophilic airway inflammation,[4] few have examined the use of FeNO as a prognostic indicator for asthma disease progression. In addition, while many studies have examined the usefulness of asthma biomarkers such as serum eosinophils count,[5] immunoglobulin E (IgE),[6],[7] and peripheral blood eosinophils,[8],[9] very few have explored any possible relationships between the various asthma indicators, and it is vague from the literature whether any of the biomarkers investigated dependably correlate with the severity of asthma symptoms.[10],[11]
FeNO has a strong connotation in severe asthma with airways eosinophilia.[12],[13] FeNO appearance in the expiratory air can be controlled by the significant T-helper 2 cytokines IL-4 and IL-13.[4],[14] FeNO has a character role in motivating the changing transforming growth factor-beta (TGF-β) nodding pathway connecting milieu metalloproteinase-2 and -9, with epithelial cells overexpressing FeNO causing TGF-β-dependent ooze of Type 1 collagen by airway fibroblasts.[15] FeNO of airways is related with an asthma phenotype determined by amplified countenance of IL-5 and IL-13, with high levels of serum IgE,[1] universal and lung eosinophilia, enlarged width of the reticular basement membrane, and sensitivity to steroids.[16],[17],[18] The associations among FeNO and harshness of asthma symptoms, fitness grade, and potential confounding factors, such as comorbidity, smoking status are unknown.[19],[20],[21]
Therefore, this study is focused on investigating the prognostic value of FeNO and other biomarkers in predicting asthma exacerbations, as well as any correlations between changes in these asthma biomarkers and indicators. The key objective of this study is to link the ratio of asthma exacerbations among patients with low standard FeNO levels (<50 ppb) and patients with high baseline FeNO levels (≥50 ppb), as found by laboratory testing, to additionally detecting of FeNO as a predictive biomarker that can diagnose asthmatic patients. The second key objective of this study consists of measuring the state and ability of FeNO (and further biomarkers unaccompanied and in combination with other biomarkers) to act as a predictive marker for change in other asthma indicators, such as forced expiratory volume in 1 s (FEV1) and modified asthma-specific health-related quality of life.
| Materials and Methods | |  |
This study was a continuing, prospective, longitudinal (single-arm), real ward study over 22 weeks of a cohort of mature patients with severe asthma. Approximately 1800 patients were initially enrolled, with 849 patients persisting to the end of the 22-week study time. [Table 1] shows the data description according to asthma diagnosis.
The study enrolled patients who were identified as having asthma and who required daily treatment with inhaled corticosteroids (ICS) (total daily dose of ≥600 mg of fluticasone propionate [FP] or equivalent) and a second control drug. A summary of the study scheme is shown in [Figure 1], with change of variables related to studied asthmatic patients in [Table 2].
The study involved patients 18 years old or above who have been identified and diagnosed as asthmatics in the chest clinics in the city of Sirte. The following diagnostic indicators were used to identify such patients: FEV1 of 30%–85% a familiar bronchodilator response (≥12% upgrading in FEV1 after bronchodilator use using spirometer) or a PC20 methacholine <8 mg on current treatment, with a whole daily dose of ≥500 mg of FP (or equal), and a minimum single additional controller drug as long-acting beta-2 agonist, leukotriene receptor antagonist, long-acting muscarinic antagonist, bronchophyllin, or oral corticosteroids (as Xelon syrup or prednisolone tabs). Patients who had worsened asthma symptoms in the last 6 months before arriving at the clinic were excluded from the study, as well as those who were current or ex-smokers (≥10 pack-years) to exclude chronic obstructive diseases.
Technique used to measure FeNO
Greatest inspiration was done over an absorber to guarantee nitric oxide (NO)-free air. The adult then achieved a meticulous exhalation using flow governor at an exhalation pressure of 4–10 cm H2O for at least 6 s, during which time tester collection and gas exploration and analysis were achieved. Three acceptable measurements (within 10%) were taken at the suggested flow rate of 50 mL/s within a 15 min period.
Venous blood obtained from the participants was fascinated on filter paper and eluted. Total IgE was articulated in international units per milliliter; radio allegro sorbent testing (RAST) results were expressed in RAST units per milliliter with one RAST unit representing approximately 2.4 ng of specific IgE. All test consequences were modified for definite quantities of plasma used in the tests, using serum albumin as a protein of reference. Eosinophil was detected using an automated hematology analyzer which is an automatic blood analyzer. The KX-21 performs speedy and accurate analysis of 18 parameters in blood and detects this including all white blood cells (WBCs) count with eosinophils.
The FeNO value of <25 ppl was selected on the basis of former Phase II. In that work, the median value of FeNO for all patients (25–50 pp) was used to define the point between the high-FeNO group and the low-FeNO group. For this study, an asthma exacerbation is defined according to the following protocol:
- For patients who are not on fixed dose of oral corticosteroid, exacerbation is defined as an increase or new occurrence of wheezing symptoms, cough, dyspnea, chest tightness, and/or nocturnal awakening due to these symptoms that leads to initiation of treatment with oral corticosteroids (for at least 3 days), or admission to hospital with at least one dose of intravenous or intramuscular corticosteroids
- For patients who are currently on oral corticosteroid therapy, it is defined as an increase or new occurrence of the above symptoms that leads to increased treatment with systemic corticosteroids ≥30 mg or 0.5 mg/kg for ≥3 sequential days or hospital admission.
The asthma indicators for which the use of FeNO as a predictive marker is being examined include comparative alteration of FEV1 with reference to the first exacerbation of asthma symptoms; alteration in eosinophils count; a change in asthma-specific health-related questionnaire as judged by the specialized pulmonologist according to the questionnaire guidelines; asthma-exact signs scores from day zero of the study to week 22; and time to treatment failure (TTF). TTF is defined in this study as asthma exacerbation requiring a clinically meaningful change in the standard of care asthma treatment as reported by the investigator and confirmed by chest physician.
The asthma questionnaire was presented to patients in the Arabic language as required. FEV1 was calculated using the typical systems for digital spirometry (spirolab III). The values of other well-known predictive biomarkers and analytical features were measured at the starting point of the study (i.e., blood eosinophil counts and serum IgE, and history of asthma exacerbations over the 12 months before the study), and their correlation with FeNO levels and asthma exacerbations throughout the study were equally evaluated. To govern the consequence of initial FeNO levels in different subsections of patients, the correlation of FeNO levels with the degree of asthma exacerbations in patients receiving initiative for asthma management which have been recorded to count 500–1000 mg FP, or advanced management in those patients who are on >1000 mg FP, was examined and investigated. The correlation between biomarkers and clinically significant changes in standard of care drugs and healthcare use, as stated by the investigator, was appraised throughout the study.
In addition, the link between an increase in biomarkers over the baseline measured at the start of the study and the rate of crucial asthma-related healthcare use (defined as hospital admission or emergency department admission, and/or clinic visits due to asthma and asthma-related symptoms) over the study period were examined. All treatments and medications taken through the study were noted, with medication type, generic and common name, treatment dates, dosage, and management timetable. Blood eosinophil counts and serum IgE points as determined both by the local laboratory, and the central laboratory in Sirte, were assessed. The baseline measurements were used for the identification and consideration of negative outcomes linked to the study actions, and single-medical events such as anaphylaxis, hypersensitivity reaction, infection, malignancy, diabetes, cataract, bone fracture or dental operations, and conditions of physiological hyperdynamic circulation such as pregnancy.
This study is designed to detect a clinically significant comparative alteration between high level of FeNO versus the low-FeNO group of outpatients chest clinic. About 849 patients persisting to the end of the 22 weeks study, to discard the null hypothesis at least 80% of those participants needed to show upsurge in grade of asthma exacerbations with the supposition of a normal rate of FeNO-low group.
For the initial analysis, the number of asthma exacerbations was related to the FeNO-high and FeNO-low groups as determined the test. The study included both reported and observed exacerbations, without including patients who left the study before the end. The comparative alteration in the exacerbation degree (between FeNO-high and FeNO-low groups) was valued by the exponential FeNO group reversion constant, and the FeNO group constant was used to map the change in exacerbation rate by the use of a probability ratio test statistic.
For secondary objectives, association between the other biomarkers mentioned and exacerbation rates, in addition to assessing the effect on exacerbation rates in each patient subgroup. Variations in biomarkers and lung events (FEV1/forced vital capacity [FVC]) were considered against time and standard FeNO (high versus low) covariates, by means of a varied effects model. The result of baseline FeNO (high versus low) on the period to first asthma exacerbation and TTF were analyzed by steer comparative risk distribution models, through clinically significant changes in regimen of asthma management, and variations in the degree of crucial asthma-correlated healthcare use were plotted by expressive statistics for each baseline FeNO group. The associations between FeNO, blood eosinophil count, serum IgE, and measured in patients following each appointment, were considered using Spearman's correlation coefficient. Additional measures of correlation/association between nominated biomarkers or risk issues (blood eosinophil count, serum IgE, and history of exacerbated asthma), and indicators such as degree of asthma exacerbations, FEV1, TTF, asthma-linked quality of life change (as assessed by the questionnaire), and asthma-connected healthcare use, were explored by pertinent use of data and statistical models, as described for the primary and secondary study objectives. Asthma-linked medicines and additional medicines unrelated to the study were logged throughout the study and were summarized by regular tables, both generally and by baseline FeNO group.
Actually, our result showed that there were significant relations among logarithm of FEV1 and logarithm IgE, blood eosinophil count, [Figure 2] and [Figure 3], respectively.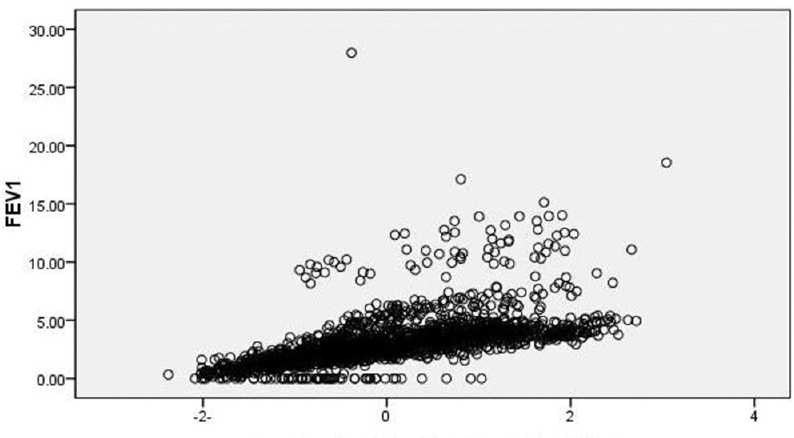 | Figure 2: Scatter plot while dependent variable id force expiratory rate in 1 s
Click here to view |
| Results | |  |
The distribution of serum FeNO morals was right skewed. The normal logarithm alteration clues to a more symmetric distribution [Figure 4]. Doctor-diagnosed asthma was observed in 659 (73.8%) out of 894 participants. The distribution of FeNO was again right skewed. [Figure 2] show distribution of FeNO in participants with high against low FVC1. The average is 49 (13.0–149) IU·L - 1 For serum IgE altitudes, in contributors who diagnosed as asthmatics and who were not diagnosed to be asthmatic, respectively. While for blood IgE in samples, the average was 0.3 (0.2–0.4) cells × 109·L -1 for both participants groups. There was a positive association between FeNO and (FEV1% predicted) as shown in our result and a weak positive relationship with functional residual capacity % predicted.
| Discussion | |  |
We poised sputum, did bronchoscopy, and harmonized outlying blood illustrations from 849 asthmatic patients who have been diagnosed to be server asthmatic by Sirte chest clinic those patients continued suggestive and symptomatic regardless of most gasped corticosteroid management (mean FEV1, 60% of expected rate). FeNO points are significantly amplified in asthmatic patients with sign of eosinophilic airway inflammation comparative to those with insignificant eosinophilic airway inflammation. A logistic deterioration model, counting gender, age, body mass index, IgE altitudes, blood eosinophil records in 759 patients out of 849 patients taken previously as severe asthmatic displayed that, of these directories, the FeNO level was the sole best prognosticator of airway eosinophilia (P = 0.007). There were no significant relationships between the investigated indicators and hospitalization. FeNO was useful as a prognostic biomarker for asthma exacerbations, along with FEV1 reduction. A greater quantity of eosinophils was correlated with a reduced risk of severe asthmatic outbreak in females; in males, no correlation was detected. Elevated serum IgE levels were correlated with an increased risk of lung fibrosis as seen by appearance of ground-glass opacity in chest computed tomography (CT) scans. This study was able to identify FeNO as a useful prognostic biomarker for asthma exacerbations, along with FEV1 reduction. This finding is in line with those of a newly stated Phase IIB clinical trial involving lebrikizumab;[2] this study differs in that it involves patients in clinical practice, and therefore may be more applicable in influencing the handling and treatment of patients, and ability to identify patients who may obtain an advantage from targeted treatment, and so may have consequences for the management of asthma patients.
A greater volume of FeNO was correlated with a reduced risk of severe asthmatic outbreak in females; in males, however, no correlation was detected. A similar inverse correlation of eosinophil count and asthma exacerbations was identified during the EXTRA study.[5] In that trial, the results of treatment with omalizumab in reducing asthma exacerbation were further marked using three biomarkers (blood eosinophils, FeNO) and a low eosinophil count (<300 cells/mL at baseline) resulting in omalizumab not reducing asthma exacerbations in patients.[5] In this study, elevated serum IgE levels were correlated with an increased risk of lung fibrosis, as seen by appearance of ground-glass opacity in chest CT scans. The usefulness of lone biomarkers as prognostic indicators has been seen in numerous experiments;[7],[10],[11] sputum eosinophil-directed management was linked to a decrease in asthma exacerbations in moderate-to-severe patients,[12] and plasma eosinophil total has been used to evaluate the effect of ICS tapering.[9],[13] In contrast to this, a meta-analysis of studies that used FeNO to adapt ICS handling did not display any advantage in decreasing the degree of asthma exacerbations.[14] In addition, in attempting to predict changes in the future lung function, a novel study identified a correlation between raised FeNO levels and a weakening in FEV1 in patients with asthma.[10] In another longitudinal study, elevated FeNO levels were also seen to be a predictive marker for FEV1 decline in asthmatic patients.[15] In this setting for patients with severe asthma, the goal of the study was to provide additional evidence for the usefulness and relevance of such biomarkers, both in isolation and when used in tandem, in clinical and scientific practice. However, while there were correlations between various biomarkers and asthma exacerbations, there were no significant relationships between the investigated indicators and hospitalization. It is notable, however, that many of the well-studied asthma biomarkers are related to paths of Type 2 inflammation facilitated by Type 2 cytokines. For instance, all of the biomarkers measured in this study can be related to Type 2-dependent mechanisms.[16] Eosinophils are inflammatory cells that may be found in large amounts in the respiratory airways and blood stream of patients with asthma. The maturation, movement, and presentation of eosinophils to areas of inflammation are organized by the Type 2 cytokines IL-5 and IL-13.[19] FeNO is formed by NO synthase, the appearance of which is determined by IL-13 and IL-4.[20] Hence, since all these biomarkers are related to Type-2 inflammation, and the levels of these biomarkers show a correlative relationship, Type 2 cytokines are therefore likely to be secreted in a consistent and interrelated manner rather than in a singular or individual fashion. This study data may be used to gain an indication into how widespread and consistent this correlation might be over time, and aid our understanding of how best to utilize the variety of available biomarkers in the real clinical setting, separate from the selection bias that can often be present in clinical trials, as well as offer us the chance to explore the likely value of using a compound biomarker in the medical evaluation of patients with asthma. Similar to this, the RASP-UK study group [21] is examining the predictive value of using FeNO and blood eosinophils as a combined biomarker to predict exacerbation risk in clinical trials of lebrikizumab and with omalizumab in patients maintained with ≥500 mg FP and an additional control. Initial results indicate that, individually, these biomarkers are all connected with exacerbation risk, but using the three biomarkers in a “composite” biomarker, they can be used as a more accurate indicator of exacerbation risk.[21]
A novel feature of this study is the opportunity to match the importance of measuring biomarkers at central and regional/local laboratories, and determining if discrepancies are amplified among different laboratories. This is of significant importance in countries such as Libya, where the impact of testing locally versus at a central laboratory on the results is not known. Specifically, it may help identify the most consistent and accurate method of eosinophil testing. The inconsistency of airway eosinophilia testing classically means that investigative and diagnostic accuracy are predisposed by clinical background and framework. This study highlights the importance of applying a coordinated and consistent methodology for the evaluation of biomarkers. Local laboratories make testing dependent on local events, and thus may make it challenging to relate and systematize results between sites. The contrast of local versus central testing of eosinophils has not before been examined and investigated, and this study may deliver some valuable insights.
Compliance with asthma treatment is of substantial concern in any study investigating asthma,[17] and in an effort to reduce the impact of this, the current study did not interfere with the treatment and management of the patients. The clinic visits carried out at the start of the study, and in weeks 11 and 22, as well as the telephone interviews carried out in weeks 6 and 16, allowed the relationships between the main biomarkers to be considered relative to the medical and clinical constraints of a real ward situation. Withdrawal rates may be a challenge for a long-term, noninterventional study, such as this one. To overcome this factor, an allowance for a 30% dropout rate has been included in the study design, while still maintaining an adequate sample size. However, it must also be carefully considered that allowing patients to change treatment during the study, according to the investigator's standard practice and discretion, should limit withdrawal rates.
| Conclusion | |  |
FeNO was useful as a prognostic biomarker for asthma exacerbations, along with FEV1 reduction. An increase in eosinophil count was correlated with a reduced risk of a severe asthmatic outbreak in females, and elevated serum IgE levels were correlated with an increased risk of lung fibrosis and therefore may be other candidates for prognostic indicators. To ensure the validity of these findings, further multicenter studies involving large numbers of patients should be performed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | American Thoracic Society; European Respiratory Society. ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med 2005;171:912-30.  [ PUBMED] |
| 2. | Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, et al. An official ATS clinical practice guideline: Interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med 2011;184:602-15.  [ PUBMED] |
| 3. | Barnes PJ, Dweik RA, Gelb AF, Gibson PG, George SC, Grasemann H, et al. Exhaled nitric oxide in pulmonary diseases: A comprehensive review. Chest 2010;138:682-92.  [ PUBMED] |
| 4. | Ricciardolo FL. Multiple roles of nitric oxide in the airways. Thorax 2003;58:175-82.  [ PUBMED] |
| 5. | Smith AD, Cowan JO, Filsell S, McLachlan C, Monti-Sheehan G, Jackson P, et al. Diagnosing asthma: Comparisons between exhaled nitric oxide measurements and conventional tests. Am J Respir Crit Care Med 2004;169:473-8.  [ PUBMED] |
| 6. | Pavord ID, Martin N. Will exhaled nitric oxide monitoring become routine in managing asthma? Expert Rev Respir Med 2009;3:107-11.  [ PUBMED] |
| 7. | Jacinto T, Alving K, Correia R, Costa-Pereira A, Fonseca J. Setting reference values for exhaled nitric oxide: A systematic review. Clin Respir J 2013;7:113-20.  [ PUBMED] |
| 8. | Leon de la Barra S, Smith AD, Cowan JO, Peter Herbison G, Robin Taylor D. Predicted versus absolute values in the application of exhaled nitric oxide measurements. Respir Med 2011;105:1629-34.  [ PUBMED] |
| 9. | Olivieri M, Talamini G, Corradi M, Perbellini L, Mutti A, Tantucci C, et al. Reference values for exhaled nitric oxide (reveno) study. Respir Res 2006;7:94.  [ PUBMED] |
| 10. | Maestrelli P, Ferrazzoni S, Visentin A, Marian E, Dal Borgo D, Accordino R, et al. Measurement of exhaled nitric oxide in healthy adults. Sarcoidosis Vasc Diffuse Lung Dis 2007;24:65-9.  [ PUBMED] |
| 11. | Olin AC, Bake B, Torén K. Fraction of exhaled nitric oxide at 50 mL/s: Reference values for adult lifelong never-smokers. Chest 2007;131:1852-6.  |
| 12. | Taylor DR, Mandhane P, Greene JM, Hancox RJ, Filsell S, McLachlan CR, et al. Factors affecting exhaled nitric oxide measurements: The effect of sex. Respir Res 2007;8:82.  [ PUBMED] |
| 13. | Travers J, Marsh S, Aldington S, Williams M, Shirtcliffe P, Pritchard A, et al. Reference ranges for exhaled nitric oxide derived from a random community survey of adults. Am J Respir Crit Care Med 2007;176:238-42.  [ PUBMED] |
| 14. | Dressel H, de la Motte D, Reichert J, Ochmann U, Petru R, Angerer P, et al. Exhaled nitric oxide: Independent effects of atopy, smoking, respiratory tract infection, gender and height. Respir Med 2008;102:962-9.  [ PUBMED] |
| 15. | Levesque MC, Hauswirth DW, Mervin-Blake S, Fernandez CA, Patch KB, Alexander KM, et al. Determinants of exhaled nitric oxide levels in healthy, nonsmoking African American adults. J Allergy Clin Immunol 2008;121:396-402.e3.  |
| 16. | Habib SS, Abba AA, Al-Zoghaibi MA, Subhan MM. Reference range values of fractional exhaled nitric oxide in healthy Arab adult males. Saudi Med J 2009;30:1395-400.  [ PUBMED] |
| 17. | Ko FW, Leung TF, Wong GW, Chu JH, Sy HY, Hui DS. Determinants of, and reference equation for, exhaled nitric oxide in the Chinese population. Eur Respir J 2013;42:767-75.  [ PUBMED] |
| 18. | See KC, Christiani DC. Normal values and thresholds for the clinical interpretation of exhaled nitric oxide levels in the US general population: Results from the National Health and Nutrition Examination Survey 2007-2010. Chest 2013;143:107-16.  [ PUBMED] |
| 19. | Matsunaga K, Hirano T, Kawayama T, Tsuburai T, Nagase H, Aizawa H, et al. Reference ranges for exhaled nitric oxide fraction in healthy Japanese adult population. Allergol Int 2010;59:363-7.  [ PUBMED] |
| 20. | Gelb AF, George SC, Camacho F, Fraser C, Flynn Taylor C, Shakkottai S. Increased nitric oxide concentrations in the small airway of older normal subjects. Chest 2011;139:368-75.  [ PUBMED] |
| 21. | Zhang YM, Lin JT. Normal values and influencing factors of fractional exhaled nitric oxide for Chinese healthy adults. Zhonghua Yi Xue Za Zhi 2012;92:1971-3.  [ PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1], [Table 2]
|