|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2017 | Volume
: 12
| Issue : 1 | Page : 25-29 |
|
Wheezing alone is not enough to validate asthma diagnosis among Libyan adults: A questionnaire-based study reinforced with pulmonary function test
Mohamed Abdelrahman Mohamed Iesa1, Hiba A Awooda2, Emadeldin Hassan E Konozy3, Omer Abdel Aziz Musa4
1 Department of Physiology, Faculty of Medicine, Umm Al-Qura University, Al Qunfudhah, Makkah, Saudi Arabia
2 Department of Physiology, Faculty of Medicine, Alneelain University, Khartoum, Sudan
3 Biotechnology Park, Africa City of Technology, University Avenue, Khartoum, Sudan
4 Department of Physiology, Faculty of Medicine, The National Ribat University, Khartoum, Sudan
| Date of Web Publication | 18-May-2017 |
Correspondence Address:
Mohamed Abdelrahman Mohamed Iesa
Department of Physiology, Faculty of Medicine, Omm Al-Qura University, P. O. Box: 203, Al Qunfudhah, Makkah 21912
Saudi Arabia
  | Check |
DOI: 10.4103/summ.summ_12_17 
Background: Asthma remains an increasing cause of morbidity and mortality in adults, especially in developing nations. In Libya, no previous study has reported the diagnosis of asthma among adults. The primary objective of this work is to validate the diagnosis of asthma through a survey questionnaire for adult Libyans, by using a digital spirometer as a recommendation to diagnose asthma. The specific objective of this study included the search for a correlation between asthma symptoms and its diagnosis. Materials and Methods: An adapted International Study of Asthma and Allergies in Childhood questionnaire was distributed to 1800 participants >18 years. Results: Females comprised 56.7% of the sample. Pulmonary function tests (spirometry) were performed on respondents who reported wheezing and chest tightness at rest and during daily activity. Approximately, 17.6% of the participants reported having wheezes during the past 12 months, while 18.4% had chest tightness at rest and during daily activities. A significant correlation was found between wheezing and chest tightness (P < 0.001). About 44% of the participants showed a positive reversibility test. Conclusion: Chest tightness at rest and wheezing are more reliable for diagnosing asthma. The city of Sirte in Libya requires the establishment of the common pollens which trigger asthma. Keywords: Asthma, Libyan, spirometry, wheezing
How to cite this article:
Iesa MA, Awooda HA, Konozy EH, Musa OA. Wheezing alone is not enough to validate asthma diagnosis among Libyan adults: A questionnaire-based study reinforced with pulmonary function test. Sudan Med Monit 2017;12:25-9 |
How to cite this URL:
Iesa MA, Awooda HA, Konozy EH, Musa OA. Wheezing alone is not enough to validate asthma diagnosis among Libyan adults: A questionnaire-based study reinforced with pulmonary function test. Sudan Med Monit [serial online] 2017 [cited 2018 Jul 22];12:25-9. Available from: http://www.sudanmedicalmonitor.org/text.asp?2017/12/1/25/206559 |
| Introduction | |  |
Asthma is an ancient respiratory disease where patients experience profound and difficult breathing. This was noted by Hippocrates, who described these patients to be asthmatic. The word “asthma” was labeled by the Greeks, meaning panting.[1] Because bronchial asthma is a heterogeneous condition, a widely acceptable definition is still used to define asthma; some of these definitions have been used since 1995. An overlap exists between asthma and bronchial hyperreactivity, and physicians face difficulties in diagnosing asthma as hyperreactivity could present in many people who do not have asthma.[2] At the same time, some milder forms of asthma could be missed and diagnosed as hyperreactivity. To avoid these limitations, many studies and guidelines now use questionnaires to diagnose asthma. The diagnosis of asthma is largely a clinical one because it involves heterogeneous symptoms and conditions, some of which are personal, while others may be related to the patient's family and medical history.[3] When making a diagnosis of bronchial asthma, physicians should bear the International Consensus Report definition of asthma in mind. Spirometry is used to measure lung function by estimating air flow.[3],[4] It is a useful device to diagnose obstructive lung diseases such as asthma. Similar to most North African countries, the prevalence of asthma in Libya is not exactly known. In fact, there is no precise way to define asthma in our population.[1] The International protocol to study Asthma and Allergies among Childhood (ISAAC) has been put forward and legislated by the International Society for Augmentative and Alternative Communication (ISAAC) who is responsible for improving the lives of children and adults. The society had also worked on revealing to educate public global society of the warning signs and symptoms in some North African countries; however, this study did not include Libya.[4] In Libya, no study has investigated the prevalence of asthma in adults.
Many factors are believed to either cause or exacerbate bronchial asthma, especially in young adults and children.[5],[6] In fact, asthma and allergy are common conditions with complex and heterogeneous etiologies.[7],[8] Asthma and allergic disease often co-occur in the same individual or in different individuals within the same family. However, there is still debate about whether this co-occurrence reflects distinct conditions with shared pathogenic pathways or different clinical manifestations of the same disease. Some studies, however, have challenged the assumption that childhood asthma was largely of allergic etiology.[9],[10] The primary objective of this study is to validate the diagnosis of asthma through a questionnaire and supportive supplementary pulmonary function tests among Libyan adults in Sirte City. The specific objective of this study included the search for a correlation between asthma symptoms and its diagnosis.
| Materials and Methods | |  |
This cross-sectional study was performed to validate asthma diagnosis by pulmonary function tests using the modified ISAAC questionnaire for adults among Libyans aged 18–60 years visiting the Sirte Chest Clinic in Sirte, Libya. A digitalized spirometer (Spirolab III)[3],[11] was used to validate pulmonary function among all participants who reported symptoms of asthma. A total of 2000 participants were targeted. Of these, 1800 responded to the questionnaire, representing a response rate of 90%. Participants were recruited provided they were aged >18 years, Libyan nationals, and residents of Sirte for more than 1 year. Patients with other obstructive lung diseases, such as chronic obstructive pulmonary disease, were excluded from the study. A questionnaire was distributed to all patients who visited Sirte Chest Clinic between January 1 and July 2, 2015. The questionnaire captured patients' data, asthma symptoms, allergy symptoms, and environmental issues. Spirolab III was used to test pulmonary function in patients assumed to have asthma. The data were analyzed using IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA). Results are presented in tables and significance was set at P < 0.05. The test was applied in either a standing or a sitting position. Forced expiratory volume in one second, forced vital capacity, and peak expiratory flow rate were measured and recorded before inhalation of bronchodilator (prevalues).
| Results | |  |
A total of 1800 participants were recruited. Of these, 56.7% were female (n = 1021). The majority of the participants were aged 18–27 years (n = 1333; 74.1%). In the past 12 months, 316 respondents (17.8%) reported having wheezes [Table 1]. In addition, patients with allergic rhinitis were significantly more likely to have wheezes. Factors which triggered allergic rhinitis, such as perfumes, positively correlated with wheezes in the past 12 months (P = 0.036). Furthermore, 33% of the participants with allergic rhinitis experienced wheezing during winter [Figure 1]. House dust was found to be the most important triggering factor (41.4%). Seasonal distribution of symptoms was found to be highest in winter [Figure 2].
Reversibility testing
Of the 320 participants who had wheezing, 34 declined the spirometry test, and of the remaining 287 participants, 127 (44%) had a positive reversibility test. One hundred and sixty patients (56%) had a negative response to reversibility testing.
- Reversibility test results for patients who complained of wheezing: Reversibility testing was performed in 287 participants, and the results are summarized in [Table 2]
- Correlation between reversibility testing and demographic data among patients with wheezing:
No correlation was found between reversibility testing and a history of wheezing in the past 12 months (P = 0.409), gender (P = 0.164), or age (P = 0.231). Spirometry test results were positive in 41.3% of the participants who reported wheezing in the past 12 months. Among participants with positive reversibility test results, females comprised 24% of the sample versus 20% for males - Correlation between wheezing in the past 12 months and other asthma symptoms:
There was a statistically significant correlation between wheezing in the past 12 months and at least five other asthma symptoms [P < 0.05; [Table 3] - Indoor and outdoor factors which seem to predispose to wheezing: A Chi-square test showed that indoor or outdoor smolder and house cockroaches were significantly correlated with wheezing in the past 12 months [Table 4]
- Family history of asthma as a risk factor for wheezing:
A family history of asthma was not statistically correlated with wheezing in the past 12 months (P = 0.082) - Correlation between reversibility testing and a combination of asthma symptoms (wheezing + other symptoms):
Although there was no statistically significant correlation between positive reversibility testing and wheezing alone (P > 0.05), there was a statistically significant correlation when wheezing was combined with shortness of breath that awakened the patient at night (P = 0.027) and nocturnal cough (P = 0.001).
| Discussion | |  |
This study demonstrated that wheezing alone is not enough to confirm a diagnosis of asthma. The objective of this study was to confirm and validate the diagnosis of asthma using the modified ISSAC survey questionnaire combined with lung function tests. According to the ISAAC protocol, a diagnosis of asthma was only based on patients' reports of wheezing in the past 12 months. However, no confirmatory test such as spirometry was used, contrary to our study. The ISSAC protocol showed a high prevalence of asthma symptoms in Sudanese children compared to children in other African countries (12.5%).[6] In our study, participants who had reported wheezing were subjected to lung function tests by spirometry. A pulmonary function test is an essential component of asthma diagnosis. In this study, wheezing was considered the predominant symptom. The prevalence of wheezing in the past 12 months was 17.6%, and the frequency of other asthma symptoms ranged between 7% and 28%. There are no published data of asthma in Libya, but the prevalence of wheezing in adults reached 3.4%–3.9% in three Maghreb countries, including Algeria, Morocco, and Tunisia.[5] Asthma prevalence among children, based on the ISAAC questionnaire, ranged between 5% and 19% in 2008 in Algeria, Morocco, and Tunisia.[5] A previous study conducted in Algeria by Adeloye D et al.[6] showed that asthma was emerging as a public health problem in middle-income persons, with an incidence of 800 cases per 100,000 population. In Sudan, the prevalence of asthma in 2007 was 13%.[11] In this study, reversibility testing was positive in 33 (44%) and negative in 42 (56%) of 75 symptomatic participants. Most of the participants in this study who complained of wheezing showed a positive correlation with other asthma symptoms. However, wheezing alone was not found to be reliable as an indicator of asthma symptoms,[12] contrary to our expectation. Reversibility testing was performed in patients who had at least one other symptom in addition to wheezing (wheezing plus shortness of breath that awakened the patient at night or wheezing plus nocturnal cough). Our finding that allergic rhinitis was significantly correlated with wheezing is consistent with those reported by other authors.[13],[14] Based on our questionnaire data, we identified two major triggering factors, including indoor and outdoor smolder and house cockroaches, which are well documented in the literature.[15]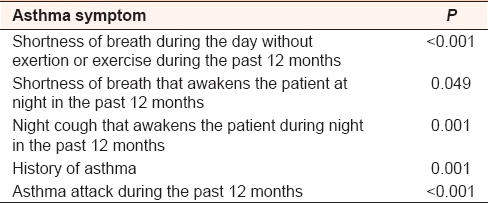 | Table 3: Correlation between wheezing in the past 12 months and other asthma symptoms
Click here to view |
| Conclusion | |  |
The prevalence of asthma symptoms among adults in Sirte using the modified ISSAC questionnaire was 17.6%, which is comparable with findings reported in other North African countries; however, when validated by pulmonary function tests, the prevalence was only 6.9%. Reversibility testing alone and the presence of one symptom (wheezing) might not be enough to reach a diagnosis of asthma among adult patients. Therefore, a large-scale study with more tests is warranted. Furthermore, we believe that two symptoms should be considered reliable to reach a diagnosis of asthma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Kim YM, Kim YS, Jeon SG, Kim YK. Immunopathogenesis of allergic asthma: More than the th2 hypothesis. Allergy Asthma Immunol Res 2013;5:189-96.  [ PUBMED] |
| 2. | Athanazio R. Airway disease: Similarities and differences between asthma, COPD and bronchiectasis. Clinics (Sao Paulo) 2012;67:1335-43.  [ PUBMED] |
| 3. | Canova C, Heinrich J, Anto JM, Leynaert B, Smith M, Kuenzli N, et al. The influence of sensitisation to pollens and moulds on seasonal variations in asthma attacks. Eur Respir J 2013;42:935-45.  [ PUBMED] |
| 4. | Schermer TR, Crockett AJ, Poels PJ, van Dijke JJ, Akkermans RP, Vlek HF, et al. Quality of routine spirometry tests in Dutch general practices. Br J Gen Pract 2009;59:e376-82.  [ PUBMED] |
| 5. | Prieto Centurion V, Huang F, Naureckas ET, Camargo CA Jr., Charbeneau J, Joo MJ, et al. Confirmatory spirometry for adults hospitalized with a diagnosis of asthma or chronic obstructive pulmonary disease exacerbation. BMC Pulm Med 2012;12:73.  |
| 6. | Adeloye D, Chan KY, Rudan I, Campbell H. An estimate of asthma prevalence in Africa: A systematic analysis. Croat Med J 2013;54:519-31.  [ PUBMED] |
| 7. | American College of Chest Physicians. American Thoracic Society: Pulmonary terms and symbols. Chest 1975;67:583.  |
| 8. | Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. November 1986. Am Rev Respir Dis 1987;136:225-44.  [ PUBMED] |
| 9. | Ben Abdallah FC, Taktak S, Chtourou A, Mahouachi R, Kheder AB. Burden of chronic respiratory diseases (CRD) in Middle East and North Africa (MENA). World Allergy Organ J 2011;4 1 Suppl:S6-8.  |
| 10. | Burney PG, Chinn S, Britton JR, Tattersfield AE, Papacosta AO. What symptoms predict the bronchial response to histamine? Evaluation in a community survey of the bronchial symptoms questionnaire (1984) of the International Union Against Tuberculosis and Lung Disease. Int J Epidemiol 1989;18:165-73.  [ PUBMED] |
| 11. | El Sony AI, Chiang CY, Malik E, Hassanain SA, Hussien H, Khamis AH, et al. Standard case management of asthma in Sudan: A pilot project. Public Health Action 2013;3:247-52.  [ PUBMED] |
| 12. | Wang J, Li B, Yu W, Yang Q, Wang H, Huang D, et al. Rhinitis symptoms and asthma among parents of preschool children in relation to the home environment in Chongqing, China. PLoS One 2014;9:e94731.  [ PUBMED] |
| 13. | Schmidt M. Not all wheezing is asthma: On functional laryngospasm. Pneumologie 1993;47:439-42.  [ PUBMED] |
| 14. | Lim FL, Hashim Z, Than LT, Md Said S, Hisham Hashim J, Norbäck D. Asthma, airway symptoms and rhinitis in office workers in Malaysia: Associations with house dust mite (HDM) allergy, cat allergy and levels of house dust mite allergens in office dust. PLoS One 2015;10:e0124905.  |
| 15. | Lee YL, Lin YC, Hsiue TR, Hwang BF, Guo YL. Indoor and outdoor environmental exposures, parental atopy, and physician-diagnosed asthma in Taiwanese schoolchildren. Pediatrics 2003;112:e389.  [ PUBMED] |
[Figure 1], [Figure 2]
[Table 1], [Table 2], [Table 3], [Table 4]
|