| |


 |
| Year : 2014 | Volume
: 8
| Issue : 4 | Page : 107-113 |
|
|
|
|
|
ORIGINAL ARTICLE Assessment of function in patients with rotator cuff tears: Functional test versus self-reported questionnaire
Selda Basar1, Seyit Citaker1, Ulunay Kanatli2, Burak Yagmur Ozturk3, Sadettin Kilickap4, Nihan K Kafa1
1 Department of Physiotherapy and Rehabilitation, Faculty of Health Sciences, Nigde, Turkey
2 Department of Orthopedics and Traumatology, Faculty of Medicine, Gazi University, Nigde, Turkey
3 Department of Orthopedics and Traumatology Clinic, Nigde State Hospital, Nigde, Turkey
4 Department of Preventive Oncology, Faculty of Medicine, Hacettepe University, Ankara, Turkey
Correspondence Address:
Selda Basar
Muammer Yasar Bostanci Cad, Emniyet Mah., No: 16, Besevler, Ankara
Turkey
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.145249

|
|
|
|
| Date of Web Publication | 21-Nov-2014 |
 Abstract Abstract | | |
Purpose: The rotator cuff tears (RCT) are a well-known cause of shoulder pain and loss of upper extremity function. The purpose of this study was to evaluate the upper extremity function using two different methods in patients with RCT and to determine the parameters that influence the upper extremity function.
Materials and Methods: A sample of 38 patients (27-76 years; 10 men and 28 women) who were diagnosed with a chronic full-thickness RCT, confirmed by magnetic resonance imaging (MRI), was studied. Upper extremity function was determined using Western Ontario Rotator Cuff Index (WORC) and 9 Hole Peg Test (9PEG). Other assessments included active range of motion (ROM), muscle strength, shoulder pain, and scapular dyskinesis.
Results: There was a weak association between WORC scores and 9PEG. A statistically significant, negative relationship was found between 9PEG and ROM in supination, as well as muscle strength of shoulder extensors, adductors, internal and external rotators.
Conclusions: In addition to the weak association between WORC and 9PEG, the difference between the parameters related to each method suggests that they should not be used interchangeably to determine the upper extremity function. We recommend the utilization of 9PEG instead of WORC in assessing the upper extremity function in the setting of loss of muscle strength.
Level of Evidence: Level IV, Therapeutic study.
Keywords: 9 Hole Peg Test, function, rotator cuff tear, upper extremity, Western Ontario Rotator Cuff Index
How to cite this article:
Basar S, Citaker S, Kanatli U, Ozturk BY, Kilickap S, Kafa NK. Assessment of function in patients with rotator cuff tears: Functional test versus self-reported questionnaire. Int J Shoulder Surg 2014;8:107-13 |
 Introduction Introduction | |  |
Rotator cuff tears (RCT) are a common problem causing shoulder pain and loss of upper extremity function. Several factors such as pain, tissue injury, muscle strength and limited range of motion (ROM) may influence the overall upper extremity function. [1],[2]
The most commonly administered outcome tools in patients with RCT have been reported as the American Shoulder and Elbow Surgeons (ASES), Disabilities of the Arm, Shoulder, and Hand (DASH) Questionnaire, Shoulder Pain and Disability Index (SPADI) and Simple Shoulder Test. [3] Although the psychometric features of these measures are appropriate for clinical use, absolute standard error has to be re-evaluated during the measurement of some parameters. Not only are these measures focused on a relatively small number of clinical parameters, but they also lack the sensitivity to detect subtle clinical differences. [4] Therefore, it was suggested that these self-reported outcome measures are not adequate for determining the functional status and disability. [5] In a recent review, including 38 shoulder-specific outcome questionnaires, it was pointed out that no gold standard exists among these measures in terms of determining shoulder function precisely. [6]
In the majority of the previous studies, the upper extremity function was determined by the use of self-reported questionnaires in patients with RCT. There only exist a few methods in the literature that evaluate the upper extremity function based on performance, and this group includes FIT-HaNSA, 9 Hole Peg Test (9PEG) and Purdue Pegboard. [4],[7],[8] Some of the recent studies have focused on determining the upper extremity function with one of these objective methods in different patient populations. For this purpose, FIT-HaNSA has been utilized in several shoulder pathologies, as well as in healthy shoulders. [9],[10]
In this study, 9PEG was used to determine the upper extremity function objectively. In addition, Western Ontario Rotator Cuff Index (WORC) was used as an outcome measure to determine the condition-specific functional status and to gather comparative data. The WORC index is a valid and reliable 21-question outcome measurement tool with each question scored 0-100 (maximum raw score 2100, then scaled to 100). [11] Its validation was performed using the University of California at Los Angeles Shoulder Scale, ASES Index, DASH index, and SF-36. [12] Pursuit analyzed include physical symptoms (6 items), sports and recreation (4 items), work (4 items), lifestyle (4 items), and emotions (3 items). [11]
9 Hole Peg Test is a standardized, validated method with normative values in a wide age range that is widely administered to determine the hand and upper extremity function in patients with RCT, as well as healthy adults. [7],[13],[14],[15] It involves picking up nine pegs from the holes one at a time and placing them in until all nine holes are filled. It is a practical, performance-based clinical tool that is used to evaluate the upper extremity function in different patient groups. [16],[17]
The purpose of this study was to evaluate the upper extremity function in patients with RCT by two different methods (WORC and 9PEG) and to determine the parameters that have influence on each method. We hypothesized that there would be no significant association between these methods and therefore, it would not be appropriate to use them interchangeably to determine the upper extremity function, particularly in the group of patients with loss of muscle strength. Simultaneously, the answer of the following questions will be sought in this study:
- Are the WORC and 9PEG alternatives of each other?
- May WORC determine ROM losses and shoulder muscle strength weakness itself?
 Materials and Methods Materials and Methods | |  |
This study was approved and performed in accordance with the guidelines of the institutional review board at our university, and all patients gave written informed consent to participate in the study beforehand. A sample of 38 patients (mean age, 53.93 ± 10.87 years [range, 43.06-64.8]; mean height, 1.72 ± 0.10 m; mean mass, 72.53 ± 12.78 kg; 10 men and 28 women) with a diagnosis of chronic (>3 months) full-thickness RCT was enrolled in the study (between the years 2011 and 2012). The educational breakdown of patients included 18 university/high school graduates (48.1%), 17 primary school graduates (44%) and 3 illiterate patients (7.9%). 26 patients (68.4%) were housewives while the rest had different occupations. Patient demographics is shown in [Table 1].
Inclusion criteria were full-thickness RCT causing typical signs and symptoms associated with shoulder impingement and rotator cuff tendinopathy for 3 months or more. Patients were excluded if they exhibited any neurologic condition resulting in muscle weakness or decreased ROM had a history of prior shoulder surgery and rheumatoid arthritis. Other exclusion criteria were acute RCT; bilateral RCT; glenohumeral joint osteoarthritis and adhesive capsulitis.
Radiological assessment
The tear sizes were classified according to the system described by Cofield et al. [18] Involvement and retraction of the rotator cuff tendons were assessed with the standard, noncontrast coronal, axial and sagittal MRI sequences, as described by Boileau et al. [19] The presence of humeral head migration was evaluated on true anteroposterior shoulder radiographs (positive if acromiohumeral distance >7 mm). [20] The fatty degeneration of the rotator cuff musculature was graded on the system described by Goutallier et al. [21] The presence of cystic changes in rotator cuff footprint (major and minor tuberosities) was also recorded based on MRI findings.
Upper extremity function
Upper extremity function was determined by 9PEG and WORC. [7],[22] The patients were asked to complete the WORC form depending on their quality of life in last 2 weeks. For 9PEG, the patients were asked to pick up the pegs with their affected side and place them in the holes, while holding the board with their unaffected side. The elapsed time was recorded in seconds.
Range of motion
Active shoulder flexion, extension, internal and external rotation as well as elbow flexion and extension were measured in the supine position, while active shoulder elevation was measured in the standing position with a universal goniometer.
Muscle strength
The muscle strength of shoulder flexor, extensor, internal and external rotators, abductor and adductors (with arm in neutral adduction and elbow in 90° flexion), and elbow flexor and extensors were measured with a digital hand dynamometer (Baseline® ) according to the criteria of American Academy of Orthopedic Surgeons. Supraspinatus muscle strength was determined in full can position. [23] Hand grab strength was measured with a hand dynamometer (Baseline® ), while triple and lateral finger grab strength were measured with a pinchmeter (Baseline® ) in the standard position proposed by American Society of Hand Therapists.
Pain
Patients were asked to mark their current shoulder pain on a visual analog scale (range from 0 to 10). They rated their pain at rest, at night, while carrying 2-3 kg packages and in shoulder elevation >90°.
Scapular dyskinesis
Scapular dyskinesis was assessed by observation during bilateral shoulder elevation, according to the classification described by Kibler and Sciascia. [24]
Statistical analysis
Overall summary statistics were assessed for normality and the means and standard deviations were calculated for continuous variables. Frequencies and percentages were calculated for categorical variables. Scapular dyskinesis, cysts, retraction and migration were categorized as present or absent, and tear size as small or large, tear extension as involving one or more tendons, and atrophy as absent, moderate or severe. Group differences among discrete variables were evaluated using Mann-Whitney U-test or Kruskal-Wallis test. Group differences for continuous variables were evaluated using Spearman test. All tests were evaluated using two-sided hypothesis testing with statistical significance set to α = 0.05. Calculations were performed using PASW version 18 (formerly SPSS Software, Chicago, IL).
 Results Results | |  |
Question 1
There was a weak association between WORC scores (average ± minimum-maximum, 26.5 ± 8.9-100) and 9PEG (average ± minimum-maximum, 20.9 ± 15-28), which was not statistically significant (r: 0.299, P: 0.076) [Table 2].
Question 2
The correlation of parameters pertaining to WORC and 9PEG is listed in [Table 3].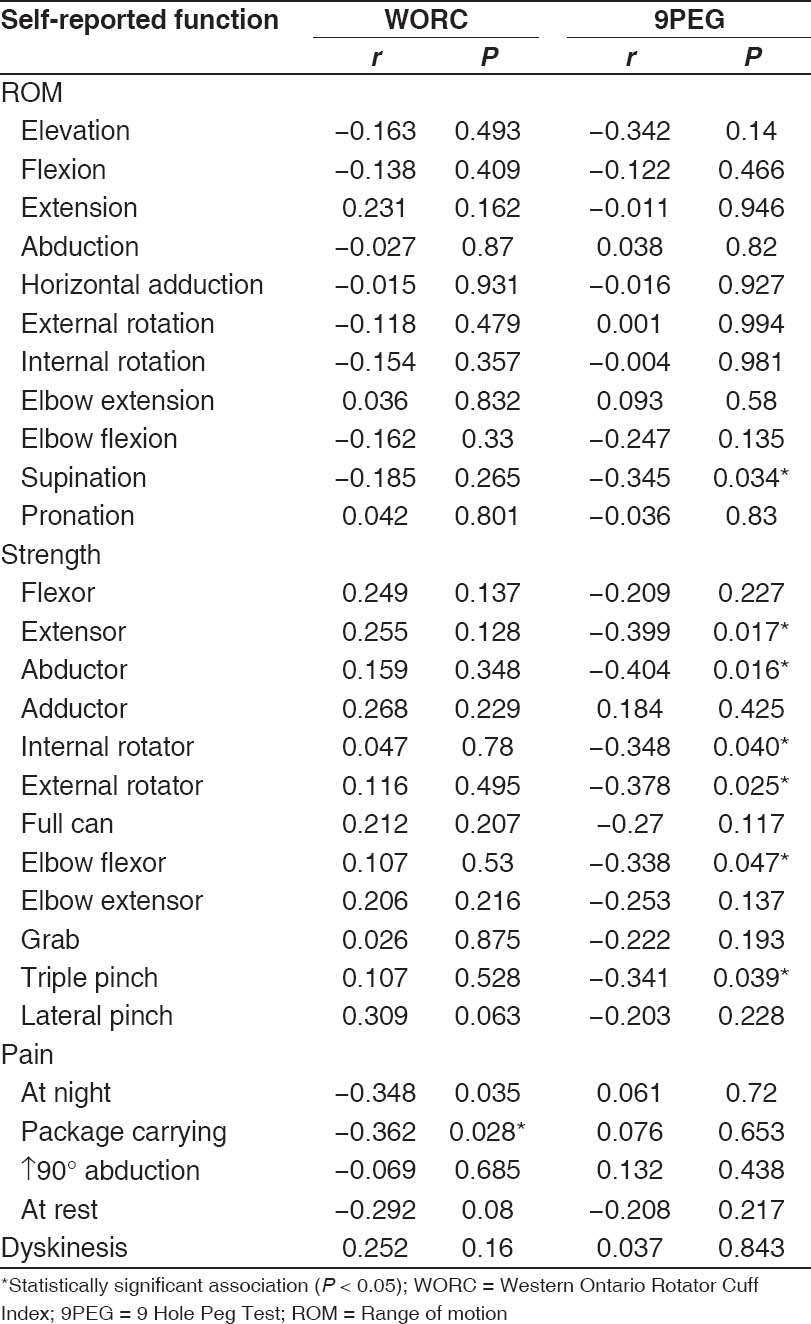 | Table 3: Correlations between self-reported function and pain, ROM, muscle strength
Click here to view |
A statistically significant, negative relationship was found between 9PEG and ROM in supination (r: −0.345, P: 0.034), as well as muscle strength of shoulder extensors (r: −0.399, P: 0.017), abductors (r: −0.404, P: 0.016), internal (r: −0.348, P: 0.04) and external rotators (r: −0.378, P: 0.025). There was also a statistically significant negative relationship between WORC scores and night pain/pain with package carrying (r: −0.362, P: 0.028). We found no significant relationship between WORC scores and ROM or muscle strength.
In addition, there was no statistical difference between WORC scores and 9PEG with regards to the presence of scapular dyskinesis, humeral head cysts, humeral head migration, tendon retraction, the number of tendons involved in RCT and the degree of atrophy (P > 0.05) [Table 4] and [Table 5].
 Discussion Discussion | |  |
In this study, we aimed to investigate whether two different validated tests (WORC, a self-reported outcome measure versus 9PEG, a functional test) used in the evaluation of patients with RCT may be used interchangeably to determine the upper extremity function. The relationship between the two tests and the parameters that may potentially influence the outcomes was also investigated. We found that, as outcome measures with distinct parameters, WORC and 9PEG yield different results with regards to the upper extremity function in patients with RCT.
We acknowledge that our study has some limitations that influenced the overall results. The relatively small sample size constituted by a majority of patients with small-sized RCT is the major drawback of this study. The use of a single outcome tool (WORC) for determining the upper extremity function is another limitation that precluded the comparison of a possible relationship between 9PEG and other outcome tools. Further studies with larger patient groups, which utilize multiple outcome tools and tests are warranted to conclude on the relationship and effectiveness of these tools in determining the upper extremity function.
It has been shown that validated, self-reported, condition-specific outcome measures are predictable and accurate in determining the extremity function and the response to treatment in musculoskeletal conditions, and are therefore recommended for utilization in patient populations with this group of disorders, [25] such as the use of WORC in patients with RCT and the use of Western Ontario Osteoarthritis of the Shoulder Index in patients with glenohumeral osteoarthritis. [26] On the other hand, it has been proposed that in addition to the objective measurements such as ROM and muscle strength, the utilization of performance-based tests prove more effective in determining subtle functional losses when compared with the subjective methods. [5] Thus, we used WORC to determine the upper extremity function in the setting of RCT, and used 9PEG to evaluate the functional performance in this study. [7],[21]
Question 1
One of the main findings of this study is the weak association between WORC scores and 9PEG, which was not statistically significant. This weak association and the difference between the parameters related to each method suggest that the use of one method as an alternative to the other one is not appropriate. In this study, considering α = 0.05 (two-sided) and β = 0.10 (power = 90%); the number of patients needed to meet assumption were 36. To the authors' knowledge, there exists no study in the literature investigating the accordance of a self-reported outcome measure with 9PEG for determining the upper extremity function in patients with RCT. Nevertheless, a weak relationship has been shown between objective measurements such as ROM and muscle strength, and subjective scores of SPADI and UPenn Shoulder Scale in patients following rotator cuff repair. [5] Another study has shown that no association exists between FIT-HaNSA and WORC for determining the upper extremity function in healthy shoulders. [10]
Another notable finding of this study is the negative relationship found between 9PEG scores and ROM in supination. However no association was noted between 9PEG scores and shoulder ROM. It has been previously shown that active abduction is the main factor that determines WORC scores in patients with RCT. [27] In this regard, it is not surprising to find no relationship between 9PEG and shoulder ROM in our study population, because 9PEG is a performance-based test that is routinely performed under the shoulder level (90°< abduction). Most of the activities related to the shoulder joint are performed in the scapular plane, rather than the frontal plane. We think that the shoulder joint is placed in a favorable position in the scapular plane during 9PEG, which provides an advantage in performing the test and may interfere with the performance-based results of the test. In addition, the fact that 9PEG is performed under the shoulder level creates a disadvantage in determining the functional loss secondary to the pain elicited by overhead activity (90°< abduction).
Question 2
We found that 9PEG test performance displayed a positive trend parallel to the increases in shoulder extensor, internal and external rotators and abductors, as well as elbow flexors and triple grab strength, while there was no significant relationship between WORC scores and the upper extremity ROM measurements, as well as the muscle strength. It has been shown that the elevation and abduction strength are the factors that determine WORC scores in patients with RCT. [27] On the contrary, it has been reported that internal and external rotation strength do not have a direct relationship with the upper extremity functional performance (FIT-HaNSA) or WORC scores in healthy shoulders. [10],[28] These results suggest that WORC and 9PEG are distinct outcome measures with different methodology in determining the upper extremity function, and the effectiveness of WORC in determining the upper extremity functional losses may be limited in comparison with 9PEG, particularly in the setting of strength loss. Further studies with larger groups are warranted to conclude on this matter.
We noted that WORC scores decreased as the night pain and pain with package carrying increased; however, we found no relationship between WORC scores and pain at rest, as well as pain with activities over 90° of elevation. With regards to the pain, not being able to sleep due to night pain and functional loss in daily life secondary to pain were the most pronounced complaints of our patient group. From this aspect, the results of our study are in accordance with patients' complaints. Recent findings suggest that there is no relationship between WORC scores and pain at rest, [27] which is parallel to our findings. The fact that there was no relationship between WORC scores and pain at rest, as opposed to night pain and pain with package carrying, may be attributed to patients' decreased quality of life caused by sleeplessness and intense night pain overshadowing their relatively less severe pain at rest. The education level of patients may have also influenced the results since it has been shown that WORC scores are affected by educational level. Seventeen of our patients were primary school graduates (44%) and 3 were illiterate patients (7.9%). A recent study pointed out that university graduates have 17.4 more points of WORC score in average as compared to the primary school graduates and illiterate individuals. [27] Previous studies comparing the psychometric features of these measures have reported on high standard errors, [5] thus we believe our patients may have had difficulties in making decisions, while scoring their pain.
Scapular dyskinesis may result either from a structural biomechanical disorder or pain caused by the tear. [24] The presence of RCT affects the glenohumeral force vectors, and this may cause dynamic instability in upper extremity during shoulder elevation and depression. The presence of scapular dyskinesis has been reported to decrease WORC scores by 6.85 points. [27] In contrast, the presence of scapular dyskinesis had no significant effect on WORC or 9PEG scores in our study. Similarly, neither the presence of humeral head cysts, migration and tear retraction nor the degree of fatty atrophy had any negative influence on the outcomes of WORC or 9PEG. In spite of surgical intervention, fatty degeneration and muscle atrophy are irreversible in the setting of chronic RCT. [28],[29] The presence of fatty degeneration causes recurrent tears and deterioration of clinical symptoms. [30],[31] The atrophy of the supraspinatus and infraspinatus muscles has been reported to decrease the WORC scores by 4.21 and 7.37, respectively. [27] It has been shown that the tear size is not a factor that determines the upper extremity function (WORC) in symptomatic, atraumatic RCT. [27] However, following the surgical repair, the tear size has been shown to influence the function in previous studies with self-reported questionnaires and clinical evaluations. [25],[32],[33],[34] Particularly, after repair of large and massive sized tears, functional outcomes such as muscle strength and objective active ROM measurements have been found to be inferior in short, [33] mid [32],[34] and long-term follow-ups. [18] The relationship between the tear size and functional outcomes has been varying following arthroscopic repair. Some authors propose that the functional outcome is not influenced by the tear size or muscle atrophy, while the others advocate that the integrity of rotator cuff is directly related to the functional outcome. [24],[35],[36] More studies that objectively evaluate the upper extremity function are required to address this controversy.
We acknowledge that our study has some limitations that influenced the overall results. The relatively small sample size constituted by a majority of patients with small-sized RCT is the major drawback of this study. The use of a single outcome tool (WORC) for determining the upper extremity function is another limitation that precluded the comparison of a possible relationship between 9PEG and other outcome tools. On the other hand, interpreting of the questions in survey (WORC) of patients with basic schooling may differ in patients with university graduates. In this regard difference in education, levels may affect the results and may constitute a limitation for the study. Further studies with larger patient groups which utilize multiple outcome tools and tests are warranted to conclude on the relationship and effectiveness of these tools in determining the upper extremity function.
 Conclusions Conclusions | |  |
The weak association between WORC and 9PEG, and the difference between the parameters related to each method suggest that they should not be used interchangeably to determine the upper extremity function. We recommend the utilization of 9PEG instead of WORC for upper extremity functional assessment in the setting of loss of muscle strength.
 References References | |  |
| 1. | Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am 2006;88:1699-704.  |
| 2. | Yamaguchi K, Sher JS, Andersen WK, Garretson R, Uribe JW, Hechtman K, et al. Glenohumeral motion in patients with rotator cuff tears: A comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg 2000;9:6-11.  |
| 3. | Bot SD, Terwee CB, van der Windt DA, Bouter LM, Dekker J, de Vet HC. Clinimetric evaluation of shoulder disability questionnaires: A systematic review of the literature. Ann Rheum Dis 2004;63:335-41.  |
| 4. | Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: A systematic review of four questionnaires. Arthritis Rheum 2009;61:623-32.  |
| 5. | Roddey TS, Cook KF, O′Malley KJ, Gartsman GM. The relationship among strength and mobility measures and self-report outcome scores in persons after rotator cuff repair surgery: Impairment measures are not enough. J Shoulder Elbow Surg 2005;14:95S-8.  |
| 6. | Fayad F, Mace Y, Lefevre-Colau MM. Shoulder disability questionnaires: A systematic review. Ann Readapt Med Phys 2005;48:298-306.  |
| 7. | Earhart GM, Cavanaugh JT, Ellis T, Ford MP, Foreman KB, Dibble L. The 9-hole PEG test of upper extremity function: Average values, test-retest reliability, and factors contributing to performance in people with Parkinson disease. J Neurol Phys Ther 2011;35:157-63.  |
| 8. | Tiffin J, Asher EJ. The Purdue pegboard; norms and studies of reliability and validity. J Appl Psychol 1948;32:234-47.  [ PUBMED] |
| 9. | Kumta P, MacDermid JC, Mehta SP, Stratford PW. The FIT-HaNSA demonstrates reliability and convergent validity of functional performance in patients with shoulder disorders. J Orthop Sports Phys Ther 2012;42:455-64.  |
| 10. | Roy JS, Macdermid JC, Boyd KU, Faber KJ, Drosdowech D, Athwal GS. Rotational strength, range of motion, and function in people with unaffected shoulders from various stages of life. Sports Med Arthrosc Rehabil Ther Technol 2009;1:4.  |
| 11. | Holtby R, Razmjou H. Measurement properties of the Western Ontario rotator cuff outcome measure: A preliminary report. J Shoulder Elbow Surg 2005;14:506-10.  |
| 12. | Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality of life measurement tool for rotator cuff disease: The Western Ontario Rotator Cuff Index (WORC). Clin J Sport Med 2003;13:84-92.  |
| 13. | Kellor M, Frost J, Silberberg N, Iversen I, Cummings R. Hand strength and dexterity. Am J Occup Ther 1971;25:77-83.  |
| 14. | Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the Box and Block Test of manual dexterity. Am J Occup Ther 1985;39:386-91.  |
| 15. | Oxford Grice K, Vogel KA, Le V, Mitchell A, Muniz S, Vollmer MA. Adult norms for a commercially available Nine Hole Peg Test for finger dexterity. Am J Occup Ther 2003;57:570-3.  |
| 16. | Beebe JA, Lang CE. Relationships and responsiveness of six upper extremity function tests during the first six months of recovery after stroke. J Neurol Phys Ther 2009;33:96-103.  |
| 17. | Hoffmann T, Russell T, Thompson L, Vincent A, Nelson M. Using the Internet to assess activities of daily living and hand function in people with Parkinson′s disease. NeuroRehabilitation 2008;23:253-61.  |
| 18. | Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am 2001; 83-A:71-7.  |
| 19. | Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal? J Bone Joint Surg Am 2005;87:1229-40.  |
| 20. | Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am 1986;68:1136-44.  [ PUBMED] |
| 21. | Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;304: 78-83.  |
| 22. | El O, Bircan C, Gulbahar S, Demiral Y, Sahin E, Baydar M, et al. The reliability and validity of the Turkish version of the Western Ontario Rotator Cuff Index. Rheumatol Int 2006; 26:1101-8.  |
| 23. | Itoi E, Kido T, Sano A, Urayama M, Sato K. Which is more useful, the "full can test" or the "empty can test," in detecting the torn supraspinatus tendon? Am J Sports Med 1999;27:65-8.  |
| 24. | Kibler WB, Sciascia A. Current concepts: Scapular dyskinesis. Br J Sports Med 2010;44:300-5.  |
| 25. | Gartsman GM, Brinker MR, Khan M. Early effectiveness of arthroscopic repair for full-thickness tears of the rotator cuff: An outcome analysis. J Bone Joint Surg Am 1998;80:33-40.  |
| 26. | Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg 2007;16:717-21.  |
| 27. | Harris JD, Pedroza A, Jones GL, MOON (Multicenter Orthopedic Outcomes Network) Shoulder Group. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: A time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med 2012;40:359-66.  |
| 28. | Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2000;82:505-15.  |
| 29. | Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 2007;35:719-28.  |
| 30. | Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg 2003;12:550-4.  |
| 31. | Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res 1997;344:275-83.  |
| 32. | Harryman DT 2 nd , Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA 3 rd . Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 1991;73:982-9.  |
| 33. | Iannotti JP, Bernot MP, Kuhlman JR, Kelley MJ, Williams GR. Postoperative assessment of shoulder function: A prospective study of full-thickness rotator cuff tears. J Shoulder Elbow Surg 1996;5:449-57.  |
| 34. | Romeo AA, Hang DW, Bach BR Jr, Shott S. Repair of full thickness rotator cuff tears. Gender, age, and other factors affecting outcome. Clin Orthop Relat Res 1999;367:243-55.  |
| 35. | Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 2004;86-A:219-24.  |
| 36. | Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 2007;89:953-60.  |
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
|
