| |


 |
| Year : 2014 | Volume
: 8
| Issue : 4 | Page : 114-121 |
|
|
|
|
|
REVIEW ARTICLE Intra-articular infiltration therapy for patients with glenohumeral osteoarthritis: A systematic review of the literature
Sascha Colen1, Pieter Geervliet2, Daniël Haverkamp3, Michel P. J. Van Den Bekerom4
1 Department of Orthopaedic Surgery, University Hospitals Leuven, Pellenberg, Belgium; Department of Orthopaedic Surgery and Traumatology, Hümmling Hospital Sögel, Sögel, Germany,
2 Department of Orthopaedic Surgery, Gemini Hospital, Den Helder, Amsterdam, the Netherlands,
3 Department of Orthopaedic Surgery, Slotervaart Hospital, Amsterdam, the Netherlands,
4 Department of Orthopaedic Surgery, Onze Lieve Vrouwe Gasthuis, Amsterdam, the Netherlands,
Correspondence Address:
Sascha Colen
Department of Orthopaedic Surgery and Traumatology, Hümmling Hospital Sögel, Mühlenstrasse 17, 49751 Sögel, Germany
 Source of Support: None, Conflict of Interest: None  | 5 |
DOI: 10.4103/0973-6042.145252

|
|
|
|
| Date of Web Publication | 21-Nov-2014 |
 Abstract Abstract | | |
Background: Conservative treatments are especially in patients with glenohumeral osteoarthritis (GH-OA) important, since shoulder arthroplasty has its limitations. In this systematic review, we will evaluate the current evidence regarding the efficacy of intra-articular (IA) infiltration treatment options in patients with GH-OA.
Materials and Methods: The following databases are searched: Pubmed/Medline, Cochrane Clinical Trial Register, Embase and the WHO clinical trial register. All IA injection products used for the treatment of shoulder OA in humans are included.
Results: A total of 8 studies could be included in this review. Hyaluronic acid (HA) showed effect sizes of 2.07, 2.02 and 2.11 at 6, 12 and 26 weeks follow-up, respectively. Placebo (1.60, 1.82 and 1.68) also showed stable effect sizes at the same time points. The efficacy of corticosteroids (CS) decreased rapidly at follow-up (1.08, 0.43 and 0.19). Although statistical significant, the maximum difference in effect sizes between HA and placebo was only 0.43 with absolute values between 2.0 and 6.4 on a 100-point visual analogue score for pain.
Conclusion: IA treatment with HA has a good efficacy at follow-up compared to baseline. However, the difference in efficacy between HA and placebo never reaches the minimal clinically important difference at any of the follow-up points. We are not able to give clear recommendations for the use of IA CS injections in patients with GH-OA. In future research, we recommend focusing on sufficiently powered randomized trials to compare the efficacies of HA, CS, placebo and other IA treatment options in patients with GH-OA.
Keywords: Anesthetics, corticosteroid, hyaluronic acid, hyaluronan, osteoarthritis, shoulder, sodium hyaluronate, systematic review, viscosupplementation
How to cite this article:
Colen S, Geervliet P, Haverkamp D, Van Den Bekerom MP. Intra-articular infiltration therapy for patients with glenohumeral osteoarthritis: A systematic review of the literature. Int J Shoulder Surg 2014;8:114-21 |
 Introduction Introduction | |  |
Glenohumeral osteoarthritis (GH-OA) is characterized by a gradual, progressive, mechanical, and biochemical breakdown of the articular cartilage and other joint tissues, including bone and joint capsule. As the articular surface wears, friction within the joint increases and causes progressive loss of the normal load-bearing surfaces with pain, stiffness and disability as a result. Patients can have pain at night, especially when the patient lies on the affected shoulder. [1],[2],[3],[4],[5] The cause of GH-OA can be divided into a primary or secondary type, resulting from trauma (fracture or instability), inflammatory arthropathies, or genetic predisposition. [6] Painful GH-OA is difficult to treat and highly disabling. [1],[2],[4] Shoulder arthroplasty is effective at reducing pain and improving range of motion, [1],[7] but complications such as periprosthetic fractures, infections and instability of the joint are not unusual. [8] In clinical practice, the most effective nonsurgical treatments of shoulder OA are a combination of therapies, customized to patient's requirements, rather than a single drug or a single nonsurgical intervention. [1],[9] Several nonsurgical treatment options for GH-OA are widely known. Changes in daily activities and occupation should be considered. Physical therapy can be advised to keep range motion and muscle strength. However, an incongruent shoulder joint can lead to an increase of pain. [10] Pharmacological treatments, including acetaminophen (first pharmacological option), nonsteroidal anti-inflammatory drugs (NSAIDs), narcotic and nonnarcotic analgesics and intra-articular (IA) injections of corticosteroids (CS) or hyaluronic acid (HA), have been the mainstay of nonsurgical treatment. [11],[12],[13] Analgesics and NSAIDs can be insufficient and can be associated with (well-known) adverse effects, especially in the elderly patient. [14],[15],[16],[17] The use of IA CS and HA in patients with OA is well documented. Especially concerning knee OA, a large number of studies is published about the efficacy of different IA administered treatments. Several reviews conclude that HA has a positive effect on pain. [18],[19] However, in the systematic review and meta-analysis of Colen et al., a large placebo effect was shown in the knee and hip. [18],[20] The difference between the efficacies of IA administered HA and placebo was considered significant, but not reaching the minimum clinically important difference (MCID). Bannuru et al. showed in a meta-analysis that HA is superior to CS after 8 weeks. [21] However, CS is more effective up to 4 weeks after IA administration. We are not aware of a published review concerning the efficacy of the different IA infiltration treatment options for GH-OA. In this systematic review, we will describe and evaluate the current evidence regarding efficacy of the several IA infiltration treatment options of patients with GH-OA with or without a rotator cuff tears.
 Materials and methods Materials and methods | |  |
Inclusion criteria
Types of studies
A search of the literature performed for this review was limited to published original reports concerning the IA injection treatment of adults with GH-OA. Studies form levels I to IV were included [Table 1]. Abstracts from scientific meetings, unpublished reports, case reports, expert opinions and review articles were not included.
Types of participants
Inclusion was limited to articles on male and female adult humans with primary and secondary GH-OA. The diagnosis of GH-OA was made by history, physical examination and radiology. Patients with bilateral GH-OA were also included.
Studies focussing on "OA of the acromion-clavicular joint," "shoulder impingement," "rotator cuff tendinopathy," "adhesive capsulitis" and "periarthritis" were not included in the current review. A mixed population of OA and other pathologies was included if the OA population could be analyzed separately.
Types of intervention
All IA injection products (corticoids, HA, platelet rich plasma, stem cells, and anti-inflammatory drugs) used for the treatment of shoulder OA in humans were included. Studies comparing one of the IA injections with another active or placebo treatment were also included. All approaches (posterior and anterior) and techniques (ultrasound or fluoroscopic guided or no guidance) of IA administration were included.
Types of outcomes measures
The Outcome Measures in Rheumatology (OMERACT) III core set of outcome measures was considered for analysis; pain, physical function and patient global assessment. [22] The minimum criterion for inclusion of the trial in the review was the adequate reporting of at least one of the outcome variables. Information regarding other outcome measures and adverse events was extracted and analyzed when feasible.
Search strategy for identification of studies
The following databases were searched: Pubmed/Medline (period 1966 to June 1st 2013), Cochrane Clinical Trial Register (1988 to June 1st 2013), Embase (January 1988 to June 1st 2013) and the WHO clinical trial register to identify all articles concerning the IA injection therapy for GH-OA. The search was independently performed by two authors (SC and PG). When using the search terms (Viscosupplementation OR HA OR CS OR platelet rich plasma OR stem cells OR anti-inflammatory drugs AND shoulder) we initially found 1492 papers. Osteoarthritis was not used as a search term, because of the risk of missing studies. The references of retrieved publications were also manually checked to add studies potentially meeting the inclusion criteria and missed by the electronic search. Papers not written in English language were considered if translation was possible. The flowchart is defined in [Figure 1].
Methods of the review
Selection of trials
Trial selection was done by two authors (SC and PG) reviewing title and abstract to identify potentially relevant articles for our review. The full manuscript was retrieved when the title, keywords or abstract revealed insufficient information to determine the appropriateness for inclusion. Disagreement was resolved by discussion, with arbitration when necessary by a third reviewer (MB) when differences remained.
Data collection
From the included studies, data for meta-analysis was extracted by one reviewer (PG), using a prepiloted data extraction-tool. Extraction was verified by a second reviewer (SC). Disagreements were resolved in a consensus meeting or, if necessary, by third party adjudication (DH). Articles were not blinded for author, affiliation, and source. [23],[24],[25] If necessary, authors were contacted for additional information.
Assessment of methodological quality
Differences in quality amongst trials indicate a possible difference in bias between these trials. Therefore, it is important to evaluate the quality of the trials when evaluating the effectiveness of an intervention. Two independent reviewers (SC and PG) obtained the full text of all potentially eligible articles for independent methodological assessment. Studies were scored according to the Level of evidence and recommendations for clinical practice were formulated [Table 1] and [Table 2]. The strength of these recommendations was classified with a grade [Table 3].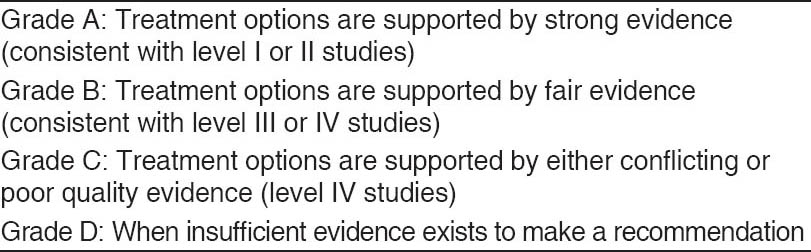 | Table 3: Grades of recommendation (given to various treatment options based on the level of evidence supporting that treatment)
Click here to view |
Quantitative analysis
Since many studies used different subjective outcome scoring systems, the average improvement is calculated as an effect size, this is a well-established measurement in which the improvement of the score is divided by the standard deviation of the pretreatment score. The average effect sizes pertreatment will be compared using Student's t-test. P < 0.05 was considered to be significant.
 Results Results | |  |
The initial search using the above-mentioned search strategy resulted in 1492 studies, after reading the title and abstract, 32 articles were screened for eligibility. We included two randomized controlled trials (RCTs) comparing the efficacy of IA administered HA with placebo, five prospective case series (all using IA administered HA), and one retrospective study comparing the efficacy of HA and CS. [1],[10],[13],[14],[26],[27],[28],[29] A total of 895 patients was included in these 8 studies; 579 patients received HA (Hylan G-F 20 (Synvisc® , Genzyme Corporation, Cambridge, MA, USA), Supartz® (Smith & Nephew, Inc, Andover, MA, USA) or Hyalgan® (Sanofi-Aventis, Bridgewater, NJ, USA and Fidia Farmaceutici, SpA, Abano Terme, Italy), 33 patients CS (6-methylprednisolone acetate, Depo-Medrol® , Pfizer, Latina, Italy) and 283 patients phosphate-buffered saline (PBS) [Table 2]. The first article was published in 1988 and the most recent in January 2013.
Randomized clinical trials
The first performed RCT (Blaine et al.) studied 660 patients with persistent shoulder pain. [14] Patients were treated with a weekly series of 3 injections of Hyalgan® and 2 injections with PBS (three-injection group), 5 injections of Hyalgan® (five-injection group), or 5 injections of PBS (control group). A subgroup of the study population had radiographic signs of GH-OA. Of the patients with GH-OA 136 patients were included in the three-injection group, 129 in the five-injection group, and 133 in the control group. The visual analog score (VAS: 100 point scale) for pain showed a difference of 7.5 (standard deviations [SD]: 2.5) comparing the efficacy of the treatment in the three-injection group with the control group (in favour of the three-injection group: P = 0.003). Similar results were shown between the five-injection group and the control group with a difference of 7.8 (SD: 2.5) (P = 0.002). At all follow-up visits (7, 9, 17, and 26 weeks) there was a significant improvement using the VAS for pain compared to baseline in both three- and five-injection groups (P < 0.05). No difference in efficacy was noted between the three- and five-injection groups during the 26 weeks follow-up period. The second RCT also studied the efficacy of IA administered HA (Supartz® ) and compared this with IA administered PBS. [10] Three weekly injections of either HA or PBS was given in patients with chronic shoulder pain associated with GH-OA. The injections were performed without the support of ultrasound or fluoroscopy. A total of 300 patients were included (150 patients with HA and 150 with PBS). The improvement in VAS for pain between baseline and 26 weeks follow-up was 19.88 for the HA treated patients and 16.3 for the PBS treated patients. The least-squares difference in VAS between the groups (at 7, 13, 20 and 26 weeks follow-up) was 2.8 in favour of the HA treated patients (P = 0.112). For the patients only with GH-OA and no other shoulder pathologies the improvement in VAS between baseline and 26 weeks follow-up was 21.0 for the HA treated patients and 15.7 in the PBS treated patients. The repeated-measures longitudinal analysis showed a significant difference between these groups (P = 0.038). Similar results were observed using the OMERACT-Osteoarthritis Research Society International (OARSI) high responder rates (a score evaluating treatment effects in OA). The HA treated patients showed a higher OMERACT-OARSI high responder rate, with an odds ratio of 1.45 (95%CI: −0.97 to 2.17) and 6.92% difference in responder rate at 26 weeks follow-up. In the patients only with GH-OA the OMERACT-OARSI high responder rates were similar (1.62 [95%CI: −1.06 to 2.50] and an 8.37% difference in responder rate) at 26 weeks. This odds ratio also showed a significant difference between the HA and PBS treated patients (in favour of the HA treated patients: P = 0.028).
Prospective case series
Leardini et al. were in 1988 the first to report the outcome of IA administered HA in 29 patients with a painful shoulder including six patients diagnosed with OA. [26] Each patient received 3 injections with a 3 days interval. The total follow-up was only 11 days and of the patients with shoulder OA 3 had a fairly good result, while the other 3 experienced good to very good results.
Noël et al. were the first to study clearly defined and uniform population (33 patients) who had primary GH-OA and an intact rotator cuff. [28] All patients were treated with Hylan G-F 20. A second infiltration with HA was possible on demand of the patient at 1, 2 or 3 months follow-up. The VAS for pain decreased from 61.2 at baseline to 37.1 at 3 months follow-up (P < 0.001). The Western Ontario Osteoarthritis of the Shoulder score (a disease-specific quality of life score) (45.7% at baseline to 63.1% at 3 months follow-up) and SF-36 score (38.6 at baseline to 40.7 at 3 months follow-up) also showed improvement. However, only the results of the Western Ontario osteoarthritis of the shoulder score were significant (P < 0.001).
In a letter to the editor Valiveti et al. reported the results of 11 courses of IA administered HA (Hylan G-F 20: Weekly for 3 weeks and Hyalgan: Weekly for 5 weeks). [29] Five patients had moderate improvement; five had mild improvement, and one had no improvement. The average time of improvement was 4 months (range: 2-12 months).
Brander et al. in their prospective case series included 36 patients with GH-OA that were intra-articularly infiltrated with a series of 2 injections of Hylan G-F 20 14 days apart. [1] The VAS for pain improved from 63.0 (SD: 14.5) at baseline to 38.9 (SD: 27.6), 41.4 (SD: 23.9), and 34.9 (SD: 21.7) at 6, 12 and 26 weeks follow-up, respectively (P < 0.001 at all follow-up visits). The Western Ontario Rotator Cuff Index (a quality of life index using the VAS including 5 domains: Physical symptoms, sports and recreation, work social function, and emotions) showed similar results with a score of 65.3 (SD: 18.4) at baseline improving to 48.4 (SD: Not available), 49.9 (SD: Not available) and 45.9 (SD: 22.4) at 6, 12 and 26 weeks follow-up respectively (P < 0.001 at all follow-up visits). Silverstein et al. in their prospective study reported the results of 27 patients with GH-OA who were IA injected with Hylan G-F 20. [13] The infiltrations were blind performed. The VAS for pain improved from 54.0 at baseline to 42 (P = 0.01), 36 (P < 0.001), and 30 (P < 0.001) at 1, 3, and 6 months follow-up, respectively. The modified University of California at Los Angeles score (a score consisting of the sum of the individual scores for pain, function, motion, and strength) improved significant at all 3 follow-up visits (15.7 at baseline to 20.0, 20.8, and 20.5, respectively). The simple shoulder test (a patient completed form that measures a patient's ability to perform 12 common tasks in normal activities of daily living and work) improved from 5.7 at baseline to 7.2 (P = 0.012), 7.2 (P = 0.001), and 7.6 (P = 0.001) at 1, 3, and 6 months, respectively.
Retrospective case-control study
Merolla et al. reported a retrospective case-control study comparing IA CS and HA in patients with GH-OA. [27] Fifty-one patients received HA and 33 CS. The VAS for pain in the HA injected group decreased from 61.0 (SD: 9.1) to 33.7 (SD: 9.4), 35.1 (SD: 8.9) and 36.5 (SD: 9.0) at 1, 3 and 6 months follow-up, respectively (P < 0.05 at all follow-up visits). The effect of IA administered CS was less. At baseline, the VAS for pain was 62.5 (SD: 16.7) which decreased to 44.2 (SD: 11.7; P = 0.0431), 55.4 (SD: 18.4; P = 0.0626), and 59.4 (SD: 15.8; P = 0.0691) at 1, 3 and 6 months follow-up, respectively. The shoulder pain and disability index and the Constant-Murley scale as clinical outcome parameters improved significant showing improvement at 1, 3 and 6 months follow-up for the HA injected group and only at 1 month follow-up in the CS injected group.
Statistical analysis of available data
For 5 studies (6 groups) data could be extracted, and effect sizes could be calculated at 6 weeks, 12 weeks and 26 weeks for HA. [1],[10],[14],[27],[28] Pooling these data resulted in stable effect sizes at each of these time points, respectively 2.07 (±0.53), 2.02 (±0.53) and 2.11 (±0.40) [Figure 2].
From the studies of Blaine et al. [14] and Kwon et al. [10] an effect size for placebo could be calculated. As for HA these effect sizes are stable during follow-up at 6, 12 and 26 weeks (1.60 (±0.04), 1.82 (±0.04) and 1.68 (±0.23), respectively) [Figure 3].
Only the study of Merolla et al. [27] allowed calculation of effect size for CS [Figure 4]. The effect size between placebo and HA are significantly different at 6, 12 and 26 weeks follow-up (all P < 0.01). Although statistically significant, the maximum difference in effect size at any of the time points is only 0.4 and the pooled differences between HA and placebo ranches between 2.0 and 6.4 on a 100-point VAS for pain.
Safety data
None of the included studies reported severe adverse effects. [1],[10],[13],[14],[26],[27],[28],[29] Five studies reported mild local adverse effects, such as local pain and local reaction at the injection side. [1],[10],[14],[27],[28] Local adverse effects occurred in the patients treated with IA administered HA, CS and placebo (PBS) [Table 2].
 Discussion Discussion | |  |
The objective of this systematic review was to collect the available evidence reported on the outcome of IA injection treatments for patients with GH-OA. The efficacy of IA administered HA was described in 8 studies, of IA administered CS in 1 study and IA administered PBS (placebo) in 2 studies. We found no studies reporting the efficacy of IA injection treatment with platelet rich plasma, stem cells or other more experimental therapies for patients with GH-OA. The level of evidence of most of the included studies was low [Table 2]. The retrospective case-control series (Merolla et al.) was the only study reporting on the efficacy of IA administered CS. [27] Other concerns regarding the quality of the reported studies in this review include the not well-defined characteristics of the baseline characteristics, and the blindly and not ultrasound guided performed infiltrations in most studies. Blind infiltrations, especially performed in the study setting, can affect the outcome of the treatment since only 28-100% of the injections seem to be performed intra-articularly. [30],[31],[32],[33]
We were able to show that the improvement in pain and function using IA HA as treatment for patients with GH-OA compared to baseline at all the follow-up points (6, 12 and 26 weeks) was significant, showing effect sizes of more than 2 [Figure 2]. However, the effect sizes of IA administered PBS were also at least 1.5 at the same follow-up points. The efficacy of IA administered HA compared with PBS showed an efficacy in favour of HA (P < 0.01), but the maximum absolute difference in efficacy using the VAS for pain was 6.4 on 100 points. This difference is not reaching the MCID and the question should be asked whether IA treatment with HA is in clinical practice superior to IA administered PBS. [34] The efficacy of IA administered CS (although the level of evidence is very poor) is even less. At 6 weeks follow-up the effect size was 1.08 compared with baseline, but at 12 and 26 weeks the effect sizes were even lower, 0.43 and 0.19, respectively. Although the concerns about the design of the study of Merolla et al., the data reported in this review indicate that IA administered HA has a longer and better efficacy in patients with GH-OA than CS. [27] Bannuru et al. showed similar data in their systematic review about the efficacy of IA administered HA and CS in the knee. [21]
Several systematic reviews and meta-analysis regarding the efficacy of IA treatment with HA in patients with knee OA report similar results as we are showing in the shoulder, with small to moderate treatment effects compared with PBS. [18],[19] Rutjes et al. concluded that the treatment with IA administered HA in patients with knee OA showed only small and clinically irrelevant benefit compared to IA administered saline and a risk for serious adverse events. [19] Colen et al. showed a 40-50% pain reduction in patients treated with IA HA at a follow-up of 3 months. [18] When comparing the efficacy of IA administered HA to saline (approximately 30% pain reduction) they determined a weighted mean difference of just 10.20 using the VAS for pain. Colen et al. also studied the efficacy of IA administered HA in other joints (the metatarsophalangeal-joint, the ankle, the hip, the sacroiliac joint, the facet joints, the carpometacarpal-1 joint and the shoulder). [20] They concluded that there is a significant improvement in pain injecting IA HA compared to baseline, but comparing the efficacy of HA to placebo there is only limited evidence that HA is superior and that there is no evidence that IA HA is better than CS or other conservative therapies.
Both HA and CS injections are well-tolerated. Local adverse effects in the shoulder are typical of those observed in the hip and knee joint [Table 2]. [1],[10],[13],[14],[26],[27],[28],[29],[35],[36] Serious adverse effects are not reported in the studies included in this review. CS infiltrations are frequently administered for the treatment of shoulder pain and have been effective in clinical trials. [37],[38],[39],[40] However, the indications in all these studies for the treatment with CS were rotator cuff tendinopathy and adhesive capsulitis. In addition, the potential damage to the collagen matrix of tendons and ligaments suggests caution in the use of CS injections around the shoulder, especially with repeated infiltrations. [41],[42],[43],[44] Several clinical studies have indicated that HA is also effective in managing pain associated with various other shoulder pathologies (adhesive capsulitis and rotator cuff tendinopathy). [45],[46],[47],[48],[49]
Although the difference in efficacy between IA administered HA and PBS is small, the efficacy of IA injection of HA at follow-up during the first 6 months is good in patients with GH-OA [grade A of recommendations: [Table 3]]. IA treatment with HA is useful as a conservative treatment in patients with GH-OA. Because the IA treatment with CS is only reported in a single retrospective case control study showing a very low efficacy [grade B of recommendations: [Table 3]] and the fact that the above-mentioned risks of the use of IA CS are serious, we agree with the guidelines of the American Academy of Orthopedic Surgeons that there are no clear recommendations for the use of IA CS injections in patients with GH-OA. [50] In future research we recommend to focus on sufficiently powered randomized trials to compare the efficacy of HA, CS, PBS and other IA treatment options in patients with GH-OA.
 Acknowledgments Acknowledgments | |  |
The authors have no conflicts of interest that are directly relevant to this systematic review. There is no support from any organization for the submitted work, no financial relationship with any organizations that might have an interest in the submitted work in the previous 2 years and no other relationship or activity that could appear to have influenced the submitted work.
 References References | |  |
| 1. | Brander VA, Gomberawalla A, Chambers M, Bowen M, Nuber G. Efficacy and safety of hylan G-F 20 for symptomatic glenohumeral osteoarthritis: A prospective, pilot study. PM R 2010;2:259-67.  |
| 2. | Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: Part II. Treatment. Am Fam Physician 2008;77:493-7.  |
| 3. | Meislin RJ, Sperling JW, Stitik TP. Persistent shoulder pain: Epidemiology, pathophysiology, and diagnosis. Am J Orthop (Belle Mead NJ) 2005;34:5-9.  |
| 4. | Millett PJ, Gobezie R, Boykin RE. Shoulder osteoarthritis: Diagnosis and management. Am Fam Physician 2008;78:605-11.  |
| 5. | van der Meijden OA, Gaskill TR, Millett PJ. Glenohumeral joint preservation: A review of management options for young, active patients with osteoarthritis. Adv Orthop 2012;2012:160923.  |
| 6. | Kerr R, Resnick D, Pineda C, Haghighi P. Osteoarthritis of the glenohumeral joint: A radiologic-pathologic study. AJR Am J Roentgenol 1985;144:967-72.  [ PUBMED] |
| 7. | van de Sande MA, Brand R, Rozing PM. Indications, complications, and results of shoulder arthroplasty. Scand J Rheumatol 2006;35:426-34.  |
| 8. | Sperling JW, Hawkins RJ, Walch G, Zuckerman JD. Complications in total shoulder arthroplasty. J Bone Joint Surg Am 2013;95:563-9.  |
| 9. | Iannotti JP, Kwon YW. Management of persistent shoulder pain: A treatment algorithm. Am J Orthop (Belle Mead NJ) 2005;34:16-23.  |
| 10. | Kwon YW, Eisenberg G, Zuckerman JD. Sodium hyaluronate for the treatment of chronic shoulder pain associated with glenohumeral osteoarthritis: A multicenter, randomized, double-blind, placebo-controlled trial. J Shoulder Elbow Surg 2013;22:584-94.  |
| 11. | Recommendations for the medical management of osteoarthritis of the hip and knee:2000 update. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum 2000;43:1905-15.  |
| 12. | Hinton R, Moody RL, Davis AW, Thomas SF. Osteoarthritis: Diagnosis and therapeutic considerations. Am Fam Physician 2002;65:841-8.  |
| 13. | Silverstein E, Leger R, Shea KP. The use of intra-articular hylan G-F 20 in the treatment of symptomatic osteoarthritis of the shoulder: A preliminary study. Am J Sports Med 2007;35:979-85.  |
| 14. | Blaine T, Moskowitz R, Udell J, Skyhar M, Levin R, Friedlander J, et al. Treatment of persistent shoulder pain with sodium hyaluronate: A randomized, controlled trial. A multicenter study. J Bone Joint Surg Am 2008;90:970-9.  |
| 15. | Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR Recommendations 2003: An evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2003;62:1145-55.  |
| 16. | Singh G. Recent considerations in nonsteroidal anti-inflammatory drug gastropathy. Am J Med 1998;105:31S-8S.  [ PUBMED] |
| 17. | Singh G, Rosen Ramey D. NSAID induced gastrointestinal complications: The ARAMIS perspective - 1997. Arthritis, Rheumatism, and Aging Medical Information System. J Rheumatol Suppl 1998;51:8-16.  |
| 18. | Colen S, van den Bekerom MP, Mulier M, Haverkamp D. Hyaluronic acid in the treatment of knee osteoarthritis: A systematic review and meta-analysis with emphasis on the efficacy of different products. BioDrugs 2012;26:257-68.  |
| 19. | Rutjes AW, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S. Viscosupplementation for osteoarthritis of the knee: A systematic review and meta-analysis. Ann Intern Med 2012;157:180-91.  |
| 20. | Colen S, Haverkamp D, Mulier M, van den Bekerom MP. Hyaluronic acid for the treatment of osteoarthritis in all joints except the knee: What is the current evidence? BioDrugs 2012;26:101-12.  |
| 21. | Bannuru RR, Natov NS, Obadan IE, Price LL, Schmid CH, McAlindon TE. Therapeutic trajectory of hyaluronic acid versus corticosteroids in the treatment of knee osteoarthritis: A systematic review and meta-analysis. Arthritis Rheum 2009;61:1704-11.  |
| 22. | Bellamy N, Kirwan J, Boers M, Brooks P, Strand V, Tugwell P, et al. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis. Consensus development at OMERACT III. J Rheumatol 1997;24:799-802.  |
| 23. | Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials 1996;17:1-12.  |
| 24. | Schulz KF, Chalmers I, Grimes DA, Altman DG. Assessing the quality of randomization from reports of controlled trials published in obstetrics and gynecology journals. JAMA 1994;272:125-8.  [ PUBMED] |
| 25. | Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Knipschild PG. Balneotherapy and quality assessment: Interobserver reliability of the Maastricht criteria list and the need for blinded quality assessment. J Clin Epidemiol 1998;51:335-41.  |
| 26. | Leardini G, Perbellini A, Franceschini M, Mattara L. Intra-articular injections of hyaluronic acid in the treatment of painful shoulder. Clin Ther 1988;10:521-6.  |
| 27. | Merolla G, Sperling JW, Paladini P, Porcellini G. Efficacy of Hylan G-F 20 versus 6-methylprednisolone acetate in painful shoulder osteoarthritis: A retrospective controlled trial. Musculoskelet Surg 2011;95:215-24.  |
| 28. | Noël E, Hardy P, Hagena FW, Laprelle E, Goebel F, Faure C, et al. Efficacy and safety of Hylan G-F 20 in shoulder osteoarthritis with an intact rotator cuff. Open-label prospective multicenter study. Joint Bone Spine 2009;76:670-3.  |
| 29. | Valiveti M, Reginato AJ, Falasca GF. Viscosupplementation for degenerative joint disease of shoulder and ankle. J Clin Rheumatol 2006;12:162-3.  [ PUBMED] |
| 30. | Jo CH, Shin YH, Shin JS. Accuracy of intra-articular injection of the glenohumeral joint: A modified anterior approach. Arthroscopy 2011;27:1329-34.  |
| 31. | Kraeutler MJ, Cohen SB, Ciccotti MG, Dodson CC. Accuracy of intra-articular injections of the glenohumeral joint through an anterior approach: Arthroscopic correlation. J Shoulder Elbow Surg 2012;21:380-3.  |
| 32. | Sethi PM, Kingston S, Elattrache N. Accuracy of anterior intra-articular injection of the glenohumeral joint. Arthroscopy 2005;21:77-80.  |
| 33. | Tobola A, Cook C, Cassas KJ, Hawkins RJ, Wienke JR, Tolan S, et al. Accuracy of glenohumeral joint injections: Comparing approach and experience of provider. J Shoulder Elbow Surg 2011;20:1147-54.  |
| 34. | Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg 2009;18:927-32.  |
| 35. | Caborn D, Rush J, Lanzer W, Parenti D, Murray C, Synvisc 901 Study Group. A randomized, single-blind comparison of the efficacy and tolerability of hylan G-F 20 and triamcinolone hexacetonide in patients with osteoarthritis of the knee. J Rheumatol 2004;31:333-43.  |
| 36. | Wobig M, Dickhut A, Maier R, Vetter G. Viscosupplementation with hylan G-F 20: A 26-week controlled trial of efficacy and safety in the osteoarthritic knee. Clin Ther 1998;20:410-23.  |
| 37. | Arroll B, Goodyear-Smith F. Corticosteroid injections for painful shoulder: A meta-analysis. Br J Gen Pract 2005;55:224-8.  |
| 38. | Carette S, Moffet H, Tardif J, Bessette L, Morin F, Frémont P, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: A placebo-controlled trial. Arthritis Rheum 2003;48:829-38.  |
| 39. | Hay EM, Thomas E, Paterson SM, Dziedzic K, Croft PR. A pragmatic randomised controlled trial of local corticosteroid injection and physiotherapy for the treatment of new episodes of unilateral shoulder pain in primary care. Ann Rheum Dis 2003;62:394-9.  |
| 40. | van der Windt DA, Bouter LM. Physiotherapy or corticosteroid injection for shoulder pain? Ann Rheum Dis 2003;62:385-7.  [ PUBMED] |
| 41. | Mikolyzk DK, Wei AS, Tonino P, Marra G, Williams DA, Himes RD, et al. Effect of corticosteroids on the biomechanical strength of rat rotator cuff tendon. J Bone Joint Surg Am 2009;91:1172-80.  |
| 42. | Stannard JP, Bucknell AL. Rupture of the triceps tendon associated with steroid injections. Am J Sports Med 1993;21:482-5.  |
| 43. | Tillander B, Franzén LE, Karlsson MH, Norlin R. Effect of steroid injections on the rotator cuff: An experimental study in rats. J Shoulder Elbow Surg 1999;8:271-4.  |
| 44. | Wiggins ME, Fadale PD, Barrach H, Ehrlich MG, Walsh WR. Healing characteristics of a type I collagenous structure treated with corticosteroids. Am J Sports Med 1994;22:279-88.  |
| 45. | Chou WY, Ko JY, Wang FS, Huang CC, Wong T, Wang CJ, et al. Effect of sodium hyaluronate treatment on rotator cuff lesions without complete tears: A randomized, double-blind, placebo-controlled study. J Shoulder Elbow Surg 2010;19:557-63.  |
| 46. | Itokazu M, Matsunaga T. Clinical evaluation of high-molecular-weight sodium hyaluronate for the treatment of patients with periarthritis of the shoulder. Clin Ther 1995;17:946-55.  |
| 47. | Rovetta G, Monteforte P. Intraarticular injection of sodium hyaluronate plus steroid versus steroid in adhesive capsulitis of the shoulder. Int J Tissue React 1998;20:125-30.  |
| 48. | Shibata Y, Midorikawa K, Emoto G, Naito M. Clinical evaluation of sodium hyaluronate for the treatment of patients with rotator cuff tear. J Shoulder Elbow Surg 2001;10:209-16.  |
| 49. | Tamai K, Mashitori H, Ohno W, Hamada J, Sakai H, Saotome K. Synovial response to intraarticular injections of hyaluronate in frozen shoulder: A quantitative assessment with dynamic magnetic resonance imaging. J Orthop Sci 2004;9:230-4.  |
| 50. | Izquierdo R, Voloshin I, Edwards S, Freehill MQ, Stanwood W, Wiater JM, et al. American academy of orthopaedic surgeons clinical practice guideline on: The treatment of glenohumeral joint osteoarthritis. J Bone Joint Surg Am 2011;93:203-5.  [ PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1], [Table 2], [Table 3]
|
