|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 9
| Issue : 1 | Page : 34-38 |
|
Insecticidal net distribution channel that is rural women-friendly, in Abia South, Nigeria
UM Nwosu1, LN Chigbu2, RA Eke3, CO Emereole4
1 Department of Nursing Sciences, Abia State University, Uturu, Nigeria
2 Department of Medical Microbiology, Abia State University Teaching Hospital, Abia, Nigeria
3 Department of Public Health, Abia State University Teaching Hospital, Abia, Nigeria
4 Department of Health Science, Federal University of Technology Owerri, Imo State, Nigeria
| Date of Web Publication | 15-May-2014 |
Correspondence Address:
L N Chigbu
Department of Medical Microbiology, Abia State University Teaching Hospital, Abia
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/9783-1230.132557

Background: Government channel for distributing free insecticidal nets stop at the health centers. About 70% of rural women who do not access this health facility fail to collect the free nets. Alternative channel for reaching these women is hereby advocated. Materials and Methods: An interventional study was carried out in eight randomly selected villages of Abia South. Experimental and control groups were assigned four villages each. Sample size for each group was 200 households systematically selected. Questionnaire and interview guide were instruments for data collection. Data were analyzed quantitatively. Chi-square statistic was used in testing for statistical significance. Results: Before intervention, ownership and utilization of treated nets in experimental group were 36.5% and 28.8%, respectively, while in the control group, it was 38% and 30.0%, respectively. Ownership and utilization of treated nets in experimental group increased by 54.5% and 46.5%, respectively, after intervention. In the control group, where there were no interventional activities carried out, ownership and utilization of treated nets showed no significant increase. Conclusion: Health promotion intervention, fixed-install mental payment-basis for net cost, and home-based net distribution channel scaled up net ownership and utilization by 54.5% and 46.5%, respectively, in the study area. Keywords: Abia South, Net distribution channel, Nigeria, Rural women-friendly
How to cite this article:
Nwosu U M, Chigbu L N, Eke R A, Emereole C O. Insecticidal net distribution channel that is rural women-friendly, in Abia South, Nigeria. J Med Investig Pract 2014;9:34-8 |
How to cite this URL:
Nwosu U M, Chigbu L N, Eke R A, Emereole C O. Insecticidal net distribution channel that is rural women-friendly, in Abia South, Nigeria. J Med Investig Pract [serial online] 2014 [cited 2018 Aug 24];9:34-8. Available from: http://www.jomip.org/text.asp?2014/9/1/34/132557 |
| Introduction | |  |
In rural communities of Abia South, various methods and combination of methods are used as protective measures against mosquito bite within a household. These include aroma from burning leaves of ocimum viridis, indoor residual spraying, use of mosquito coil, use of untreated nets, wearing of trousers, long sleeve shirt and stockings at night, physically killing mosquitoes by hand, and most recently, use of insecticidal nets. Roll Back Malaria (RBM) strategy for protecting against mosquito bite and reducing malaria burden is by sleeping under insecticidal nets regularly. [1],[2],[3],[4],[5] Scarcity of insecticidal nets at grass root level has been identified as one of the factors limiting universal coverage of the country with the net. [6] Government channel through which free long-lasting insecticidal net (LLINs) get to rural communities is considered inadequate, inaccessible, and unfriendly to most rural families. The current plan in 2008-2013 reviewed RBM plan period in Nigeria is universal coverage. This means that by the year 2013, about 80% of Nigerians will be sleeping under insecticidal nets, while 100% will have access to LLINs and sustain it. Barely few months to the end of the plan period, it does appear that some rural communities in Nigeria are yet to be covered with the nets. The study aims at finding out the rate of ownership and utilization of the treated nets by women of reproductive age in the study area. It also seeks to identify a channel for purchasing and distributing the nets that will be rural women-friendly in order to complement the existing government channel.
| Materials and Methods | |  |
A quasi-experimental study design was used. Villages rather than individuals formed the unit of allocation to experimental or control group for the purpose of introducing health promotion intervention with a channel of purchasing and distributing insecticidal nets that would be rural women-friendly. A multi-stage probability sampling method was used in selecting the study sample. From six local governments that make up Abia south senatorial zone, four were randomly selected; namely, obingwa, ugwunagbo, Ukwa East, and West local governments. From each local government selected above, two villages were randomly selected for the study. The first village selected in each local government area was assigned to the experimental group, while the second became the control group. A total of eight villages were selected. From the prepared sampling frame for each village, households that had women of reproductive age were systematically selected for interview. The study population was 2176 households gotten by enumeration of all the eight villages. Sample size was 400 determined using Lut'z formula n = z 2 pq/d 2 as stated by Ejemot. [7] Sample sizes in experimental and control groups were 200 households respectively.
Instrument for data collection
Instruments for data collection were focus group discussion guide and questionnaire. The focus group discussion guide had ten open-ended questions that sought and obtained information on why many households did not own insecticidal nets even when it was given free at government health facilities. It also sought to find out in respondent's opinion, what could be done to make rural women own and use available treated nets. The questionnaire was used in collecting quantitative data. SECTION 'A' of the questionnaire sought and obtained information on respondent's socio-demographic and economic characteristics. SECTION 'B' captured information on ownership and utilization of insecticidal nets, while, SECTION 'C' was on factors/reasons for not owning or utilizing available nets in the homes. The questionnaire was structured, pre-tested in a pilot survey before being interviewer-administered on every woman of reproductive age within the selected households. Sixteen assistants, two from each village, were selected and trained on how to impregnate nets, hang nets properly on beds, and obtain sampling frame for each village.
Health promotion intervention activities involved
- A massive insecticidal net awareness campaign at the village council hall on the days of women meetings in the four experimental villages only.
- Health education on cause of malaria, its transmission, prevention, protection, control measures, and the benefits of insecticidal net.
- Cost-effectiveness of treated nets over all other protective measures against mosquito bite used in the communities.
- Practical participatory net hanging demonstration session.
- Re-channeling procurement and distribution of treated nets through community-based-women council leaders on a fixed-installment-payment basis (FIPB) and in the cost price recovery, if at cost. This channel of fixed-installmental-payment basis (FIPB) is their normal channel for accomplishing community development strides in the past. That is why this strategy of fixed-installment-payment is referred to as "Rural women-friendly." Not only that it made the cost of net appear affordable, but also made the net accessible at a short distance from their homes.
Data analysis
Data collected were analyzed quantitatively and qualitatively, using calculator and computer with SPSS package. Chi-square statistic was used in testing for statistical significance.
Ethical consideration
Approval to conduct the study was sought and obtained from the village head of studied villages. Personal consents of the individuals interviewed were sought and obtained before administering the questionnaire on them. Data collected were held in strict confidence.
| Results | |  |
The result of socio-demographic and economic characteristics of respondents indicated that the experimental and control groups were comparable [Table 1]. Ownership of treated net in the experimental group was 36.5% before and 91% after health promotion intervention (HPI). In the control group, where HPI did not take place, ownership of net was 38% before and 38.5% after HPI [Table 2]. HPI with complementary purchasing and distribution channel (CPDC) increased ownership of treated nets by 54.5% in the study area. The null hypothesis that HPI does not increase ownership of treated net was rejected (P < 0.005). Identified reasons for not owning the net included: Inability of most rural women to access the health facilities where insecticidal nets were given freely to women on completion of their babies' immunization schedule. Secondly, lack of home-based treated net purchasing and distribution channel that is rural women-friendly. That is to say that the net will be available and accessible at a walking distance from their homes and the price made affordable through fixed-installment-payment-basis. Other reasons are shown in [Table 3], which revolved around the aforementioned two.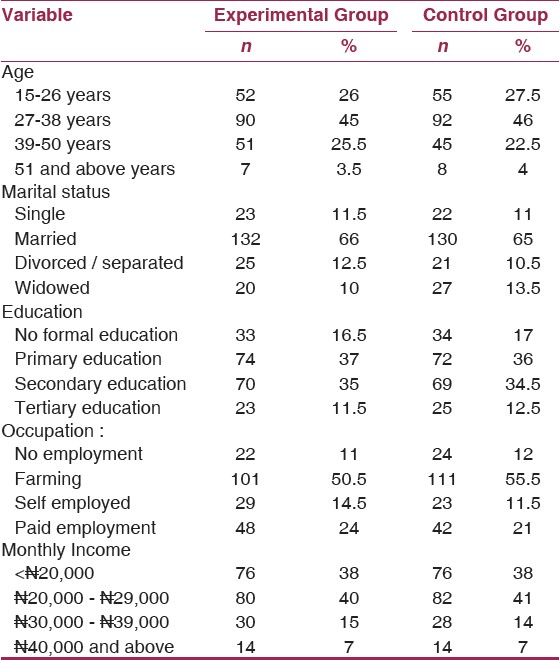 | Table 1: Socio – Demographic and Economic characteristics of respondents
Click here to view |
Utilization of available nets in the experimental group was 28.8% before HPI and 75.3% after HPI. In the control group, where the HPI did not take place, utilization of available net was 30.3% before and 32.5% after HPI [Table 4]. HPI with complementary purchasing and distribution channel (CPDC) increased utilization of treated nets by 46.5% in the study area. The null hypothesis that HPI does not increase utilization of treated nets was rejected (P < 0.005) [Table 4]. Identified reasons for not utilizing available treated nets before HPI are shown in [Table 5]. Topmost reasons were hot weather discomfort while sleeping under the net and illusory fears about the chemicals used in treating the nets. About 92.4% of those who did not make use of their own net claimed that insecticide could kill both mosquitoes and human beings. Some respondents claimed that their skin was allergic to chemicals used in treating nets by causing rashes on both mother and baby, including fetuses in pregnant women. Other reasons adduced for not utilizing available nets included fear of suffocating under the net due to small limited air that could pass through the tiny net holes. Some argued that they preserved their nets inside trunk boxes because they did not know how to hang them. The women who did not own a bed but slept on mud floor with mat said that using their net disturbed sexual convenience and as such, exchanged the nets for monetary reward. Some respondents converted theirs into shawls, hand gloves for ceremonial decorations. Very few respondents said that their nets were in bad condition and could not be used [Table 5].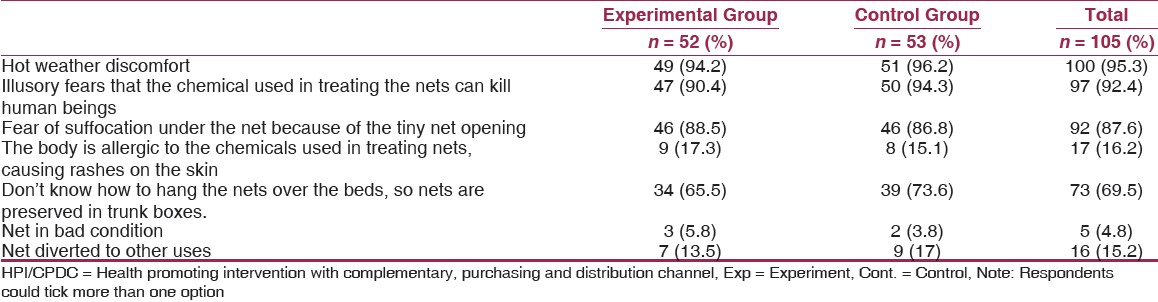 | Table 5: Identified reasons for not utilizing available treated nets before HPI
Click here to view |
The result of the various focus group discussions indicated that ignorance about the cause of malaria and proper protective measures against mosquito bites were major constraints in owning and using insecticidal nets in rural communities. Some people held tenaciously to the traditional belief the malaria is caused by evil men (witches and wizard), or by eating oily/fatty foods for long time. These beliefs were handed down to them from generation to generation and could not be changed. All the focus groups identified three of the following as the cause of malaria;
- …"malaria is caused by plasmodium species"…
- …"it is mostly caused by too much oily food"
- …"evil forces, witches and wizards cause malaria.
All the focus groups pointed out that "lack of money to buy net was the greatest reason for not owning a net in the homes." Some, especially the male group, said …. We can't spend our money to buy insecticidal nets; after all, how much do we get a day as income? "No job."
Suggested means of encouraging ownership and utilization of treated nets included:
- Distributing nets freely to women through women council leaders or health workers on house-to-house immunization programs in villages.
- If at a cost, payment should be by fixed-installmental-basis.
Some male participants in the focus group discussion mentioned four ways of scaling up ownership and utilization of the nets:
- By communal palm fruit harvest and the proceed used in offsetting the cost of nets.
- Husbands should serve as reminder to their wives to sleep under their nets regularly every night.
- Net assistants should go round demonstrating how to hang nets over the beds.
| Discussion | |  |
The finding in [Table 2] and [Table 4] that ownership and utilization of treated nets were as low as 36.5% and 28.8%, respectively, is indicative of high scarcity of the nets at the grass root level. Low level of ownership and use of treated nets found in this study is in line with earlier reports elsewhere in Africa south of Sahara, that despite the proven highly effectiveness of the net in preventing malaria and its burden, ownership and use is still very low. [1],[2],[3],[8],[9],[10],[11],[12],[13],[14],[15],[16] The findings that rate of ownership and utilization of treated nets increased significantly after health promotion intervention with complementary purchasing and distributing channel (HPI'/CPDC) were indicative of the effectiveness of this strategy. The finding in [Table 3] that unaffordability of the cost of treated nets limited ownership of the nets is in keeping with previous works done by other researchers [6],[9],[17],[18] that purchase of net at cash-and-carry-basis appeared unaffordable to most rural families. However, Guigemde [19] argued that treated nets were affordable to many individuals in malarious endemic areas, when compared with what they spend on other, often less effective preventive methods. His view was also up-held by Enato and Okhamafe. [20] Other limiting factors to ownership of treated nets identified in the study were addressed during the interventional activities.
Ignorance about the cause of malaria, its transmission, and proper protective measures against mosquito bite was addressed using health education and health promotion intervention (HPI). HPI has been reported to be effective in bringing about behavioral change in ownership and utilization of treated nets. [9],[10],[21] The finding that hot weather discomfort is a major reason for not utilizing available nets in the study area [Table 5] is in keeping with the report of Offiah [15] and Salako. [22] The illusory fears identified in [Table 5], as reasons for not using the available nets in homes, were similar to findings of Amajoh [23] that insecticidal smell could irritate users of treated nets as some people may be allergic to the insecticide. These fears and beliefs were due to ignorance as reported by Obionu [4] and were allayed during the HPI. Scarcity of the nets at the grass root was addressed by complementing the government distribution channel that stopped at the health facilities, with alternative channel that got to the grass root through the involvement of the local women organization council. The women council leaders were involved in the distribution of the nets and at the cost price recovery on installmental-payment-basis. Similar interventional studies elsewhere had demonstrated remarkable increase in ownership and utilization of treated nets when individuals received health promotion activities and nets made available and accessible to them. [9],[10],[13],[14],[23],[24],[25],[26] We wish to recommend this HPI/CPDC strategy to other developing countries having similar socio-economic and cultural practices for rapid scaling up of ownership and utilization of insecticidal nets.
| References | |  |
| 1. | Federal Ministry of Health (FMOH). National Malaria Control Programme in Nigeria, Abuja: 2005 Report. 
|
| 2. | Oresanya OB, Hoshen M, Sofola OT. Utilization of insecticide treated nets by under five children in Nigeria: Assessing progress towards the Abuja targets. Malar J 2008;7:145-52. 
|
| 3. | WHO. Malaria Vector Control and Personal Protection Report of a WHO Study Group (online) Geneva: WHO; 2006. Available from: http.// www.who.int/malaria/docs/WHO-TRS-9365.pdf. Last accessed in 2006]. 
|
| 4. | Obionu CN. Primary health care for developing countries. Enugu: Ezu Book Ltd. Publishers; 2007. 
|
| 5. | Lucas AO, Gilles HM. Short Textbook of Public Health Medicines for the Tropics. Revised 4 th ed. Malta: Book Power Publishers; 2007. 
|
| 6. | Federal Ministry of Health (FMOH). National Malarial and Vector Control Programmed in Nigeria, Guidelines for implementation of long lasting insecticidal Mosquito Nets in Nigeria. Abuja: Primo Wonder Ltd. Publishers; 2010. 
|
| 7. | Ejemot-Nwadiaro RI. A Guide to Biostatistics and Health Research methods. Calabar: Data Pro; 2009. 
|
| 8. | Iwuala CC, Sutherland C. The roll back malaria programme. A review of progress in Africa (11). Int J Environ Health Hum Dev 2005;6:28-47. 
|
| 9. | Rhee M, Sissoko M, Perry S, Dicko A, McFarland W, Donmbo O. Malaria prevention practices in Mopti Region, Mali. East Afr Med J 2005;82:240-8. 
|
| 10. | Elsheikh IE. Effectiveness of communication for behavioural impact (COMBI) strategy in increasing utilization rate of insecticide treated nets (ITNs). Blue Nile State. Sudan J Public Health 2007;2:365-8. 
|
| 11. | Onwujekwu O, Hanson K, Fox-Rushby JA. Who buys insecticide treated nets? Implications for increasing coverage in Nigeria. Health Policy Plan 2003;18:279-89. 
|
| 12. | Kweku M, Webster J, Taylor I, Burns S, McDamien D. Public delivery of insecticide treated nets. A voucher scheme in Volt Region, Ghana. MaIar J 2007;6:14. 
|
| 13. | Macintye K, Keating J, Okbalt YB, Zerom M, Sosler S, Ghebremeskel T, et al. Rolling out insecticide treated nets in Eritrea: Examining the determinants of possession and use in Malarious zones during the rainy season. Trop Med Int Health 2006;11:824-33. 
|
| 14. | San-Clamente CA. Nuru international Community Health Worker Model Tackless Malaria Prevention in Kuria, Kenya 5 Startling Statistics for World Health Malaria Day 2011. Available from: http://www.prwob.com/releases/2011/4/prweb8333635.htm [Last accessed on 2011 Apr 25]. 
|
| 15. | Offiah RM. Factors Associated with Acceptability and Use of ITNs Among Women of Reproductive Age in Andoni L.G.A., Rivers State Nigeria. Unpublished MPH thesis, University of Calabar, Nigeria. 
|
| 16. | Chapman RR. Chikotsa-secrets, silence, and hiding: Social risk and reproduction vulnerability in Central Mozambique. Med Anthropol 2006;20:487-515. 
|
| 17. | Nuwaha F. People′s perception of malaria in Mbarare, Uganda. Trop Med Int Health 2002;7:467-70. 
|
| 18. | Nwosu UM, Emereole CO, Uwakwe KA. Factors influencing ownership and utilization insecticide-treated nets in rural communities of Abia State, Nigeria. Int J Environ Health Hum Dev 2010;11:49-59. 
|
| 19. | Guigemde TR, Dao F, Cuntis V, Traore A, Sonoh B, Testa J, et al. Household expenditure in the town of Bobo - Dioulasso, Burkina-Faso. Tran R Soc Med Hyg 1994;88:285-7. 
|
| 20. | Enato EF, Okhamafe AD. Plasmodium falciparum malaria and antimalarial interventions in sub-saharan Africa: Challenges and Opportunities. Afr J Biotech 2005;4:1598-605. 
|
| 21. | Brieger B. Malaria matters: Advocating for a malaria-free future. Available from: http://www.google.com.ng/search hl & malaria free future.Org. [Last accessed in 2008]. 
|
| 22. | Salako LA. Malaria and its control in Nigeria, Nigerian Institute of Medical Research Lagos, 1993. 
|
| 23. | Amajoh CN. Advantages of ITNs. Nigerian Medical Association Special Focus 2001;1:12-3. 
|
| 24. | Magadi MA, Agwanda AO, Obare FO. Comprehensive Analysis of the use of Maternal Health Services between teenagers and older mothers in Sub-saharan Africa: Evidence from Demographic and Health Survey (DHS). Soc Sci Med 2007;64:1311-25. 
|
| 25. | Morse JM. Culture variation in behavioural response to participation childbirth in Figi. Med Anthropol 1999;12:35-54. 
|
| 26. | Beninguisse G, De Brouswere V. Tradition and Modernity in Cameroon: The confrontation between social demand and biomedical Logics of health of health services. Afr J Reprod Health 2004;8:152-75. 
|
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
|