|
 
 |
|
ORIGINAL ARTICLE |
|
|
|
| Year : 2012 | Volume
: 18
| Issue : 3 | Page : 294-298 |
| |
Hemoglobinopathies in South Gujarat population and incidence of anemia in them
Ankur G Patel, Avani P Shah, Smita M Sorathiya, Snehalata C Gupte
Surat Raktadan Kendra and Research Centre, (NABH Accredited Regional Blood Transfusion Centre), Surat, Gujarat, India
| Date of Web Publication | 4-Mar-2013 |
Correspondence Address:
Snehalata C Gupte
Surat Raktadan Kendra and Research Centre 1st Floor, Khatodara Health Centre, Besides Chosath Joganiyo Mata's Temple, Udhana Magdalla Road, Khatodara, Surat - 394 210, Gujarat
India
 Source of Support: Surat Raktadan Kendra and Research Centre Management, Conflict of Interest: None
DOI: 10.4103/0971-6866.107979

 Abstract Abstract | | |
Objective: To Screen of South Gujarat population for determination of prevalence of different hemoglobinopathies particularly beta thalassemia trait (BTT) and sickle cell trait (SCT) and find out the incidence of anemia in them.
Material and Methods: The present study screened 32,857 samples of students from different school and colleges in South Gujarat. Blood samples were initially tested for solubility test and complete hemogram on hematology analyzer. Samples having MCV (≤78), MCH (≤28) and/or positive solubility test were investigated for Hb electrophoresis on cellulose acetate membrane (pH 8.6). Hb A 2 level ≥3.5% was considered as diagnostic for BTT. High performance liquid chromatography on Biorad Hb variant system was done on samples having doubtful results.
Result: Overall prevalence of BTT and SCT in South Gujarat was 4.4% and 1.3% respectively. Gamit, Vasava, Chaudhary, and Mahyavanshi castes had high prevalence of BTT (15.9%, 13.6%, 12.6%, and 6.9%) as well as SCT (22.2%, 15.2, 22.3, and 4.2%) respectively. Other communities like Lohana (10.8%), Sindhi (10.2%), Prajapati (6.3%), and Ghanchi (6.2%) also showed higher prevalence of BTT. Incidence of mild to moderate anemia was higher in BTT and SCT compared to non-BTT or non-SCT subjects.
Conclusion : Study suggests that BTT is the most prevalent hemoglobinopathy in South Gujarat. β-thalassemia and Sickle cell anemia are highly prevalent in Mahyavanshi, Chaudhary, Gamit, Vasava and Rohit. Prajapati, Lohana, Leva Patel, and Ghanchi have β- thalassemia risk. SCT is more frequently detected in Dhodia Patel and Kukanas.
Keywords: Hb D, Hb E, hemoglobinopathy, sickle cell trait, South Gujarat, β-thalassemia trait
How to cite this article:
Patel AG, Shah AP, Sorathiya SM, Gupte SC. Hemoglobinopathies in South Gujarat population and incidence of anemia in them. Indian J Hum Genet 2012;18:294-8 |
How to cite this URL:
Patel AG, Shah AP, Sorathiya SM, Gupte SC. Hemoglobinopathies in South Gujarat population and incidence of anemia in them. Indian J Hum Genet [serial online] 2012 [cited 2016 Jun 1];18:294-8. Available from: http://www.ijhg.com/text.asp?2012/18/3/294/107979 |
 Introduction Introduction | |  |
Hemoglobinopathies are more common in Gujarat compared to other Indian states. Model and Petrou [1] have estimated 12% incidence of major hemoglobinopathy traits in Gujarat. β-thalassemia is the most common single gene disorder in our country. About 7500 to 12000 β-thalassemia major infants are born in India every year. [2] Several studies have revealed high prevalence of beta thalassemia trait (BTT) in some caste groups in Gujarat. [3],[4] Abnormal hemoglobins D, J and L have been reported in Cutchi Lohana community of Gujarat. [3] Certain castes and tribes in Gujarat are yet to be investigated for β-thalassemia and other abnormal hemoglobins.
About 10-15% of the tribal population of India is in Gujarat, particularly in South Gujarat and prevalence of sickle cell trait (SCT) varies from 0 to 31.4% among different tribes. [5] In India, sickle hemoglobin was first discovered by Lehman and Cutbush about 50 years ago among the tribles of Nilgiri hills of Southern India. [6] The gene is not confined to tribal peoples, but is prevalent in scheduled castes and some Hindu castes. [7]
Present study is an attempt to screen for hemoglobinopathies in South Gujarat population with an objective to investigate some of the communities which have never been screened for hemoglobinopathies. Simultaneously we plan to find out the incidence of anemia in BTT and SCT cases.
 Materials and Methods Materials and Methods | |  |
The study was approved by our Institutional ethics committee and commenced in the year 2007. The study participants are mainly students from different colleges of Veer Narmad South Gujarat University. Camps were also organized in schools and in community gathering events. Only unrelated subjects were included in the study. Necessary permission was obtained from the university or respective college or school principals. An informed consent was taken from all subjects who were more than 18 year old. Consent forms were singed by college authority as their guardians, if students were <18 years old. The information like name, age, sex, address, phone number, religion, caste, sub-caste, previous transfusion history etc. was filled in forms.
Two ml of blood sample was collected in EDTA tubes. Complete blood count was measured on the NIHON KOHDEN fully automated or semi-automated cell counter (MEK-6318 or MEK-5216k). Solubility test [8] was carried out on all samples to identify subjects suspected to have SCT or Sickle cell disease (SCD). All samples having Mean cell volume (MCV) ≤78 fl and/or Mean cell hemoglobin (MCH) ≤28 pg were investigated for HbA 2 and positive solubility test were investigated for Hb S by Hb-electrophoresis. [8] The electrophoresis was carried out on cellulose acetate using TEB buffer, pH 8.6. [8] HbA 2 was estimated following elution after electrophoresis. The samples having HbA 2 levels >3.5% were labeled as having β-thalassemia trait (BTT). Further confirmation was done by using BIO-RAD "VARIANT" (beta-thalassemia short program) high performance liquid chromatography (HPLC) system. The samples having HbA 2 between 3 to 4 % were also run on HPLC. Parents were investigated on HPLC if the BTT or SCT diagnosis was doubtful. Sickling test was performed for all cases of Hb S to conform the presence of sickle shape RBC. [8]
 Result Result | |  |
Total 32,857 blood samples were screened for BTT, SCT and other hemoglobinopathies during the period of study. Out of them, 30,953 were normal and 1904 had various types of hemoglobinopathies.
[Table 1] shows the prevalence of different hemoglobinopathies in study participants. Among different hemoglobinopathies prevalence of BTT was the highest. Other hemoglobin like Hb E and Hb D were found in Hindu population and one case of Hb E in Muslim community. Most of the Hb E cases were among the migrants from Bengal, UP, Manipur and Dhor from Maharashtra.
Five out of 12 Hb D subjects were of Leva Patel caste and remaining were from Sindhi Lohana, Thkkar, Rajput, Lohar and Yadav communities.
[Table 2] shows prevalence of different hemoglobinopathies amongst different religions. Majority of the subjects were Hindu. The prevalence of BTT was higher with 4.7% prevalence in Muslims followed by 4.4% in Hindus and 4.0% in Jains. χ2 test did not reveal significant difference in prevalence of BTT in these three religions (P > 0.1). Jain community had very low prevalence of SCT compared to Hindu (χ2 = 14.3 for 1 df, P < 0.001) and Muslims (χ2 = 10.9 for 1 df, P < 0.001).
Further analysis revealed that out of 10 cases of SCD nine were Hindu and one Muslim. Other hemoglobins like Hb E (8) and Hb D (12) were also found among Hindu individuals and there was one case of Hb E in Muslim.
[Table 3] shows prevalence of BTT and SCT in different caste groups. Gamit, Chaudhary and Vasava tribal communities showed the highest prevalence of both BTT and SCT, followed by Mahiyavanshi and Rohit. Lohana, Sindhi, Prajapati and Ghanchi showed high prevalence of BTT but low prevalence of SCT. Statistically significant difference was found in prevalence of BTT and SCT between different caste groups (P < 0.001). Analysis of different Jain and Muslim castes was not done as the samples size was very small. Three cases of SCD were found in each Chaudhary and Gamit, one case was found in Vasava community.
In this study, large number of samples were of Patel community therefore they were further classified as per their sub-castes as shown in the [Table 4]. Kukanas have the highest prevalence of BTT but the sample size was too small for any conclusion. In Leva, Kachhiya, Koli and Dhodia Patels BTT prevalence ranged from 3.7% to 4.9%. Five cases of hemoglobin D was also found in Leva patel. On comparison of prevalence of BTT and SCT in different sub-caste groups, significant difference was found between them.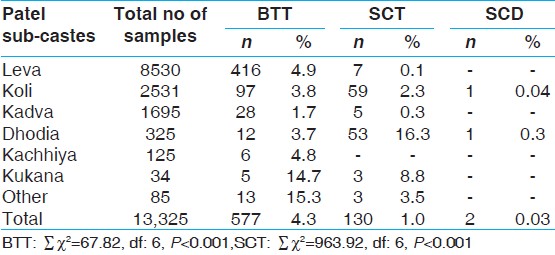 | Table 4: Prevalence of abnormal hemoglobinopathies in sub-castes of Gujarati patel
Click here to view |
[Table 5] shows the Hemoglobin distribution among the male and female individuals having BTT, SCT and normal subjects negative for any hemoglobinopathy. Severe anemia with Hb concentration ≤7g/dl was observed in <1% individuals. Majority of individuals had mild anemia with Hb concentration between 10 to 12.9 g/dl in males and 10 to 11.9 g/dl in females. The incidence of anemia was predominantly high in BTT males and females (P < 0.001) and SCT males and females compared to normal individuals.
 Discussion Discussion | |  |
The Indian population comprises numerous castes and tribal groups, each revealing different genetic traits. Several studies in the literature have reported that Gujarat has higher frequency of β-thalassemia and sickle cell disease. [3],[4],[9],[10] Therefore prospective studies are essential to identify high risk communities. Premarital screening of college students not only gives prevalence in different caste groups but also helps in counseling and prenatal diagnosis programs for prevention of birth of an affected child.
Overall prevalence of BTT in this study was 4.4%. Hindu, Muslim and Jain communities had comparable prevalence. In a multicentric collaborative study of Indian council of medical research (ICMR) 2.8% Shiya and 2.5% Sunni Muslims in Mumbai had BTT whereas in Delhi 1.7% BTT was reported in Sunni Muslim. [11] Jain community in Mumbai and Delhi had 3.3% and 4.8% BTT prevalence respectively. In our study 4.0% prevalence was observed in this community.
The Gamit, Chaudhary, Vasava tribals and Lohana, Sindhi non-tribal communities had greater than 10% prevalence of BTT. Gamit tribals from Surat district have been investigated for SCT and SCD by Vyas et al. [9] but there are no reports of BTT studies in them. Cutchhi, Halai and Sindhi Lohanas have been studied by Bhatia et al. [3] and 10.7%, 17.2% and 6.8% prevalence of BTT respectively has been reported in them. Mulchndani et al. [12] have reported 16.81% prevalence of BTT in Sindhis which is higher than that reported in our study. Prajapati, Ghanchi, Mahiyavanshi (non-tribal) and Rohit (tribal) communities also had high prevalence ranging from 6.2 to 6.9%. Prajapati and Ghanchi are one of the most prevalent castes of South Gujarat. But we could not find any hemoglobinopathy study on them. Rohits have been studied earlier for SCT [5] but not for BTT. Gamit, Chaudhary, Vasava, Mahyavanshi and Rohit had the high prevalence of both BTT and SCT. Overall prevalence of BTT was 4.3% in Patel caste, with highest prevalence in Kukana followed by Kachhiya and Leva Patel.
Tribal population in many states has been screened for SCT and SCD. [13] SCT prevalence reports on Bhils, Gamit, Dhodia, Dubla, Koli, Naika, Rohit, Konkana tribes are available. [5],[13] However we did not find any published report on Vasava. We observed 13.6% BTT and 15.2% SCT in them. Mahiyavanshi which is a non-tribal caste group had 4.3% SCT prevalence. To our knowledge there are no reports on Mahyavanshi community which has beta thalassemia and sickle cell genes.
Besides Hb S we also found other two abnormal hemogloglobins D and E. Out of 32,857 blood samples, 21 were positive for these two hemogloglobins. Hb D was first reported in Sikh community and later on 326 Gujarati individuals living in Uganda were found to have this abnormal Hb. [14] In our study five out of 12 Hb D subjects were of Leva Patel caste. This community also had 4.9% prevalence of BTT. Hb E was prevalent in migrants coming to Surat from North-East and North India. Literature reports high frequency of Hb E in Benglis and Assamese. [14]
Literature suggests that iron deficiency is less common in BTT. [15],[16] In the present study over all incidence of mild to moderate anemia was 75.1% in BTT, 42.8% in SCT and 31.1% in normal subjects, negative for any hemoglobinopathy. In Sindhi community also anemia is more common in BTT male and females compared to non-BTT individuals. [12] However as anemia is not due to iron deficiency iron therapy is ineffective in these cases.
 Conclusion Conclusion | |  |
Study suggests that BTT is the most prevalent hemoglobinopathy in South Gujarat. Mahyavanshi, Chaudhary, Gamit, Vasava and Rohit are at high risk for both β-thalassemia as well as Sickle cell anemia while Prajapati, Lohana, Leva Patel, and Ghanchi are high risk communities for β-thalassemia. Leva Patel subjects also have Hb D gene. Dhodia Patel and Kukanas are high risk communities for sickle cell anemia. Mild to moderate anemia is more frequently present in BTT and SCT subjects compared to normal individuals.
 Acknowledgment Acknowledgment | |  |
We are grateful to the management of Surat Raktadan Kendra and Research Center for financial support. We gratefully acknowledge the grant given by Lions Club International Fund for equipment.
 References References | |  |
| 1. | Modell B, Petrou M. The problem of the hemoglobinopathies in India. Ind J Hematol 1983;1:5-16. 
|
| 2. | Gorakshakar AC, Colah RB. Cascade for β-thalassemia: Apractical approach for identifying and counseling in India. Indian J Community Med 2009;34:354-6. 
[PUBMED]  |
| 3. | Bhatia HM, Shanbagh SR, Baxi AJ, Bapat JP, Sharma RS. Genetic studies among the endogamous groups of Lohanas of North and West India. Hum Hered 1976;26:298-305. 
|
| 4. | Mukherjee MB, Gangakhedkar RR, Sathe MS. Abnormal hemoglobin, G6PD deficiency and their pattern of interaction in the tribal population of Valsad district (Gujarat). Indian J Hematol Blood Transf 1993;11:227-31. 
|
| 5. | Bhatia HM, Rao VR. Genetic atlas of Indian tribes. Bombay, India: Institute of Immunohaematology (ICMR) publication; 1986. p. 263-73. 
|
| 6. | Lehman H, Cutbush M. Sickle-cell trait in Southern India. BMJ 1952;1:404-5. 
|
| 7. | Kar BC. Sickle cell disease in India. J Assoc Physician India 1991;39:954-60. 
|
| 8. | Dacie JV, Lewis SM. Practical Hematology.10 th ed. Philadelphia: Churchill Livingstone; 2010. p. 281-3. 
|
| 9. | Vyas GN, Bhatia HM, Sukumaran PK, Balkrishanan V, Sanghvi LD. Study of blood groups, abnormal hemoglobins and other genetical characters in some tribes of Gujarat. Am J Phys Anthropol 1962;20:255-65. 
|
| 10. | Sukumaran PK. Abnormal hemoglobins in India. Trends in hematology. In: Sen NN, Basu AK, editors. Culcutta, India: Saraswati press; 1975. p. 225-36. 
|
| 11. | Madan N, Sharma S, Sood SK, Colah RB, Bhatia LH. Frequency of β-Thalassemia trait and other hemoglobin in northern and western India. Indian J Hum Genet 2010;16:16-25. 
[PUBMED]  |
| 12. | Mulchandani DV, Fulare MB, Zodpey SP, Vasudev ND. Prevalence and some epidemiological factors of beta thalassemia trait in Sindhi community of Nagpur city, India. Indian J Public Health 2008;52:11-5. 
[PUBMED]  |
| 13. | Balgir RS. Distribution of sickle cell hemoglobin in India. Indian J Hemat 1988;6:1-14. 
|
| 14. | Chatterjea JB. Hemoglobinopathies, glucose-6-phosphate dehydrogenase deficiency and allied problems in the Indian subcontinent. Bull World Health Organ 1966;35:837-56. 
|
| 15. | Mehta BC, Pandya BG. Does beta thalassemia trait protect against iron deficiency? Indian J Hemat 1987;5:59-62. 
|
| 16. | Mehta BC, Gandhi S, Kamath P. Survey of children of the Lohana community in Bombay for Beta thalassemia trait and Iron deficiency. Int J Hematol 1989;7:63-6. 
|
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
| This article has been cited by | | 1 |
Epistasis and the sensitivity of phenotypic screens for beta thalassaemia |
|
| Bridget S. Penman,Sunetra Gupta,David J. Weatherall | | British Journal of Haematology. 2014; : n/a | | [Pubmed] | [DOI] | |
|
 |
|






