|
 
 |
|
ORIGINAL ARTICLE |
|
|
|
| Year : 2013 | Volume
: 19
| Issue : 2 | Page : 150-153 |
| |
Body composition in Egyptian Turner syndrome girls
Moushira Erfan Zaki1, Hanan H Afifi2
1 Department of Biological Anthropology, Medical Research Division, National Research Centre, Cairo, Egypt
2 Department of Clinical Genetics, Human Genetics and Genome Research Division, National Research Centre, Cairo, Egypt
| Date of Web Publication | 5-Aug-2013 |
Correspondence Address:
Moushira Erfan Zaki
Department of Biological Anthropology, Medical Research Division, National Research Centre, Cairo
Egypt
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0971-6866.116108

 Abstract Abstract | | |
Objective: This cross-sectional study was undertaken to construct the new body fat % curve and provide body composition reference data for adolescent girls with Turner syndrome (TS). They diagnosed cytogenetically by blood karyotyping and not treated with growth hormone (GH).
Materials and Methods: The study included 70 TS girls from age 13 years to age 17 years. Body composition was measured by bioelectrical impedance. Smoothed centile charts were derived by using the least mean square (LMS) method.
Results: The new body fat curves reflect the increase of body fat mass (FM) from age 13 years to age 17 years. Body FM % of Egyptian TS girls was lower when compared with age-matched American untreated TS girls.
Conclusion: This study presents the new body fat curves and reference values of body composition for untreated Egyptian TS adolescent girls. The present charts can be used for direct assessment of body FM % for Egyptian TS girls and evaluation for cases on GH treatment or other growth promoting therapy.
Keywords: Body fat mass, Egyptians, Turner syndrome
How to cite this article:
Zaki ME, Afifi HH. Body composition in Egyptian Turner syndrome girls. Indian J Hum Genet 2013;19:150-3 |
 Introduction Introduction | |  |
Turner syndrome (TS) is one of the most common chromosomal abnormalities, its incidence being between 1/2500 and 1/5000 live births among girls. [1] In approximately 50% of the cases, the karyotype anomaly is 45 × monosomy; however, a variety of other anomalies, including mosaicism, Xp or Xq deletion, and isochromy of the X long arm are known. [2] Turner females are primarily growth retarded along the longitudinal axis. The short stature in TS is attributed in a large part to haploinsufficiency for the pseudoautosomal gene Short stature homeobox protein SHOX. Although girls with TS are not usually growth hormone (GH) deficient, treatment with exogenous recombinant human GH is widely used to augment adult height. [3] Body composition is altered in TS. Numerous factors seem to influence the decreased lean body mass (LBM) and the increased fat mass (FM), such as sex hormones, the growth hormone (GH)/insulin-like growth factor 1 (IGF-1) (GH/IGF) system, maximal oxygen uptake (or physical fitness), insulin sensitivity, ghrelin and leptin, and possibly other factors. [4] Distinct differences in the regional body composition were present in young TS girls (9-15 years) in comparison with age- and body mass index (BMI)-matched controls. [5] Therefore, TS has been characterized as a syndrome of disproportionate body composition. [6]
The aim of this study was to construct the new body fat centiles for Egyptian untreated TS and to present the body fat references.
 Materials and Methods Materials and Methods | |  |
The study included 70 females with TS recruited from the out-patient clinic of Clinical Genetics Department, National Research Centre (NRC). Upon entry in the study, all subjects received oral and written information concerning the study, before giving written informed consent. The protocol was approved by the NRC ethical scientific committee. Each patient was subjected to history taking, pedigree construction and analysis, meticulous clinical examination of all body systems and essential body anthropometric measurements. Standard cytogenetic analysis following GiemsaTequnique Banding GTG banding technique was carried out for all patients on metaphases derived from the phytohemagglutinin stimulated peripheral blood lymphocytes by standard methods. [7] A total of 50 metaphases were karyotyped and analyzed according to International System of Human Cytogenetic Nomenclature (ISCN) [8] (2005).
Classic TS 45, X karyotype was found in 78.6% of cases (n = 55), 45, X/46, XX in 14.3% (n = 10), 45, X/46, X, i (Xq) in 4.3% (n0 = 3) and 45, X/46, X, r (X) in 2.8% (n = 2).
Body composition analyzer (Tanita Corporation, Tokyo, Japan) with correction for light indoor clothing was used to measure the body composition parameters. The measurement procedure required the subject to stand in bare feet on the analyzer and to hold a pair of handgrips, one in each hand. The bio-impedance component of the measurements took approximately 30 s/subject. BMI was calculated as weight (kg)/height 2 (m). Bioelectrical impedance analysis (BIA) can measure the electrical properties of living things. The prediction equations used in this model are based on bio-impedance, weight, height, and age and were derived from the calibration studies against whole-body dual X-ray absorptiometry. The bioelectrical impedance was used to measure conductivity in the body. The method is based on the fact that the lean tissue of the body is much more conductive due to its higher water content than fat tissue. The BIA can measure and track changes in the amounts of body fluids, fat, and LBM, which includes muscles and organs. The BIA distinguishes where the water is located in body-either intracellular or extracellular. Functionally, the BIA assesses how much of the body is acting as functioning cells, transport tissue or storage cells (fat).
Statistics
Data is presented as means with the standard deviation (SD) or as proportions. Statistical analysis and centile curves for body fat percentage were constructed for TS girls using the least Mean Square LMS method, which summarizes the data in terms of three smooth age-specific curves, namely L (lambda), M (mu), and S (sigma). The M and S curves correspond to the median and co-efficient of variation of body fat percentage at each age whereas, the L curve allows for the age-dependent skewness in the distribution of body fat percentage. For the construction of the percentile curves, data were imported into the LMS software (version 1.25) and the L, M, and S curves estimated. Five centiles curves were calculated from the 2 nd to the 98 th .
 Results Results | |  |
[Table 1] shows the means and SD reference values of body composition of TS girls aged from 13 years to 17 years. Body FM % increased up to age 14 year with a marked increase after age 15 year. Fat free mass (FFM) % increases slightly by age, while lean/fat ratio and total body water percentage (TBW %) decrease up to age 17 years.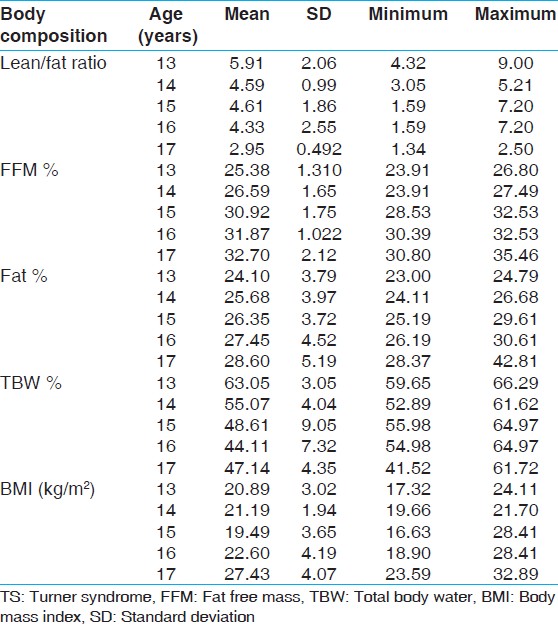 | Table 1: Body compositional reference values of Egyptian TS girls by age groups
Click here to view |
[Figure 1] illustrates curves of body fat % at 2 nd , 75 th , 50 th , 25 th , and 98 th centiles for Egyptian untreated TS girls aged 13-17 years. The 50 th centile continues to rise, and the other centiles diverge from the 50 th centile. TS girls show a relatively flat 50 th centile ranged between 24% and 28% body fat over the entire age range. BMI was ranged between 20 kg/m 2 and 27 kg/m 2 over the entire age range.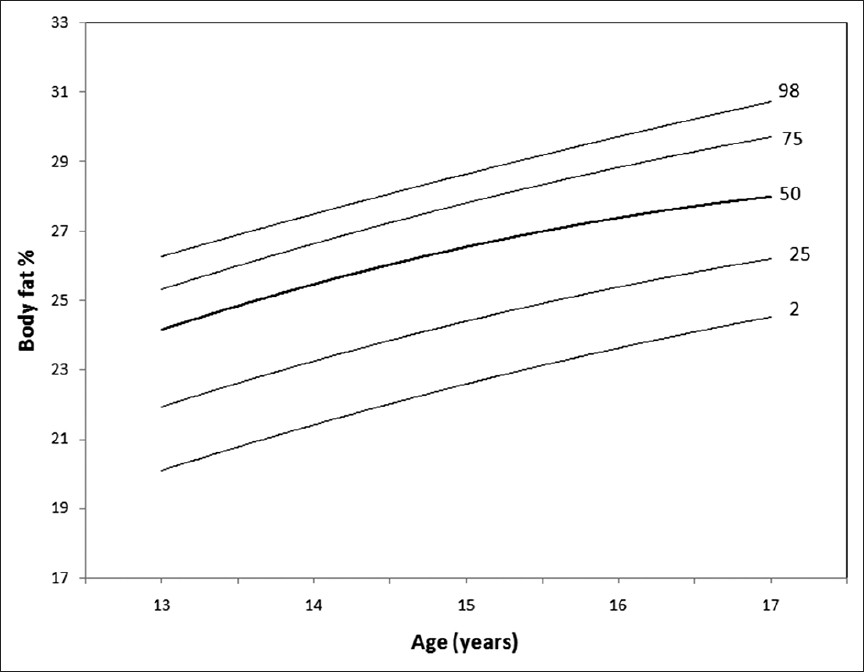 | Figure 1: Body fat centile curves for Turner syndrome girls aged 13 - 17 years
Click here to view |
 Discussion Discussion | |  |
In this study, we found no relation between karyotype and any of the measured variables. The present data showed that body composition in the untreated TS girls is profoundly changed, with increased amounts of body fat when compared with normal standard Egyptian controls. [9] On the other hand, the present study showed that body FM % was lower in our cases compared with age-matched American untreated TS girls. [10] It has shown that GH-treated individuals had on average 15% less adipose tissue and approximately 8% more lean mass compared with untreated girls. GH treatment is well-known to promote anabolism of lean tissue and reduce adiposity in adults, with or without GH deficiency. [11] Two small longitudinal studies showing that GH treatment increased lean mass and decreased adiposity in girls with TS. Leger et al. [12] found increased thigh muscle volume in eight girls with TS over 12 months of GH treatment, and Gravholt et al. [5] observed increased muscle and decreased fat after 2 months of GH treatment. Body composition, gender, age, and spontaneous GH secretion have been shown to be interrelated. Obesity is associated with low circulating levels of GH, [13] a situation that can be reversed by weight loss. [14],[15]
BMI in Turner's syndrome was unchanged by treatment with sex hormone, whereas significant increases in FFM and the TBW/FFM ratio were seen with sex hormone treatment. [16] The average BMI in this study was between 20 kg/m 2 and 27 kg/m 2 over the entire age range. The present data showed that TS girls were overweight when compared with age matched Egyptian controls, with a higher FM. [9] FM and BMI have been found to be higher in adult Turner patients compared with age matched controls, and LBM is inappropriately low, which is similar to the present findings. [17]
Previous studies reported marked differences in regional body composition in young TS girls (9-15 years), in comparison with age-and BMI-matched controls in two different study groups. [5] The authors reported that overweight TS girls have smaller skinfold thickness compared to equally overweight girls and suggested that this difference may be due to either to hidden fat on the trunk, or to increased LBM. [18] Gravholt et al. [4] reported that females with UTS are overweight as a group when compared with a group of normal women, with a higher FM, a lower LBM, however, with a comparable amount of total body water (in %). However, the present study found decreased total body water %, in TS girls. Previous studies reported decreased subcutaneous fat content and the body composition in TS. [19],[20]
This study provides body fat references, which can be used to base a clinical judgment for obesity in Egyptian TS children and provides data to compare with other countries.
 Conclusion Conclusion | |  |
The present study presents a new centile curve for body fat body for untreated TS girls from 13 years to 17 years. This curve might use for clinical monitoring of body fat for TS girls, whereas the 2 nd centile and the 98 th centile as cut-off points for under-fat and over-fat girls, respectively.
 References References | |  |
| 1. | Gravholt CH, Juul S, Naeraa RW, Hansen J. Prenatal and postnatal prevalence of Turner's syndrome: A registry study. BMJ 1996;312:16-21. 
|
| 2. | Fergusson-Smith M. Genotype-phenotype correlations in Turner syndrome. In: Hibi I, Takano K, editors. Basic and clinical approach to Turner syndrome. Amsterdam: Elsevier Science; 1993. p. 17-25. 
|
| 3. | Sas TC, de Muinck Keizer-Schrama SM, Stijnen T, van Teunenbroek A, van Leeuwen WJ, Asarfi A, et al. Bone mineral density assessed by phalangeal radiographic absorptiometry before and during long-term growth hormone treatment in girls with Turner's syndrome participating in a randomized dose-response study. Pediatr Res 2001;50:417-22. 
|
| 4. | Gravholt CH, Hjerrild BE, Mosekilde L, Hansen TK, Rasmussen LM, Frystyk J, et al. Body composition is distinctly altered in Turner syndrome: Relations to glucose metabolism, circulating adipokines, and endothelial adhesion molecules. Eur J Endocrinol 2006;155:583-92. 
|
| 5. | Gravholt CH, Naeraa RW, Brixen K, Kastrup KW, Mosekilde L, Jørgensen JO, et al. Short-term growth hormone treatment in girls with Turner syndrome decreases fat mass and insulin sensitivity: A randomized, double-blind, placebo-controlled, crossover study. Pediatrics 2002;110:889-96. 
|
| 6. | Gravholt CH, Hjerrild BE, Naeraa RW, Engbaek F, Mosekilde L, Christiansen JS. Effect of growth hormone and 17beta-oestradiol treatment on metabolism and body composition in girls with Turner syndrome. Clin Endocrinol (Oxf) 2005;62:616-22. 
|
| 7. | Verma RS, Babu A. Human chromosomes: Principal and Techniques. 2 nd ed. San Francisco: Mc Graw-Hill Inc.; 1995. 
|
| 8. | ISCN. An International system of human cytogenetic nomenclature. In: Mitelman F, editors. Karger, Basel: Krager; 2005. 
|
| 9. | Hassan NE, El Masrey SA, Zaki ME. Standards of fat free mass and body fat mass indices for egyptian children and adolescents. Med J Natl Res Cent 2005;1:5-30. 
|
| 10. | Ari M, Bakalov VK, Hill S, Bondy CA. The effects of growth hormone treatment on bone mineral density and body composition in girls with Turner syndrome. J Clin Endocrinol Metab 2006;91:4302-5. 
|
| 11. | Bengtsson BA, Johannsson G. The use of growth hormone in adults: A review of the last 10 years, the present and a perspective for the future. Growth Horm IGF Res 1998;8:27-35. 
|
| 12. | Leger J, Carel C, Legrand I, Paulsen A, Hassan M, Czernichow P. Magnetic resonance imaging evaluation of adipose tissue and muscle tissue mass in children with growth hormone deficiency, Turner's syndrome, and intrauterine growth retardation during the first year of treatment with GH. J Clin Endocrinol Metab 1994;78:904-9. 
|
| 13. | Veldhuis JD, Iranmanesh A, Ho KK, Waters MJ, Johnson ML, Lizarralde G. Dual defects in pulsatile growth hormone secretion and clearance subserve the hyposomatotropism of obesity in man. J Clin Endocrinol Metab 1991;72:51-9. 
|
| 14. | Williams T, Berelowitz M, Joffe SN, Thorner MO, Rivier J, Vale W, et al. Impaired growth hormone responses to growth hormone-releasing factor in obesity. A pituitary defect reversed with weight reduction. N Engl J Med 1984;311:1403-7. 
|
| 15. | Rasmussen MH, Hvidberg A, Juul A, Main KM, Gotfredsen A, Skakkebaek NE, et al. Massive weight loss restores 24-hour growth hormone release profiles and serum insulin-like growth factor-I levels in obese subjects. J Clin Endocrinol Metab 1995;80:1407-15. 
|
| 16. | Gravholt CH, Naeraa RW, Fisker S, Christiansen JS. Body composition and physical fitness are major determinants of the growth hormone-insulin-like growth factor axis aberrations in adult Turner's syndrome, with important modulations by treatment with 17 beta-estradiol. J Clin Endocrinol Metab 1997;82:2570-7. 
|
| 17. | Holl RW, Kunze D, Etzrodt H, Teller W, Heinze E. Turner syndrome: Final height, glucose tolerance, bone density and psychosocial status in 25 adult patients. Eur J Pediatr 1994;153:11-6. 
|
| 18. | Hanaki K, Ohzeki T, Ishitani N, Motozumi H, Matsuda-Ohtahara H, Shiraki K. Fat distribution in overweight patients with Ullrich-Turner syndrome. Am J Med Genet 1992;42:428-30. 
|
| 19. | Ohzeki T, Hayashi K, Higurashi M, Hanaki K, Ishitani N, Shiraki K. Ullrich-Turner syndrome and anorexia nervosa. Am J Med Genet 1989;32:87-9. 
|
| 20. | Ohzeki T, Hanaki K, Motozumi H, Ohtahara H, Urashima H, Shiraki K. Assessment of subcutaneous fat using ultrasonography in the Ullrich-Turner syndrome. Am J Med Genet 1993;46:450-2. 
|
[Figure 1]
[Table 1]
|






