| |


 |
| Year : 2011 | Volume
: 5
| Issue : 2 | Page : 38-43 |
|
|
|
|
|
ORIGINAL ARTICLE Percutaneous fixation with Schanz screws for displaced two- and three- part fractures of the proximal humerus in patients above fifty years of age
Abdelsalam Eid, Mohamed Osman, Hosam-Eldeen Fekry
Department of Orthopaedic Surgery, Faculty of Medicine, Zagazig University, Egypt
Correspondence Address:
Abdelsalam Eid
5 Mahfouz Street, from Ahmed Ismail Street, Zagazig, 44511
Egypt
 Source of Support: None, Conflict of Interest: None  | 11 |
DOI: 10.4103/0973-6042.83195

|
|
|
|
| Date of Web Publication | 26-Jul-2011 |
 Abstract Abstract | | |
Purpose: The aim of this study is to evaluate whether two 3.0 mm Schanz screws in two-part proximal humeral fractures (plus one additional Schanz screw or K wire in three-part fractures) can provide enough stability to allow early mobilization until healing occurs in elderly patients.
Settings and Design: This prospective study was performed in the Orthopaedic Department of our University Hospital.
Patients and Methods: We performed closed reduction and percutaneous pinning for thirty-three patients with proximal humerus fractures. Twenty-seven patients were available for the final follow-up. Of those 27 patients, 17 had two-part surgical neck fractures; while 10 had three-part fractures. For fixation, we used two 3.0 mm Schanz screws in patients with two-part fractures plus one additional Schanz screw or K wire in the 10 patients with three-part fractures.
Results: The mean Constant score modified according to the age and sex was 89.8% (range: 77.3-97.2%). Fifteen patients had excellent results, 11 patients had good results, and one patient had a fair result.
Conclusion: Closed reduction and percutaneous pinning with two Schanz screws for two-part surgical neck humeral fractures, plus an additional Schanz screw or K wire for three-part proximal humeral fractures is a useful and effective technique that provides enough stability to allow an early rehabilitation program till union occurs in elderly patients.
Level of Evidence: IV; therapeutic study, case series.
Keywords: Early rehabilitation, proximal humerus fracture, Schanz screws
How to cite this article:
Eid A, Osman M, Fekry HE. Percutaneous fixation with Schanz screws for displaced two- and three- part fractures of the proximal humerus in patients above fifty years of age. Int J Shoulder Surg 2011;5:38-43 |
How to cite this URL:
Eid A, Osman M, Fekry HE. Percutaneous fixation with Schanz screws for displaced two- and three- part fractures of the proximal humerus in patients above fifty years of age. Int J Shoulder Surg [serial online] 2011 [cited 2016 Apr 25];5:38-43. Available from: http://www.internationalshoulderjournal.org/text.asp?2011/5/2/38/83195 |
 Introduction Introduction | |  |
Proximal humeral fractures are the third most common fracture in elderly patients. [1] They represent over 70% of humeral fractures occurring over the age of 40. [2] According to the widely accepted Neer [3] classification, most are undisplaced and can be managed conservatively, usually with satisfactory results. [1,2] However, there is considerable controversy concerning the treatment of displaced proximal humeral fractures. Numerous open and closed techniques as well as a variety of fixation methods were reported, with each claiming good results. [1],[2],[4],[5],[6] A percutaneous method of fixation allows for minimal soft tissue dissection thereby protecting the blood supply to the fracture fragments which promotes rapid healing and minimizes the chances of avascular necrosis. This is even more important in the elderly population as it allows a rapid return of function and independence. Numerous reports describe percutaneous techniques of fixation of the proximal humerus fractures. [7],[8],[9],[10],[11],[12],[13] Percutaneous fixation is believed to be best suited for two-part and some three-part fractures. [5],[11] The aim of this study is to evaluate whether two 3.0 mm Schanz screws for two-part proximal humeral fractures (plus one additional Schanz screw or K wire for three-part fractures) can provide enough stability to allow early mobilization until healing occurs in patients above 50 years of age. The study was approved by the Institutional Ethical Committee.
 Patients and Methods Patients and Methods | |  |
This prospective study was conducted between January 2005 and December 2008 in the casualty unit of the Orthopaedic Department of our University Hospital. All patients gave an informed consent before their data were included in the study. Thirty-three patients with proximal humerus fractures were managed by closed reduction and percutaneous pinning. Twenty-seven patients were available for the final follow-up. Only those 27 patients will be discussed hereafter. According to the Neer [3] classification of proximal humeral fractures, 17 patients had two-part surgical neck fractures; while 10 patients had three-part fractures, where the fracture involved the surgical neck as well as the greater tuberosity which will be hereafter referred to as "three-part fracture". Inclusion criteria were: age over 50 years; and displaced two-part or three-part proximal humeral fractures. Exclusion criteria were: the presence of a four-part fracture, a fracture-dislocation or a head splitting fracture, uncontrolled diabetes, and poor general and mental condition. There were 19 injuries involving the right shoulder and eight injuries involving the left shoulder. The age of the patients ranged from 51 to77 years (mean 60.9 years). Sixteen patients were females. The interval between the injury and the surgical intervention ranged from 12 hours to seven days (mean 2 days). The fixation was performed using two Schanz screws in all patients with two-part fractures. One additional Schanz screw or K wire was used in the 10 patients with three-part fractures. All patients were injured as a result of a low energy fall on the outstretched hand. All patients were examined clinically to check for other associated injuries as well as associated medical comorbidities. Two patients had ipsilateral fractures of forearm bones which were concomitantly managed as required. X-rays in the anteroposterior and axillary views were obtained. In all patients, computerised tomography (CT)'s were obtained to confirm the number of fragments, detect secondary fracture lines that may interfere with the expected site of Schanz screw placement, and rule out dislocation or head split.
Surgical technique
A prophylactic third generation cephalosporin was administered just before induction of anesthesia. Twenty-two patients were given general anesthesia, whereas five patients were given regional anesthetic block. The patient was placed in the supine position with the affected shoulder hanging outside the table for clear visualization by the image intensifier. The entire upper limb to the root of the neck and the midline of the chest anteriorly and posteriorly was prepped and draped. The fracture was reduced under the image intensifier by gentle manual traction with counter traction provided by a towel placed like a sling in the axilla and held by an assistant. Abduction/adduction and external/internal rotation of the arm helped adjust the reduction. Medial displacement of the shaft, when present, was corrected by the surgeon's hand in the axilla pushing the shaft laterally. When the fracture was impacted and reduction was difficult, a 3.0 mm K wire was inserted manually from distal to proximal along the anterior cortex of the humerus to disimpact the head fragment and help the reduction. A stab incision was placed in the skin approximately 10 cm distal to the edge of the acromion, and the soft tissues were split with a hemostat to the lateral cortex of the humerus. The first 3.0 mm Schanz screw was mounted on a power drill and inserted through the skin so as to penetrate the lateral humeral cortex at or in front of its midline approximately 8 cm from the edge of the acromion. To avoid slippage, the Schanz screw was initially introduced nearly perpendicular to the lateral humeral cortex, then it was gradually inclined until it reached the angle required to engage the inferior part of the humeral head. Then the Schanz screw was advanced at a low speed until the Schanz screw was well seated in the subchondral bone of the inferior part of the humeral head. Anteroposterior and axillary views were obtained by the image intensifier throughout this manoeuvre to ascertain the Schanz screw's placement within the head without penetration of the articular surface in both views. The second Schanz screw was placed in the same manner 0.5 - 1 cm proximally. Range of motion was then carried out under fluoroscopy to ensure the stability of the fixation. In the 10 patients with a three-part fracture involving the greater tuberosity, an additional Schanz screw (six patients) or a 2.0 mm K wire (four patients) were advanced from the tip of the greater tuberosity inferiorly and medially to engage the medial cortex of the shaft. The K wire was used when the tuberosity was judged to be too thin and fragmented and the surgeon feared that a Schanz screw might fragment it even more. Under image intensification, the reduction was finally evaluated and graded as anatomical, acceptable, or unacceptable. The criteria for an acceptable reduction were: less than 5.0 mm displacement and less than 20° angulation. This evaluation was primarily the judgment of the operating surgeon. The quality of reduction was later confirmed in the postoperative control X-ray. The reduction was found to be anatomical in 14 patients with two-part fractures, and five patients with three-part fractures. The reduction was considered acceptable in the remaining patients. The Schanz screws ± K wire were left protruding from the skin to facilitate later removal in the outpatient clinic.
The mean duration of the surgical procedure was 25 min (range: 13-50 min). Its improvement was directly related to the rise of the learning curve.
Postoperative care
The arm was placed in a pouch arm-sling. Postoperative X-rays were obtained for documentation purposes. The patient was instructed on the care of the Schanz screws ± K wire and discharged on the second postoperative day. Prophylactic intravenous antibiotics were continued for three days. The patient came for clinical follow-up every week during the initial four weeks, then at six and eight weeks postoperatively, while control X-rays were obtained at four and six weeks postoperatively. If no radiological union had been detected at six weeks, another X-ray was obtained at eight weeks to check for radiological union. Exercises for the elbow, wrist, and hand were started as soon as pain allowed. Gentle pendulum exercises were started one week postoperatively, and then gradually increased over the following weeks. The patient continued to wear the pouch arm sling, while not exercising till the end of the third week where it was discarded. Assisted active exercises were started four weeks postoperatively. The Schanz screws ± K wire were removed in the outpatient clinic six weeks postoperatively and active exercises and muscle strengthening were encouraged. Range of motion continued to improve over the six months following the procedure.
Follow-up
The patients came for clinical follow-up at three months, clinical and radiological follow-up at six months, one year, and then yearly thereafter. The mean follow-up was 18 months (range: 12-36 months).
 Results Results | |  |
All fractures united. Clinical union, as evidenced by the disappearance of pain and the progress of active movement and usage of the arm occurred at an average of five weeks (range: four to six weeks). On the other hand, radiological union was judged by callus formation, progressive obliteration of the fracture line, and maintenance of the reduction. Radiological union was evident at an average of seven weeks (range: six to eight weeks). The patients were evaluated clinically using the Constant Shoulder Score. [14] The mean absolute Constant score for the entire series was 69.5 (range: 56-87). This corresponded to a mean of 89.9% (range: 77.3-97.3%) of the Constant score modified according to the age and sex [Table 1]. [14]
According to the Constant score modified according to the age and sex, 15 patients had excellent results, 11 patients had good results, and one patient had a fair result (excellent = ≥ 90, good = 80 - 89, fair = 70-79, poor ≤ 69).
The pain was evaluated by the method of Constant using a Visual Analogue Scale (VAS) where 0 = severe pain and 15 = no pain. The mean pain VAS score was 13.2 (range: 10-15).
In the two-part group, the range of abduction exceeded 150° in one patient, was up to 150° in seven patients, and was over 90° in nine patients. As regards to internal rotation, two patients could reach the interscapular region, four could reach T12 vertebra, 10 could reach their waist region, and one could reach only to the sacro-iliac joint. For the 17 patients with two-part fractures, the mean absolute Constant score was 71.9 (range: 59-87) which corresponded to a mean of 92.5% (range: 84.3-97.3%) of the Constant score modified according to age and sex. Fifteen patients were very satisfied or satisfied with the outcome [Figure 1].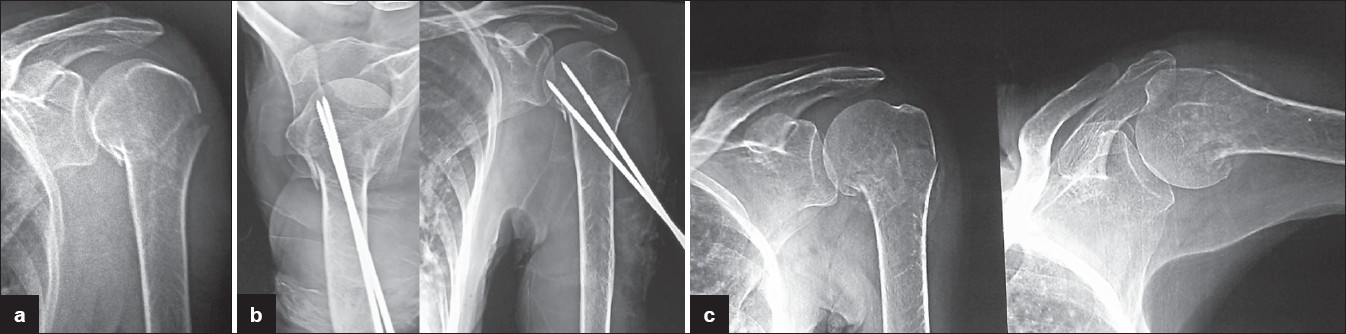 | Figure 1: A 61-year-old female presented with two-part fracture showing a final good result. (a) Preoperative X-ray showing two-part fracture with varus angulation (b) Postoperative X-ray showing correction of angulation and fixation by two Schanz screws (c) After removal of Schanz screws
Click here to view |
In the three-part group, the range of abduction was up to 150° in three patients, over 90° in six patients, and up to 90° in one patient. As regards to internal rotation, four patients could reach T12 vertebra, and six could reach their waist region. The mean absolute Constant score for the 10 patients with three-part fractures was 65.5 (range: 56-79) which corresponded to a mean of 85.5% (range: 77.3-97.3%) of the Constant score modified according to the age and sex. Seven patients were very satisfied or satisfied with the outcome [Figure 2]. | Figure 2: A 74-year-old male presented with three-part fracture showing A final excellent result (a) Preoperative X-ray showing three-part valgus impacted fracture with fragmented greater tuberosity (b) Postoperative X-ray showing disimpaction of the head, correction of the valgus orientation of the head, and reduction of the greater tuberosity beneath the head (c) After removal of Schanz screws (d) Range of shoulder motion
Click here to view |
Complications
The most common complication was pin tract infection. It occurred in thirteen cases. However, it was generally mild and limited to minimal discharge around the pin that did not affect the quality of fixation or disturb the reduction. Swabs were taken and antibiotics given according to culture and sensitivity. No premature removal of pins was necessary and complete resolution of the infection occurred following removal of the pins in all cases after union had occurred. There was no injury to the axillary nerve in any of the patients as all had good active function of the deltoid muscle. No other nerves or vessels were injured in any of the cases. Minor redisplacements occurred in five cases within the first two weeks, though still within the limits of an acceptable reduction. However, they did not progress further, the fixation was holding well and the signs of union were progressing. Therefore, no revision was considered necessary. There was no pin migration. No radiological signs of avascular necrosis of the humeral head or glenohumeral osteoarthritis were noted in any of the cases during the period of follow-up.
 Discussion Discussion | |  |
Fractures of the proximal humerus are common in the elderly population. Historically, proximal humeral fractures used to be predominantly treated conservatively.
Court-Brown et al. [15] reported that the results of conservative treatment of translated two-part fractures were comparable to surgical treatment (flexible intramedullary nailing + tension band wiring) in their series. However, they stated the outcome was related to the age of the patient and the degree of translation.
Zyto [16] presented the ten year results of 14 shoulders with proximal humeral fractures treated conservatively (nine were three-part and five were four-part fractures). In the three-part group, the mean Constant score was 59, and the mean abduction was 100°.
Operative intervention aims at as near to anatomic reduction as possible as well as stable fixation to relieve pain and allow early mobilization thereby avoiding stiffness. However, owing to its wide range of motion, the shoulder joint can tolerate minor malreductions, making early mobilization to avoid stiffness, the most important goal.
Hintermann et al. [17] treated 38 elderly patients with proximal humeral fractures utilizing a blade plate to obtain rigid fixation. Their series consisted of three- and four-part fractures. The three-part group had a median Constant score of 75.
A percutaneous method of fixation is quite desirable in the present era of minimally invasive surgery as it allows for minimal soft tissue dissection thereby protecting the blood supply to the fracture fragments which promotes rapid healing and minimizes the chances of avascular necrosis. A study comparing a group of patients treated with percutaneous pinning to another group of patients treated with open reduction and internal fixation ORIF noted that the incidence of osteonecrosis was higher after ORIF, potentially, secondary to surgical trauma. [18] In addition, when the soft tissue sleeve is minimally disturbed, it acts as a fluid compartment creating a hydraulic effect that helps in maintaining the reduction of fragments, minimizing the need for extensive metallic hardware.
A further advantage of the percutaneous fixation is minimizing operative time, which minimizes anesthesia time in those elderly patients who are often medically compromised. In this series, the mean duration of the surgical procedure was 25 min (range: 13-50 min), which meant less exposure to anesthesia and less burden on the patients' health.
Closed reduction and percutaneous pinning was popularized by Jaberg et al. in 1992. [7] Since that time, it has been reported by many other authors. [8],[9],[10],[11],[12],[13] Nevertheless, many authors still describe it as a controversial, demanding, and difficult to learn technique. [4],[5],[11]
Given the close proximity of important neurovascular structures to the fracture region, it is conceivable that the use of more pins might lead to a greater chance of injuring one of those important structures. Therefore, it is safer to limit the use of percutaneous pins to the minimum that can hold the reduction securely enough to allow early mobilization and avoid stiffness. This is the rationale behind the use of only two Schanz screws for fixation of the head fragment in this series.
The Schanz screws, as used in this series, provide better purchase and better stability than smooth K wires used by some authors. [8],[11] They can also provide better purchase than threaded K wires used by some other authors [8],[10] owing to their wider and longer threads. Thus, there is less chance for loosening, migration, or loss of fixation.
However, in this series, in four cases of three-part fractures, a K wire was used to fix the greater tuberosity rather than additional Schanz screws. The reason for this was that the greater tuberosity was thinned and fragmented in these cases, and the smooth smaller K wire was expected not to produce further fragmentation.
Fenichel et al. [10] presented the results of closed reduction and percutaneous pinning of two- and three-part fractures in 50 patients with a mean follow-up of 2.5 years. They used three to five threaded K wires of 3.0 mm diameter. Post-operatively, they immobilized the shoulder in a shoulder immobilizer for a period of six weeks. In their series, 70% of patients obtained excellent or good results. However, seven of their patients had a severe loss of reduction, and three of the seven needed revision surgery.
Calvo et al. [11] reported the outcomes of closed reduction and percutaneous pinning of proximal humeral fractures in 50 patients after a mean follow-up of 13.6 months. Their group of patients included two, three, and four-part fractures. For fixation, they utilized a minimum of three smooth K wires. Postoperatively, the arm was immobilized in a sling for four weeks. The most common complication they reported was migration of at least one Kirschner wire, which occurred in 18 cases (36%). Pin migration resulted in loss of reduction of the fracture in five patients (10%) and two patients required revision surgery.
In this series, we minimized the number of pins used for fixation to minimize the chance of injuring important neurovascular structures e.g. axillary nerve, and also minimized the postoperative immobilization in order to avoid shoulder stiffness. Our hyposthesis was that two 3.0 mm Schanz screws for two-part proximal humeral fractures (plus one additional Schanz screw or K wire for three-part fractures) can provide enough stability to allow early mobilization until healing occurs in patients above 50 years of age. Our results support this hypothesis.
Our mean follow-up was 18 months. Fifteen patients (55%) had excellent results, 11 patients (41%) had good results, and one patient (4%) had a fair result. In the two-part group, the mean Constant score modified according to age and sex for the 17 patients with two part fractures was 92.4% (range: 84.2-97.2%). Fifteen patients were very satisfied or satisfied with the outcome. The mean score for the 10 patients with three-part fractures was 85.5% (range: 77.3-97.2%). Seven patients were very satisfied or satisfied with the outcome. Minor redisplacements occurred in five cases within the first two weeks, however, no revision was considered necessary as the still fell within the criteria of an acceptable reduction.
Careful patient selection is one of the most important factors for a satisfactory outcome of this technique. This series included low-energy injuries with an intact soft-tissue sleeve. The patients were compliant, cooperative, and participated willingly in the strictly surgeon-supervised weekly follow-up and rehabilitation program.
The results of this series are comparable to those of other authors keeping in consideration that a smaller number of pins were used for fixation, and the rehabilitation program progressed at a faster pace.
The key element of success in this series is perhaps the early rehabilitation program, which allowed a rapid return of function as compared to longer periods of immobilization in other series.
One of the weaknesses of this study is the rather short follow-up period. A longer follow-up may be required to detect late onset of avascular necrosis or osteoarthritis.
 Conclusion Conclusion | |  |
Closed reduction and percutaneous pinning with two Schanz screws for two-part proximal humeral fractures, with an additional Schanz screw or a smooth K wire for three-part proximal humeral fractures is a useful technique that minimizes operative time, and reduces the risk of neurovascular injury, while providing enough stability to allow an early rehabilitation program till union occurs in elderly patients.
 References References | |  |
| 1. | Helmy N, Hintermann B. New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res 2006;442:100-8. 
|
| 2. | Burton DJ, Watters AT. Management of proximal humeral fractures. Curr Orthop 2006;20:222-33. 
|
| 3. | Neer CS 2 nd . Displaced proximal humeral fractures. Part I: Classification and evaluation. J Bone Joint Surg Am 1970;52:1077-89. 
|
| 4. | Nho SJ, Brophy RH, Barker JU, Cornell CN, MacGillivray JD. Management of proximal humeral fractures based on current literature. J Bone Joint Surg Am 2007;89(Suppl 3):44-58. 
|
| 5. | Vallier HA. Treatment of proximal humerus fractures. J Orthop Trauma 2007;21:469-76. 
|
| 6. | Lanting B, MacDermid J, Drosdowech D, Faber KJ. Proximal humeral fractures: A systematic review of treatment modalities. J Shoulder Elbow Surg 2008;17:42-54. 
|
| 7. | Jaberg H, Warner JJ, Jakob RP. Percutaneous stabilization of unstable fractures of the humerus. J Bone Joint Surg Am 1992;74:508-15. 
|
| 8. | Resch H, Povacz P, Fröhlich R, Wambacher M. Percutaneous fixation of three- and four-part fractures of the proximal humerus. J Bone Joint Surg Br 1997;79:295-300. 
|
| 9. | Ferrari JD. Percutaneous pinning of proximal humerus fractures. Oper Tech Orthop 2001;11:233-42. 
|
| 10. | Fenichel I, Oran A, Burstein G, Perry Pristch M. Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus: A retrospective study. Int Orthop 2006;30:153-7. 
|
| 11. | Calvo E, de Miguel I, de la Cruz JJ, López-Martín N. Percutaneous fixation of displaced proximal humeral fractures: Indications based on the correlation between clinical and radiographic results. J Shoulder Elbow Surg 2007;16:774-81. 
|
| 12. | Kayalar M, Toros T, Bal E, Ozaksar K, Gurbuz Y, Ademoglu Y. The importance of patient selection for the treatment of proximal humerus fractures with percutaneous technique. Acta Orthop Traumatol Turc 2009;43:35-41. 
|
| 13. | Keener JD, Parsons BO, Flatow EL, Rogers K, Williams GR, Galatz LM. Outcomes after percutaneous reduction and fixation of proximal humeral fractures. J Shoulder Elbow Surg 2007;16:330-8. 
|
| 14. | Constant CR, Gerber C, Emery RJ, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg 2008;17:355-61. 
|
| 15. | Court-Brown CM, Garg A, McQueen MM. The translated two-part fracture of the proximal humerus: Epidemiology and outcome in the older patient. J Bone Joint Surg Br 2001;83:799-804. 
|
| 16. | Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury 1998;29:349-52. 
|
| 17. | Hintermann B, Trouillier HH, Schäfer D. Rigid internal fixation of the proximal humerus in older patients. J Bone Joint Surg Br 2000;82:1107-12. 
|
| 18. | Kralinger F, Irenberger A, Lechner C, Wambacher M, Golser K, Sperner G. Comparison of open versus percutaneous treatment for humeral head fracture. Unfallchirurg 2006;109:406-10. 
|
[Figure 1], [Figure 2]
[Table 1]
| This article has been cited by | | 1 |
Internal fixation versus shoulder hemiarthroplasty for displaced 4-part proximal humeral fractures in elderly patients |
|
| Cai, M. and Tao, K. and Yang, C. and Li, S. | | Orthopedics. 2012; 35(9): e1340-e1346 | | [Pubmed] | | | 2 |
Internal Fixation Versus Shoulder Hemiarthroplasty for Displaced 4-part Proximal Humeral Fractures in Elderly Patients |
|
| Ming Cai,Kun Tao,Chunxi Yang,Shaohua Li | | Orthopedics. 2012; 35(9): e1340 | | [Pubmed] | [DOI] | |
|
 |
|
