| |


 |
| Year : 2011 | Volume
: 5
| Issue : 2 | Page : 47-49 |
|
|
|
|
|
CASE REPORT An unusual complication of the Mackenzie approach for a Copeland hemiarthroplasty
Sarah E Johnson-Lynn, Jaime Candal-Couto
Department of Orthopedics, Wansbeck General Hospital, Woodhorn Lane, Ashington, Northumberland, NE63 9JJ, United Kingdom
Correspondence Address:
Sarah E Johnson-Lynn
20 Millfield Grove North Shields, Tyne and Wear
United Kingdom
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.83197

|
|
|
|
| Date of Web Publication | 26-Jul-2011 |
 Abstract Abstract | | |
We report the case of a patient with end-stage osteoarthritis who received a successful Copeland resurfacing hemiarthroplasty through a Mackenzie anterosuperior approach, which involves taking the anterior portion of the deltoid attachment from the acromion along with an osteo-periosteal sleeve. The patient went on to develop severe subacromial impingement symptoms 4 months postoperatively. X-rays revealed a large anteroinferior acromial osteophyte that had not been present preoperatively and was deemed to represent a malunited osteo-periosteal sleeve from the Mackenzie approach.
Keywords: Copeland hemiarthroplasty, Mackenzie approach, malunion, osteo-periosteal sleeve, subacromial impingement
How to cite this article:
Johnson-Lynn SE, Candal-Couto J. An unusual complication of the Mackenzie approach for a Copeland hemiarthroplasty. Int J Shoulder Surg 2011;5:47-9 |
 Introduction Introduction | |  |
We report an unusual complication of the Mackenzie approach for a Copeland hemiarthroplasty.
 Case Report Case Report | |  |
A 66-year-old woman with Sjögren syndrome presented with a 5-year history of bilateral shoulder pain that was significantly worse on the right than the left side. The pain was reported to be constant in nature but worse at night, and completely prohibited activities above shoulder height. Examination of the right shoulder revealed a globally restricted range of movement at the glenohumeral joint. X-rays demonstrated severe osteoarthritis with osteophytosis [Figure 1]. Treatment with Copeland resurfacing hemiarthroplasty [1] was performed in June 2007 through an anterosuperior (Mackenzie) approach. [2] Two No. 1 interrupted PDS (polydioxanone) sutures were used for reattachment of the anterior border of the osteo-periosteal sleeve to the acromion. The sutures were placed transosseously through the acromium on one side and through the deltoid fascia, incorporating an osteo-periosteal sleeve, on the other [Figure 2]. 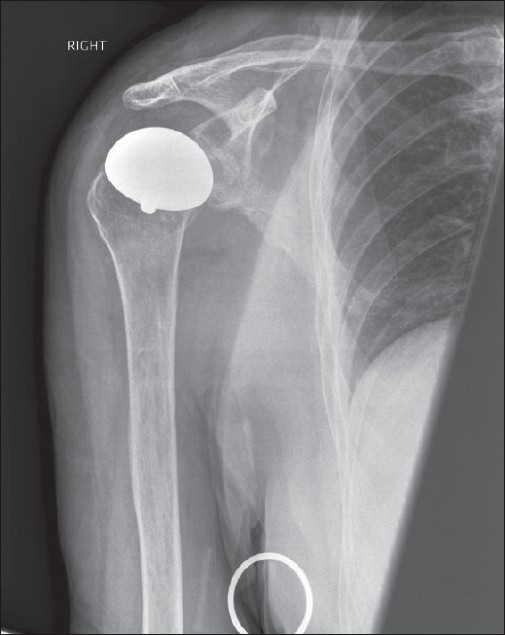 | Figure 2: Radiograph taken in the immediate postoperative period showing a Copeland resurfacing hemiarthroplasty
Click here to view |
Passive elevation past 90° could be achieved on the first postoperative day. A shoulder immobilizer was worn for 3 weeks and the patient was instructed to avoid active elevation. Good postoperative progress was made and the Copeland rehabilitation regime was followed. The patient had returned to aerobics and table tennis by the 4 th postoperative month, at which point increased pain in the shoulder was reported. At the end of the 1 st postoperative year, significant impingement symptoms were reported and X-rays demonstrated a new bony spur on the anteroinferior edge of the acromion [Figure 3]. An ultrasound scan showed a bony spur indenting the supraspinatus, but there was no accompanying cuff tear. The pain continued to worsen and diagnostic arthroscopy was performed in July 2009, which confirmed the presence of the spur at the anteroinferior edge of the acromion and excluded the presence of significant glenoid arthrosis or adhesions as contributing factors to the patient's symptoms. The spur was resected arthroscopically during this procedure. The patient's impingement symptoms have since completely resolved [Figure 4].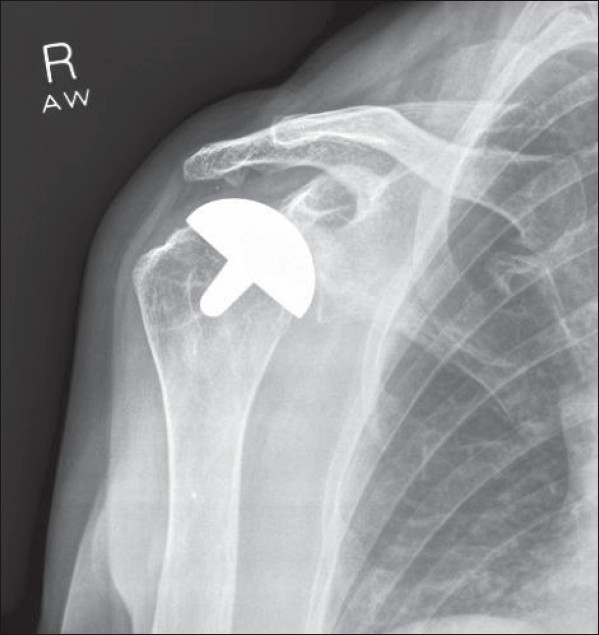 | Figure 3: Radiograph at 1 year showing new bony spur on the inferior surface of the acromion
Click here to view |
 Discussion Discussion | |  |
The Mackenzie anterosuperior approach has been popularized for several types of shoulder arthroplasties. In this approach the anterior deltoid is commonly reflected with an osteo-priosteal sleeve. [2]
We postulate that the bony spur responsible for the impingement symptoms in our patient was formed by malunion of the osteo-periosteal sleeve. At the time of arthroscopy, a sharp spur of bone of the same size and shape as the osteo-periosteal sleeve was found to be united in the correct position on the anterior acromion but, from its shape, it had apparently rotated 90° from the original orientation. The onset of symptomatic impingement along with new X-ray findings at 4 months postoperatively is consistent with rotation of the fragment during healing following the patient's return to sporting activity. Full resolution of the patient's symptoms following resection of the spur also supports this conclusion.
Intra-articular factors are the most common reasons for postoperative pain following Copeland resurfacing hemiarthroplasty and are due to the nonanatomical shape of the prosthesis, which does not accurately recreate the original shape of the humeral head. As our patient was initially pain free with good shoulder function, we carried out other investigations, including diagnostic arthroscopy, to look for other causes for her pain [3] Preoperative investigation to establish the diagnosis of subacromial impingement could include an injection of local anesthetic under aseptic technique into the subacromial space. Immediate pain relief would be convincing evidence of the existence of subacromial impingement.
To the best of our knowledge, this is the first report of formation of an acromial spur following the Mackenzie approach. Complications of the Copeland resurfacing hemiarthroplasty have been reported as infection, aseptic loosening, periprosthetic humeral fracture, and osteolysis. [4] Subacromial impingement has been reported in patients after this procedure and the symptoms have necessitated subacromial decompression, but this has not previously been reported to be associated with a malunited osteo-periosteal sleeve. [5] Nonunion (or fibrous union) has been reported by previous authors following surgical access using the Mackenzie approach but they did not report symptomatic subacromial impingement. [6]
In our patient, simple arthroscopic excision of the bony spur proved curative.
This case has altered our practice, as we have now abandoned the osteoperiosteal sleeve technique and instead opt for subperiosteal dissection of the anterior deltoid.
 Conclusion Conclusion | |  |
We conclude that the cause for the delayed, severe impingement symptoms in this patient following successful Copeland resurfacing hemiarthroplasty was malunion of the osteo-periosteal sleeve that was made as part of the Mackenzie approach. All symptoms resolved following arthroscopic resection of the spur.
 References References | |  |
| 1. | Copeland SA, Levy O, Brownlow HC. Resurfacing arthroplasty of the shoulder. Tech Shoulder Elbow Surg 2003;4:199-210. 
|
| 2. | Kuz JE, Pierce TD, Braunohler WM. Coronal transacromial osteotomy surgical approach for shoulder arthroplasty. Orthopedics 1998;21:155-62. 
|
| 3. | Tytherleigh-Strong GM, Levy O, Sforza G, Copeland SA. The role of arthroscopy for the problem shoulder arthroplasty. J Shoulder Elbow Surg 2002;11:230-4. 
|
| 4. | Levy O, Copeland SA. Cementless surface replacement arthroplasty of the shoulder. 5- to 10-year results with the Copeland mark-2 prosthesis. J Bone Joint Surg Br 2001;83:213-21. 
|
| 5. | Thomas SR, Wilson AJ, Chambler A, Harding I, Thomas M. Outcome of Copeland surface replacement shoulder arthroplasty. J Shoulder Elbow Surg 2005;14:485-91. 
|
| 6. | Webb M, Funk L. An anterosuperior approach for proximal humeral fractures. Tech Shoulder Elbow Surg 2006;7:77-81. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|
