| |


 |
| Year : 2011 | Volume
: 5
| Issue : 3 | Page : 61-67 |
|
|
|
|
|
ORIGINAL ARTICLE Open reduction and internal fixation of clavicular nonunions with allograft bone substitute
Michael D Riggenbach, Grant L Jones, Julie Y Bishop
Department of Orthopaedics, The Ohio State University, Columbus, OH, USA
Correspondence Address:
Julie Y Bishop
Department of Orthopaedics, The Ohio State University, 2050 Kenny Rd, Suite 3300, Columbus, OH 43221
USA
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.86232

|
|
|
|
| Date of Web Publication | 17-Oct-2011 |
 Abstract Abstract | | |
Background: Biologic augmentation with allograft has shown equivalent healing rates to autograft in several nonunion models. No literature exists clearly demonstrating this in the clavicle. The purpose of this study was to evaluate the healing and complication rates of clavicle nonunions treated solely with open reduction and internal fixation (ORIF) and allograft.
Materials and Methods: Nineteen clavicle nonunions treated with ORIF and allograft were evaluated retrospectively to assess healing rates and complications based on clinical symptoms and radiographic findings.
Results: For the 19 patients included and treated with ORIF and allograft, clinical follow-up averaged 15 months. Seven patients were smokers. Although complete radiographic healing was achieved in only 68% of patients, clinical success occurred in 16 (84%) patients who demonstrated full range of motion and strength without pain. The three patients who did not demonstrate full radiographic healing were completely pain free. Five patients experienced complications (26%). Two underwent hardware removal due to persistent irritation after union. Three had a persistent painful nonunion. Each of these three patients was a smoker (P=0.08). Two proceeded to union after revision fixation. The other had hardware failure, which was removed, with a persistent nonunion and did not wish any further treatment.
Conclusion: ORIF with allograft bone substitute is an acceptable treatment alternative to iliac crest bone graft for clavicle nonunions. However, we did not demonstrate equivalent healing rates to published results utilizing autograft. Smokers were identified to have a trend toward higher failure rates with ORIF augmented with allograft and therefore these patients may be better served by augmenting fixation with autograft.
Level of Evidence: IV; retrospective comparative study.
Keywords: Allograft bone substitute, clavicle nonunion, iliac crest bone graft, open reduction and internal fixation
How to cite this article:
Riggenbach MD, Jones GL, Bishop JY. Open reduction and internal fixation of clavicular nonunions with allograft bone substitute. Int J Shoulder Surg 2011;5:61-7 |
 Introduction Introduction | |  |
Clavicle fractures account for up to 10% of all fractures and are typically sustained by young, active males. [1],[2],[3] Most nondisplaced, minimally comminuted shaft fractures are treated nonoperatively and heal without complication. Most stable lateral clavicle fractures heal without event as well, although unstable distal clavicle fractures have a higher nonunion rate of up to 30%. [4] Overall, the nonunion rate after nonoperative treatment of clavicle fractures is rare, reportedly ranging from less than 1 to 4.5%. [5],[6] However, female gender, age, fracture displacement, fracture stability, and comminution have been shown to increase this nonunion risk in some studies to between 33 and 47%. [5],[7] Patients may present with mechanical symptoms, intractable pain, motion restriction, and even thoracic outlet syndrome. [8],[9] These persistent symptoms may limit functional capacity and often necessitate surgical intervention.
Open reduction and internal fixation (ORIF) with autologous iliac crest bone graft (ICBG) has been the gold standard to address clavicular shaft nonunions. A review of the literature demonstrates healing rates ranging from 89 to 100%. [1],[2],[3],[4],[8],[10],[11] Although ICBG is very effective for fracture healing, complications from graft harvest can potentially cause significant morbidity. Major complications such as pelvic fracture, infection, prolonged pain, and minor complications such as persistent drainage, sensory disturbances, and temporary pain range from 0.7 to 25% and 9.4 to 24%, respectively. [12],[13],[14],[15],[16],[17],[18],[19] Hip pain has been shown to persist as long as six months postoperatively in 37.9% of patients. [13],[14] Even with meticulous technique, the potential for graft-site complications and their associated morbidity remains and continues to be a substantial concern for the treating surgeon.
In an effort to minimize graft-site complications, alternative methods to augment healing have emerged. ORIF with demineralized bone matrix (DBM) rather than ICBG has shown equal efficacy in treating nonunions of the humerus and tibia, [18],[19] and variable enhancement of fusion rates in the spine without the associated morbidity of graft harvest. [20] However, the literature incorporating graft alternatives in clavicle nonunions is sparse. Endrizzi et al. performed a retrospective analysis of superior plate fixation in the treatment of clavicular nonunions citing a 93% healing rate. [21] However, only 29.8% of these patients were treated with DBM and the other 63.8% were treated with local autogenous graft-thus, the study was not just evaluating the use of allograft alternatives. In addition, they did not differentiate healing rates in those with DBM vs those with autogenous graft. Thus, no series exists demonstrating the efficacy of ORIF with allograft bone substitute alone when treating clavicular nonunion. The purpose of this investigation was to evaluate the clinical outcomes, radiographic healing, and complication rate of clavicle nonunions treated with ORIF and allograft bone substitute.
 Materials and Methods Materials and Methods | |  |
Institutional Review Board Approval was obtained prior to investigation.
The records of two shoulder surgeons at a tertiary referral center over the previous five years (2004-2009) were retrospectively reviewed to identify all clavicle nonunions requiring operative intervention. Inclusion criteria consisted of any patient between the ages of 18 to 89 years with a symptomatic clavicular nonunion. A nonunion diagnosis was based on radiographic [Figure 1] and [Figure 2] as well as clinical exam findings consistent with a symptomatic nonunion (continued pain, mechanical symptoms, tenderness, and/or crepitus on exam). These patients presented for operative fixation due to their persistent symptoms and failure of conservative management. Based on these criteria, 24 patients with a clavicular nonunion were identified. Five patients were excluded, two due to segmental defects requiring iliac crest corticocancellous graft, one due to incarceration, one due to suture fixation of a distal clavicle fracture, and one due to death unrelated to the surgery, two months postoperatively, preventing postoperative evaluation.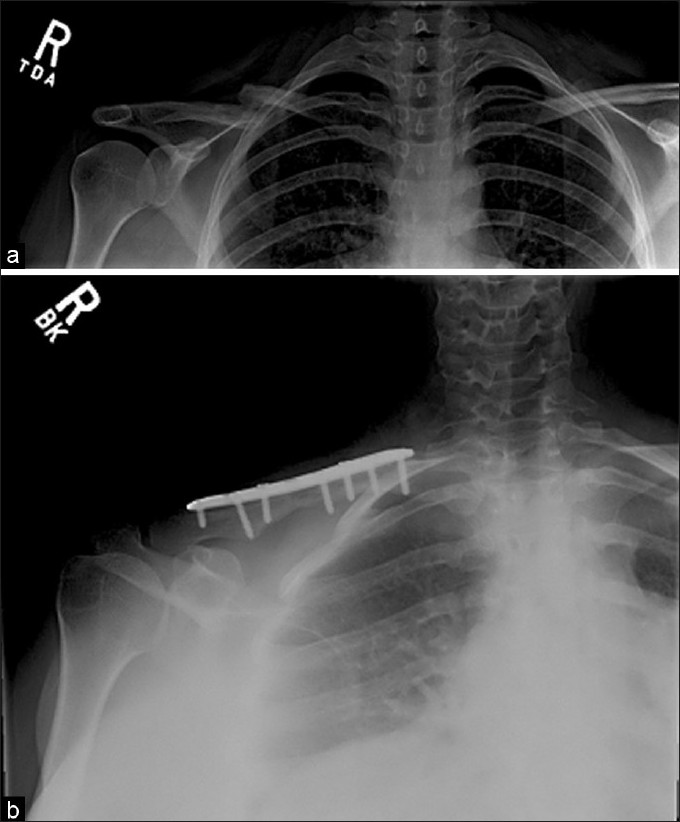 | Figure 1: Clavicle nonunion (a). Union demonstrated after fixation (b); patient had radiographic and clinical evidence of union after fixation
Click here to view |
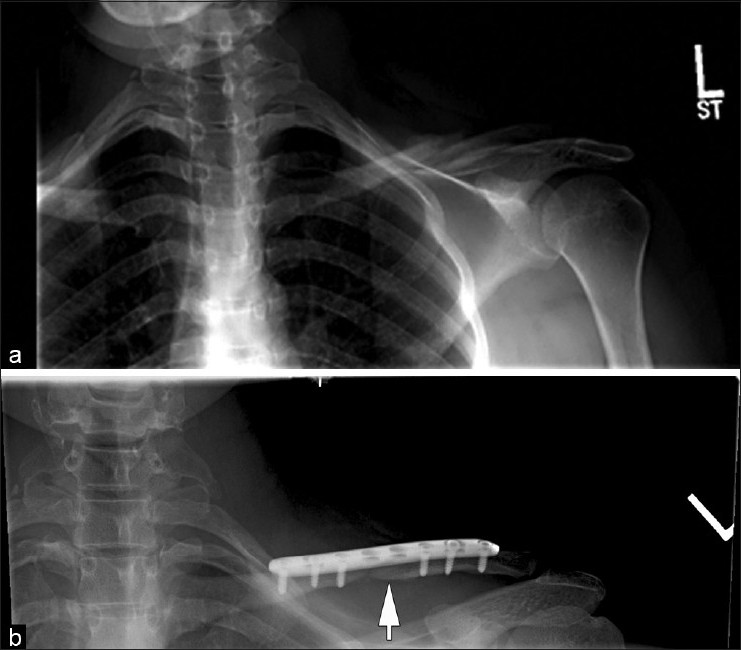 | Figure 2: Clavicle nonunion (a). No radiographic evidence of complete union (b) despite full strength, range of motion and no pain on clinical exam. Fracture line still visible eight months postoperatively (arrow)
Click here to view |
We recorded information about the subject's age, clavicular nonunion location, type, duration, range of motion, strength, tobacco use, length of postoperative follow-up, clinical and radiographic evidence of healing, and any complications.
Surgical technique
Patients were given a preoperative interscalene block and administered general anesthesia. They were placed supine on the operating table with a scapular bump. An oblique incision was made in line with the clavicle over the nonunion site. The nonunion site was identified, debrided of fibrous tissue and/or attempted callus to expose bleeding bone edges. The debrided nonunion site was then reduced and fixed on the superior surface of the clavicle with a precontoured locking clavicle plate. All plate fixation constructs achieved a minimum of three screws medial and lateral to the nonunion site. One of the following healing adjuncts was placed at the nonunion site: 12 received platelet-rich plasma (PRP) with DBM and the other seven received allograft corticocancellous chips. In one case, the allograft chip was supplemented with rhBMP-2, and in a second case, another with calcium phosphate cement. The deltotrapezial fascia, subdermal and dermal layers were closed in succession. The deltotrapezial fascia, subdermal and dermal layers were closed in succession.
Postoperative care
Patients were discharged home the same day of surgery with a sling for the first six weeks. Patients then progressed to active shoulder range of motion over the next six weeks as their symptoms allowed. At each postoperative visit, the investigators examined patients for tenderness to palpation over the nonunion site, active and passive range of motion, and strength at the shoulder. Radiographs were taken at the six-week and three-, six-, and 12-month visits and evaluated for bridging callus in two views. Strengthening was allowed when the patients had no clinical signs of pain. Patients were allowed to return to full activity when they had radiographic evidence of healing, no clinical tenderness, and return of full pain-free strength, comparable with the contralateral side.
 Results Results | |  |
The 19 patients included in this study were treated with ORIF and allograft bone substitute. Patients averaged 41.1 years in age (range, 18-57 years). A mean of 19 months elapsed between initial injury and presentation (range, 2.5-120 months). Seven patients (37%) were smokers. Eleven patients (58%) had an atrophic nonunion on preoperative X-rays. Five had a hypertrophic nonunion, and the remaining three had an oligotrophic nonunion. Eighteen patients demonstrated midshaft nonunion and one had a medial shaft nonunion. All 19 patients underwent plate fixation. Average follow-up was 15 months (range, 2.5-48 months). Patient 11 was only followed up for 2.5 months after their surgery due to clinical and radiographic evidence of healing and demonstration of full function at that time. Overall, initial radiographic evidence of healing was obtained in 13/19 (68%) patients [Figure 1]b. One patient could not afford final radiographs but had eight months of clinical follow-up and is clinically healed. Two patients without radiographic evidence of healing exhibited clinical signs of union by examination [Figure 2]b. They did not have any hardware complications, had no further interventions, and returned to full function. The other three patients are discussed below in the complication section. A total of 16 patients exhibited clinical signs of healing (84%). These patients had no pain, achieved full strength in resisted forward elevation and external rotation, and achieved range of motion equal to the contralateral side and were satisfied with their result.
Complications
There were five total complications (26%). Two were minor (hardware removal due to persistent irritation). Three major complications occurred. One of these occurred in a patient with hypertrophic nonunions, while the other two were in patients with atrophic nonunions. Three patients had failures requiring revision fixation, and two of these were catastrophic failures. Patient 19 had the plate catastrophically fail, requiring revision fixation with ICBG. He subsequently developed a hematoma requiring irrigation and debridement. This patient eventually healed without any further complications. Patient 15 had a persistent nonunion with painful instability at the nonunion site. He underwent revision fixation with DBM, which healed without any further issues. Patient 10 had four total surgeries, including revision ORIF after the initial plate fixation pulled out. He then underwent two subsequent irrigation and debridement procedures for persistent hematoma and then removal of hardware after a stress fracture developed medial to his plate. This patient's nonunion persisted, and he did not wish any further attempts at fixation. Overall, 2 of the 3 persistent nonunions did go on to eventual union, bringing the final radiographic union rate up to 80% and final clinical healing rate up to 95%. Each of the three patients with a persistent nonunion were smokers (average 0.8 pks/day) and continued to smoke during treatment despite advice to the contrary. This rate of persistent nonunion in smokers approached statistical significance (P=0.08) compared with those who went on to clinical union. The two patients with clinical evidence of healing, but not radiographic evidence of healing, were not smokers. There was no difference in complication rate in those with allograft corticocancellous chips vs those with PRP and DBM. [Table 1] lists data regarding each patient and his/her respective outcome.
 Discussion Discussion | |  |
Despite the success of ORIF with ICBG in treating clavicular nonunions, extensive literature exist exploring alternative fixation constructs and biologic adjuncts in an attempt to minimize potential graft-site morbidity. In their study evaluating external fixation of clavicle fractures and nonunions, Schiund et al. healed all five nonunions treated with a Hoffmann external fixator with no re-fractures. [22] Boehme et al. achieved 95% healing rates with Hagie pin fixation, corticoperiosteal first rib, and ICBG. [23] They cited incisional cosmesis with Langer's lines, load sharing with intramedullary fixation, and ease of hardware removal as benefits to intramedullary fixation. However, unlike a plate and screw construct, the pin does not provide rotational control. This led the authors to restrict forward elevation above 90 degrees in the early stages of rehabilitation. There was a significant rate of hardware irritation as pin removal occurred in 17 patients (81%) due to a painful bursa forming at the lateral end of the clavicle; two pins broke during removal. Despite this, they reported no graft-site complications, although most surgeons do not have a comfort level with obtaining corticoperiosteal first rib grafts. However, the complication rate with the use of the Hagie pin has ranged 25.8 to 50% and to some degree, has limited their overall use. [24],[25] Fifty-three to 66% of these complications are from skin irritation or persistent pain; yet, the nonunion rate when using this construct in the acute setting is only 8.6%. [24],[25]
In examining graft choices, ICBG remains the gold standard, and the morbidity associated with obtaining it has been well studied. Complication rates for harvesting ICBG vary significantly in the literature, based on procedure, graft site, and designation of major and minor complications. Ahlmann et al. reported major complications (hernia, pain >6 months) to be 8% and 2% for anterior and posterior ICBG, respectively. [17] The minor complication rate (superficial hematomas, temporary pain/sensory disturbances) was 15% and 0% for anterior and posterior grafting, respectively. [17] Similarly, Younger and Chapman reported major and minor complication rates of 5.3 and 25%, respectively, for anterior ICBG sites and 11.3 and 18.4%, respectively, for posterior grafting sites. [26] Subsequently, Ahlmann et al. recommended posterior grafting whenever possible. [17] However, when positioning a patient for fixation of a clavicle nonunion, this step would add significant time and complexity to the operation.
Because of this complication rate, alternative graft sources are becoming more frequently studied to determine if healing rates are acceptable given the decreased morbidity. Tashjian and Horwitz infused tricalcium phosphate with iliac crest aspirate during open reduction and plate fixation in ten clavicle nonunions and reported a 90% healing rate with no graft-site complications. [27] Their only failure was due to a postoperative wound infection and subsequent persistent nonunion. Vascularized corticoperiosteal bone grafts from the medial femoral condyle and vascularized fibula strut grafts demonstrate excellent healing capabilities, with 100% healing rates. [28],[29] The authors caution that these vascularized grafts should be used for refractory nonunions or in adverse healing environments such as an irradiated tissue bed. Therefore, they are an unlikely source of graft for the first-time treatment of a clavicle nonunion.
Like the vascularized bone grafts, DBM has shown success with bone healing in other clinical trials. DBM is created from allograft bone demineralized with acid extraction, leaving collagen and non-collagenous proteins, including growth factors. The osteoinductive potential of the graft is influenced by a number of factors: The sterilization process, the carrier, the total amount and ratios of bone morphogenetic protein (BMP) present. [30],[31],[32] Hierholzer et al. compared DBM with ICBG in their series of humeral nonunions treated with plate fixation. [19] Augmentation with DBM yielded a 97% healing rate with no donor site morbidity, while 44% of patients augmented with autologous ICBG had donor-site morbidity. [19] Similarly, Gardner et al. healed 30/31 (97%) distal femoral nonunions in which 30% were treated with DBM. [33] In a multicenter randomized controlled trial of tibial nonunions treated with intramedullary (IM) nailing and either autologous ICBG or OP-1 (BMP-7) implanted in a bovine collagen carrier (DBM), DBM demonstrated statistically equivalent clinical and radiographic healing rates at nine months and two years (81% vs 85%). [18]
When treating 47 clavicular nonunions, Endrizzi et al. utilized DBM alone in 29.8% of patients, drill reamings in 63.8%, and ICBG in 6.4% to yield a 93% rate of union. [21] Despite their usage of DBM in nearly a third of their patients, their reoperation rate only approximated 7%. However, they did not differentiate between healing rates for those with DBM vs local grafting. Still, one must exercise caution in choosing an allograft substitute. Variation in each company's bone supply and mode of preparation yields varying qualities of DBM. For instance, Peterson et al. found that Grafton putty yielded the most fusion material at eight weeks in athymic rats when comparing three brands of DBM. [34] Allograft bone substitute has also been studied in combination with autograft with similar success. Morone and Boden demonstrated that decreased autograft volume could be supplemented with DBM gel to yield fusion rates similar to those following use of autograft alone. [35] Overall, as many different allograft sources are available, at this point, the best source is yet to be determined. Multiple factors influence the surgeons' choice and cannot be explored in depth in this paper.
Our study demonstrated an 84% clinical healing rate with an overall complication rate of 26%. Although the authors recognize that the clinical success rate was 84%, the three individuals without radiographic evidence of healing cannot be considered truly "healed" as the goal of using biologic enhancement is to obtain bony healing. Radiographic healing is truly the best indicator of success of the use of allograft. Thus, our radiographic healing rate of 68% is certainly not equivalent to the reported healing rates in the literature for autograft, which range from 89 to 100%. Although the complication rate is slightly higher than those in the studies using ORIF with ICBG, those reported rates mostly focused on graft-site morbidity-not the complications regarding the surgical procedure itself. [3] Two of our complications were minor and involved painful hardware that was removed. However, three of the complications were persistent nonunions, two of which failed catastrophically. Thirty-seven percent of the patients in this study were smokers and in particular, the three patients with persistent nonunions each smoked at least one pack of cigarettes daily. Although it did not reach statistical significance (P=0.08), the numbers do suggest that a trend may be present and perhaps a smoking history should be the reason for pause when using allograft bone substitute. This trend is supported by Ziran et al. who noted healing rates of 67.9% and 87.5% in smokers and nonsmokers receiving allograft for fractures and nonunions, respectively. [36] Likewise, Endrizzi et al. noted that their only reoperations were on smoking patients (N=3). [21]
We believe that those with segmental bony defects should receive ICBG. We did exclude these patients from our study and did not review their charts further (The incorporation of an autogenous graft with structural integrity in this instance theoretically appears superior and is supported in the literature). Ballmer et al. had 100% union rate at six months in patients receiving tricortical ICBG for segmental clavicular defects greater than or equal to 15 mm. [9] Additionally, Endrizzi et al. also refrained from DBM in segmental defects, however, they did not specify what size of defect would lead them to ICBG. [21]
Two issues arose when examining the graft sources chosen to augment plate fixation in this study. Although DBM was the primary graft source (68%), allograft corticocancellous bone chips (37%) supplemented with rh-BMP (5%) and calcium phosphate (5%) were also included. This study's intention was not to isolate a particular substance to prove similar efficacy to ICBG. Rather, it was to present a series of patients supplemented with a nonautogenous graft source rather than ICBG and demonstrate its efficacy at healing clavicle nonunions. Admittedly, this is a limitation of the study. However, this is not a commonly seen operative problem, and the graft sources of the treating surgeons did change throughout the years of retrospective data collection. Ideally, we would have used identical graft choices in each patient. In addition to the heterogeneity in graft choice, we incorporated PRP at the nonunion site in 12 (63%) of patients to augment healing. It is unknown whether this helped stimulate healing. Previous studies showed mixed results with its efficacy in stimulating bone formation. Sanchez et al. reported healing of all femoral nonunions (N=15) with injection of PRP in conjunction with allograft, despite two requiring repeated percutaneous injections. [37] Likewise, Han et al. found significant increases in DBM osteoinductivity with PRP when not activated by thrombin. [38] However, another study by Mariconda et al. demonstrated no improvements in union rates or time to union when PRP was injected into atrophic tibial, humeral, or forearm nonunions. [39] Markou et al. showed no difference in bone formation for periodontal bone defects treated with either PRP or PRP and allograft. [40] We cannot draw any conclusions on PRP based on our study. However, our results demonstrate that allograft bone substitute, in a variety of forms, has the potential to facilitate healing in a clavicular nonunion, in particular, in a non-smoker.
Although this study is the first to look only at clavicular nonunions treated with ORIF and bone graft substitute, it does have several limitations. It is a retrospective case series without randomization to a treatment group, and as stated above, has a lack of standardization to treatment when utilizing allograft source choices. Eighteen of the fractures were fixed with a locking clavicle plate; however, one was treated with a pelvic recon plate. A "cleaner" study would employ the same type of fixation for all fractures. One fracture was more medial and is susceptible to different forces across the fracture site and thus perhaps a different union potential, but it was rigidly fixed with a locking plate. However, our goal was to look at all clavicle nonunions to evaluate the efficacy of allograft as an alternative and successful treatment option when compared with ICBG. We believe our data do demonstrate acceptable healing rates without graft-site morbidity. However, we do recognize that our healing rates are inferior to the reported healing rates for the use of allograft. Lastly, follow-up was not optimally standardized with functional assessments or complete radiographic profiles to ensure healing as several patients ceased to follow-up once they had obtained clinical evidence of healing.
 Conclusion Conclusion | |  |
Despite these limitations, this is the only series found in the literature evaluating clavicle nonunion healing rates grafted exclusively with allograft bone substitute sources. Based on our current results, ORIF with a bone graft substitute source is a viable alternative to ICBG when treating clavicle nonunions. Our healing rates with allograft are lower than reported rates utilizing ICBG, but our method does eliminate graft-site morbidity. However, smokers may have a higher risk for failure with allograft, although this was not found to be statistically significant. When clavicle nonunions persist after surgical treatment, the failures can be catastrophic and difficult to revise. Thus, given this trend, ORIF and ICBG may better serve patients with a smoking history. We are currently enrolling patients in a prospective case series to re-examine the efficacy of ORIF with DBM in clavicular nonunions to standardize treatment and to formally evaluate patient's clinical progress with standardized outcomes measurements and complete radiographic analysis. We hope this will shed more light on this complicated problem.
 References References | |  |
| 1. | Manske DJ, Szabo RM. The operative treatment of mid-shaft clavicular non-unions. J Bone Joint Surg Am 1985;67:1367-71. 
[PUBMED] [FULLTEXT] |
| 2. | Jupiter JB, Leffert RD. Non-union of the clavicle. Associated complications and surgical management. J Bone Joint Surg Am 1987;69:753-60. 
[PUBMED] |
| 3. | Bradbury N, Hutchinson J, Hahn D, Colton CL. Clavicular nonunion. 31/32 healed after plate fixation and bone grafting. Acta Orthop Scand 1996;67:367-70. 
[PUBMED] |
| 4. | Neer CS 2 . Nonunion of the clavicle. J Am Med Assoc 1960;172:1006-11. 
|
| 5. | Brinker MR, Edwards TB, O'Connor DP. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2005;87:676-7. 
[PUBMED] [FULLTEXT] |
| 6. | Wilkins RM, Johnston RM. Ununited fractures of the clavicle. J Bone Joint Surg Am 1983;65:773-8. 
[PUBMED] [FULLTEXT] |
| 7. | Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004;86-A:1359-65. 
[PUBMED] [FULLTEXT] |
| 8. | Olsen BS, Vaesel MT, Sojbjerg JO. Treatment of midshaft clavicular nonunion with plate fixation and autologous bone grafting. J Shoulder Elbow Surg 1995;4:337-44. 
|
| 9. | Ballmer FT, Lambert SM, Hertel R. Decortication and plate osteosynthesis for nonunion of the clavicle. J Shoulder Elbow Surg 1998;7:581-5. 
[PUBMED] |
| 10. | Ebraheim NA, Mekhail AO, Darwich M. Open reduction and internal fixation with bone grafting of clavicular nonunion. J Trauma 1997;42:701-4. 
[PUBMED] [FULLTEXT] |
| 11. | Marti RK, Nolte PA, Kerkhoffs GM, Besselaar PP, Schaap GR. Operative treatment of mid-shaft clavicular non-union. Int Orthop 2003;27:131-5. 
[PUBMED] [FULLTEXT] |
| 12. | Fowler BL, Dall BE, Rowe DE. Complications associated with harvesting autogenous iliac bone graft. Am J Orthop (Belle Mead NJ) 1995;24:895-903. 
[PUBMED] |
| 13. | Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res 1996;329:300-9. 
[PUBMED] |
| 14. | Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res 1997;339:76-81. 
[PUBMED] |
| 15. | Keller EE, Triplett WW. Iliac bone grafting: Review of 160 consecutive cases. J Oral Maxillofac Surg 1987;45:11-4. 
[PUBMED] [FULLTEXT] |
| 16. | Kurz LT, Garfin SR, Booth RE Jr. Harvesting autogenous iliac bone grafts. A review of complications and techniques. Spine (Phila Pa 1976) 1989;14:1324-31. 
|
| 17. | Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am 2002;84-A:716-20. 
[PUBMED] [FULLTEXT] |
| 18. | Friedlaender GE, Perry CR, Cole JD, Cook SD, Cierny G, Muschler GF, et al. Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions. J Bone Joint Surg Am 2001;83-A Suppl 1: S151-8. 
[PUBMED] [FULLTEXT] |
| 19. | Hierholzer C, Sama D, Toro JB, Peterson M, Helfet DL. Plate fixation of ununited humeral shaft fractures: Effect of type of bone graft on healing. J Bone Joint Surg Am 2006;88:1442-7. 
[PUBMED] [FULLTEXT] |
| 20. | Lee KJ, Roper JG, Wang JC. Demineralized bone matrix and spinal arthrodesis. Spine J 2005;5:217S-23S. 
[PUBMED] [FULLTEXT] |
| 21. | Endrizzi DP, White RR, Babikian GM, Old AB. Nonunion of the clavicle treated with plate fixation: A review of forty-seven consecutive cases. J Shoulder Elbow Surg 2008;17:951-3. 
[PUBMED] [FULLTEXT] |
| 22. | Schuind F, Pay-Pay E, Andrianne Y, Donkerwolcke M, Rasquin C, Burny F. External fixation of the clavicle for fracture or non-union in adults. J Bone Joint Surg Am 1988;70:692-5. 
[PUBMED] [FULLTEXT] |
| 23. | Boehme D, Curtis RJ Jr, DeHaan JT, Kay SP, Young DC, Rockwood CA Jr. Non-union of fractures of the mid-shaft of the clavicle. Treatment with a modified Hagie intramedullary pin and autogenous bone-grafting. J Bone Joint Surg Am 1991;73:1219-26. 
[PUBMED] [FULLTEXT] |
| 24. | Millett PJ, Hurst JM, Horan MP, Hawkins RJ. Complications of clavicle fractures treated with intramedullary fixation. J Shoulder Elbow Surg 2011;20:86-91. 
[PUBMED] [FULLTEXT] |
| 25. | Strauss EJ, Egol KA, France MA, Koval KJ, Zuckerman JD. Complications of intramedullary Hagie pin fixation for acute midshaft clavicle fractures. J Shoulder Elbow Surg 2007;16:280-4. 
[PUBMED] [FULLTEXT] |
| 26. | Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma 1989;3:192-5. 
[PUBMED] |
| 27. | Tashjian RZ, Horwitz DS. Healing and graft-site morbidity rates for midshaft clavicle nonunions treated with open reduction and internal fixation augmented with iliac crest aspiration. Am J Orthop (Belle Mead NJ) 2009;38:133-6. 
[PUBMED] |
| 28. | Momberger NG, Smith J, Coleman DA. Vascularized fibular grafts for salvage reconstruction of clavicle nonunion. J Shoulder Elbow Surg 2000;9:389-94. 
[PUBMED] [FULLTEXT] |
| 29. | Fuchs B, Steinmann SP, Bishop AT. Free vascularized corticoperiosteal bone graft for the treatment of persistent nonunion of the clavicle. J Shoulder Elbow Surg 2005;14:264-8. 
[PUBMED] [FULLTEXT] |
| 30. | Strates BS, Stock AJ, Connolly JF. Skeletal repair in the aged: A preliminary study in rabbits. Am J Med Sci 1988;296:266-9. 
[PUBMED] |
| 31. | Urist MR, Behnam K, Kerendi F, Raskin K, Nuygen TD, Shamie AN, et al. Lipids closely associated with bone morphogenetic protein (BMP)-and induced heterotopic bone formation. With preliminary observations of deficiencies in lipid and osteoinduction in lathyrism in rats. Connect Tissue Res 1997;36:9-20. 
[PUBMED] |
| 32. | Sammarco VJ, Chang L. Modern issues in bone graft substitutes and advances in bone tissue technology. Foot Ankle Clin 2002;7:19-41. 
[PUBMED] |
| 33. | Gardner MJ, Toro-Arbelaez JB, Harrison M, Hierholzer C, Lorich DG, Helfet DL. Open reduction and internal fixation of distal femoral nonunions: Long-term functional outcomes following a treatment protocol. J Trauma 2008;64:434-8. 
[PUBMED] [FULLTEXT] |
| 34. | Peterson B, Whang PG, Iglesias R, Wang JC, Lieberman JR. Osteoinductivity of commercially available demineralized bone matrix. Preparations in a spine fusion model. J Bone Joint Surg Am 2004;86-A:2243-50. 
[PUBMED] [FULLTEXT] |
| 35. | Morone MA, Boden SD. Experimental posterolateral lumbar spinal fusion with a demineralized bone matrix gel. Spine (Phila Pa 1976) 1998;23:159-67. 
|
| 36. | Ziran BH, Hendi P, Smith WR, Westerheide K, Agudelo JF. Osseous healing with a composite of allograft and demineralized bone matrix: Adverse effects of smoking. Am J Orthop (Belle Mead NJ) 2007;36:207-9. 
[PUBMED] |
| 37. | Sanchez M, Anitua E, Cugat R, Azofra J, Guadilla J, Seijas R, et al. Nonunions treated with autologous preparation rich in growth factors. J Orthop Trauma 2009;23:52-9. 
[PUBMED] [FULLTEXT] |
| 38. | Han B, Woodell-May J, Ponticiello M, Yang Z, Nimni M. The effect of thrombin activation of platelet-rich plasma on demineralized bone matrix osteoinductivity. J Bone Joint Surg Am 2009;91:1459-70. 
[PUBMED] [FULLTEXT] |
| 39. | Mariconda M, Cozzolino F, Cozzolino A, D'Agostino E, Bove A, Milano C. Platelet gel supplementation in long bone nonunions treated by external fixation. J Orthop Trauma 2008;22:342-5. 
[PUBMED] [FULLTEXT] |
| 40. | Markou N, Pepelassi E, Vavouraki H, Stamatakis HC, Nikolopoulos G, Vrotsos I, et al. Treatment of periodontal endosseous defects with platelet-rich plasma alone or in combination with demineralized freeze-dried bone allograft: A comparative clinical trial. J Periodontol 2009;80:1911-9. 
[PUBMED] [FULLTEXT] |
[Figure 1], [Figure 2]
[Table 1]
|
