| |


 |
| Year : 2011 | Volume
: 5
| Issue : 4 | Page : 105-107 |
|
|
|
|
|
TECHNICAL TIP Combining of small fragment screws and large fragment plates for open reduction and internal fixation of periprosthetic humeral fractures
Dominik Seybold, Mustafa Citak, Matthias Königshausen, Jan Gessmann, Thomas A Schildhauer
Department of General and Trauma Surgery, Berufsgenossenschaftliches-Universitätsklinikum Bergmannsheil, Ruhr-University Bochum, Germany
Correspondence Address:
Dominik Seybold
Department of General and Trauma Surgery, Berufsgenossenschaftliches-Universitätsklinikum Bergmannsheil, Ruhr-University Bochum, Bürkle-de-la-Camp-Platz 1, D-44789, Bochum
Germany
 Source of Support: None, Conflict of Interest: None  | 3 |
DOI: 10.4103/0973-6042.91004

|
|
|
|
| Date of Web Publication | 20-Dec-2011 |
 Abstract Abstract | | |
Operative treatment of periprosthetic humeral fractures in elderly patients with osteoporotic bone requires a stable fixations technique. The combination of 3.5 cortical screws with washers in a 4.5 Arbeitsgemeinschaft fόr Osteosynthesefragen, Limited-contact dynamic compression plate or Locking plate, allows a stable periprosthetic fixation with the small 3.5 screws and 4.5 screws above and below the prosthesis, respectively. This combination is a cost-effective technique to treat periprosthetic humeral fractures.
Keywords: Complications, new operative techniques, periprosthetic humerus fracture, shoulder arthroplasty
How to cite this article:
Seybold D, Citak M, Königshausen M, Gessmann J, Schildhauer TA. Combining of small fragment screws and large fragment plates for open reduction and internal fixation of periprosthetic humeral fractures. Int J Shoulder Surg 2011;5:105-7 |
How to cite this URL:
Seybold D, Citak M, Königshausen M, Gessmann J, Schildhauer TA. Combining of small fragment screws and large fragment plates for open reduction and internal fixation of periprosthetic humeral fractures. Int J Shoulder Surg [serial online] 2011 [cited 2016 Apr 25];5:105-7. Available from: http://www.internationalshoulderjournal.org/text.asp?2011/5/4/105/91004 |
 Introduction Introduction | |  |
Fractures of the humerus in patients with total shoulder replacement are rare and difficult to address. Due to the increasing numbers of total shoulder replacements every year, especially in older patients, periprosthetic fractures are becoming more frequent. The incidence of periprosthetic fractures in the humerus is reported to be between 1.6% and 2.4%. [1],[2] Risk factors include osteoporosis, rheumatoid arthritis, age and female gender. [1],[3],[4],[5] The treatment of periprosthetic humeral fractures depends on the location of the fracture in relation to the humeral stem and the stability of the stem/bone interface. [2],[4],[5] Notably, an unstable prosthesis necessitates an anatomic reduction, followed by revision to a long-stemmed prosthesis. When the prosthesis is stable, fracture reduction and fixation is recommended. The overall treatment goal is to preserve the pre-fracture shoulder function, reduce pain with early functional treatment and achieve fracture healing. Therefore, operative and conservative treatment options are available. [6],[7],[8],[9],[10] Conservative treatment with bracing and immobilization provides limited patient comfort, especially in elderly patients, and is only suitable for fractures proximal or distal to the stem/bone interface with a stable prosthesis (Campbell type I and IV). [4]
Operative fracture stabilization in patients with a stable prosthesis allows early mobilization and anatomic fracture reduction. The main problem in open reduction and fixation of periprosthetic fractures is the poor bone quality in the elderly patient and the cemented or non-cemented stem of the prosthesis. Different fixation options are available that use plates, cables and cerclage wires or strut grafts for use as the cortical allograft. [11] The goal of this technical note is to describe a simple and cost-efficient technique to achieve a stable plate fixation with standard AO (Arbeitsgemeinschaft fόr Osteosynthefragen) implants in periprosthetic fractures of the humerus
 Technique Description Technique Description | |  |
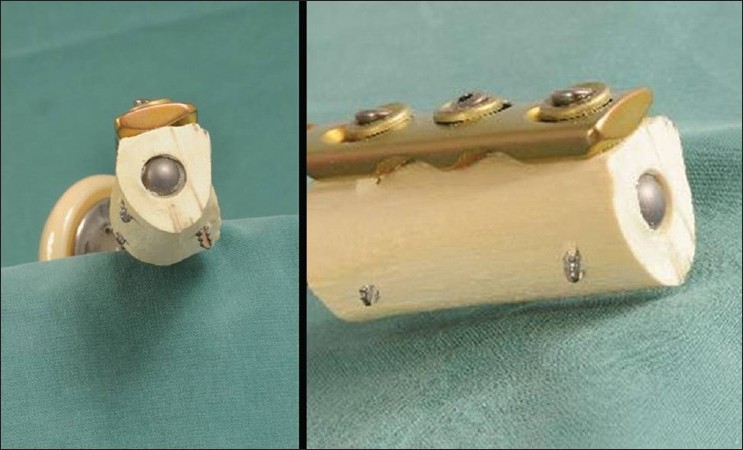
For stable fixation of a periprosthetic humeral fracture with a stable prosthesis, a plate such as a 4.5 AO limited-contact dynamic compression plate (LC-DCP) or locking plate (LCP) is required to achieve adequate fixation strength. The use of long plates provides additional stability by reducing the lever arm of the bone fragments. The cortical 4.5 screws are difficult to place around the stem of the prosthesis sometimes due to osteoporotic and thin cement/bone interface. The combination of a 4.5 plate and cortical 3.5 screws can facilitate periprosthetic fixation. Therefore, we used the 4.5 AO LC-DCP or LCP and the 3.5 cortical self tapping screws with a washer (4.0 Kφnigsee system), to fix the 3.5 screw head in the LCD-CP or LCP hole of the 4.5 plate [Figure 1]. The 3.5 self tapping screws with washers were used to fix the 4.5 plates into the proximal fragment around the prosthesis. After predrilling with the standard AO 2.5 mm drill (steel) close to the prosthesis into the bone cement interface, the 3.5 self tapping screws were inserted. Angulation of the screws and the alternating hole-offset of the 4.5 AO plates allowed a safe fixation of the screws along the prosthesis [Figure 2]. At the non-prosthetic fracture side, normal 4.5 screws or LCP screws were implanted [Figure 3].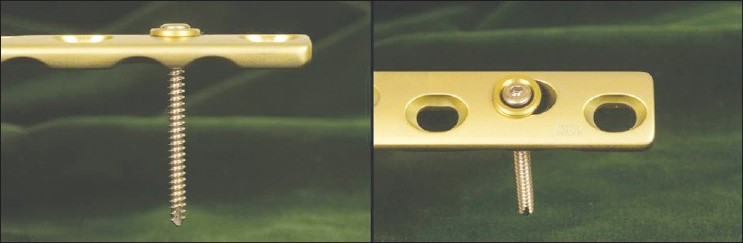 | Figure 1: 3.5 cortical screw with a washer fits into a large 4.5 AO LC-DCP (limited-contact dynamic compression plate)
Click here to view |
 | Figure 2: Insertion of the screws around the prosthesis in a sawbone model. An angulation of the 3.5 screws (with washers) within 45 degrees is possible
Click here to view |
 | Figure 3: Patient one and two, two years after open reduction and internal fixation with the periprosthetic combination of 3.5 cortical screws with washers and 4.5 plates
Click here to view |
 Patients Patients | |  |
Two female patients aged 75 and 60 years sustained periprosthetic fractures of the humerus after falling on the outstretched arm. Both shoulder prostheses were cemented and stable. The fracture type was a spiral Campbell type III in both patients. [4] Bone quality was poor due to osteoporosis. Both patients were treated operatively with a 4.5 AO plate (small in one and large in the other) patient, with 3.5 cortical screws fixed with washers around the cemented stem of the prosthesis in each patient [Figure 3]. The plates were placed anteriorly and anterolaterally. Both patients were moved to a functional rehabilitation program immediately after surgery. No immobilization was required. Both patients achieved preoperative level of range of motion (ROM) and shoulder function after fracture healing.
 Discussion Discussion | |  |
The incidence of periprosthetic fractures is increasing among elderly patients due to the increasing age of the population and the rising numbers of joint replacements. [12] The incidence of periprosthetic humeral fractures after shoulder arthroplasty is rather low compared to the incidence of periprosthetic fractures around the hip or knee. [13],[14] Moreover, a functional deficit of the upper extremities becomes even more debilitating in elderly people after these injuries, as overall mobility is reduced. Therefore, the overall goal in periprosthetic fracture treatment of the humerus is to restore the function of the upper limb. Different conservative and operative treatment options are available. The conservative treatment is very restrictive for the patient due to the long immobilization time period in a sling or a brace. This approach is also associated with frequent skin problems and is only suitable for fractures distal or proximal to the prosthesis with a spiral component; and, no cement at the fracture site. Open reduction and fixation allows the patient to achieve prefracture-level mobility faster than the conservative treatment approach. The main problems encountered in the elderly patients while administering the operative treatment approach are the poor bone quality and the periprosthetic fixation.
Different plate modifications have been described, including the Dall-Miles plate with cerclage cables. [15] The cable fixation technique compromises soft tissues due to the circular deperiostation of the bone; and therefore, is frequently not used. Until now, there have been no plate systems available that combine small screws with 4.5 plates. For a good periprosthetic fixation, a small screw diameter and the ability to place the screw at different angles are crucial. Using small 3.5 cortical screws with washers in a large LCP 4.5 plate allows surgeons to achieve successful periprosthetic fixation and stable angle fixation, with the LCP screws above or below the prosthesis. In the future, it would be preferable to have the ability to combine both 3.5 and 4.5 systems with multidirectional- angled stable screws.
 Conclusions Conclusions | |  |
In periprosthetic fractures of the humerus, a combination of small 3.5 screws with washers in stable large 4.5 plates can ease open reduction and fixation. The use of washers in 4.5 plates is a cost-effective method that can be used to achieve stable periprosthetic fixation with small 3.5 cortical screws.
 References References | |  |
| 1. | Boyd AD, Thornhill TS, Barnes CL. Fractures adjacent to humeral prostheses. J Bone Joint Surg Am 1992;74:1498-504. 
|
| 2. | Worland RL, Kim DY, Arredondo J. Periprosthetic humeral fractures: Management and classification. J Shoulder Elbow Surg 1999;8:590-4. 
[PUBMED] |
| 3. | Cameron B, Iannotti JP. Periprosthetic fractures of the humerus and scapula: Management and prevention. Orthop Clin North Am 1999;30:305-18. 
[PUBMED] |
| 4. | Campbell JT, Moore RS, Iannotti JP, Norris TR, Williams GR. Periprosthetic humeral fractures: Mechanisms of fracture and treatment options. J Shoulder Elbow Surg 1998;7:406-13. 
[PUBMED] |
| 5. | Wright TW, Cofield RH. Humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am 1995;77:1340-6. 
[PUBMED] [FULLTEXT] |
| 6. | Raiss P, Aldinger PR, Kasten P, Rickert M, Loew M. Total shoulder replacement in young and middle-aged patients with glenohumeral osteoarthritis. J Bone Joint Surg Br 2008;90:764-9. 
[PUBMED] [FULLTEXT] |
| 7. | Christoforakis JJ, Sadig S, Evans MJ. Use of a Dall-Miles plate and cables for the fixation of a periprosthetic humeral fracture. Acta Orthop Belg 2003;69:562-5. 
|
| 8. | Kent ME, Sinopidis C, Brown DJ, Frostick SP. The locking compression plate in periprosthetic humeral fractures: A review of two cases. Injury 2005;36:1241-5. 
[PUBMED] [FULLTEXT] |
| 9. | Kim DH, Clavert P, Warner JJ. Displaced periprosthetic humeral fracture treated with functional bracing: A report of two cases. J Shoulder Elbow Surg 2005;14:221-3. 
[PUBMED] [FULLTEXT] |
| 10. | Lill H, Hepp P, Rose T, Korner J, Josten C. Mennen clamp-on plate fixation of periprosthetic fractures of the humerus after shoulder arthroplasty: A report on 3 patients. Acta Orthop Scand 2004;75:772-4. 
[PUBMED] |
| 11. | Kumar S, Sperling JW, Haidukewych GH, Cofield RH. Periprosthetic humeral fractures after shoulder arthroplasty. J Bone Joint Ssurg Am 2004;86 A:680-9. 
|
| 12. | Gruner A, Hockertz T, Reilmann H. Periprosthetic fractures: Classification, management, therapy. Unfallchirurg 2004;107:35-49. 
[PUBMED] |
| 13. | Zuurmond RG, van Wijhe W, van Raay JJ, Bulstra SK. High incidence of complications and poor clinical outcome in the operative treatment of periprosthetic femoral fractures: An analysis of 71 cases. Injury 2010;41:629-33. 
[PUBMED] [FULLTEXT] |
| 14. | Platzer P, Schuster R, Aldrian S, Prosquill S, Krumboeck A, Zehetgruber I, et al. Management and outcome of periprosthetic fractures after total knee arthroplasty. J Trauma 2010;68:1464-70. 
[PUBMED] [FULLTEXT] |
| 15. | Christoforakis JJ, Sadiq S, Evans MJ. Use of a Dall-Miles plate and cables for the fixation of a periprosthetic humeral fracture. Acta Orthop Belg 2003;69:562-5. 
|
[Figure 1], [Figure 2], [Figure 3]
| This article has been cited by | | 1 |
Management of shoulder periprosthetic fractures: Our institutional experience and review of the literature |
|
| Mineo, G.V. and Accetta, R. and Franceschini, M. and DellæAcqua, G.P. and Calori, G.M. and Meersseman, A. | | Injury. 2013; 44(SUPPL.1): S82-S85 | | [Pubmed] | | | 2 |
Management of shoulder periprosthetic fractures: Our institutional experience and review of the literature |
|
| G.V. Mineo,R. Accetta,M. Franceschini,G. Pedrotti DellæAcqua,G.M. Calori,A. Meersseman | | Injury. 2013; 44: S82 | | [Pubmed] | [DOI] | |
|
 |
|
