| |


 |
| Year : 2011 | Volume
: 5
| Issue : 4 | Page : 85-89 |
|
|
|
|
|
ORIGINAL ARTICLE Is removal of clavicle plate after fracture union necessary?
Janey Wang, Ramiah Chidambaram, Daniel Mok
Department of Orthopaedic Surgery, Epsom and St Helier NHS Trust, Shoulder Unit, Epsom General Hospital, Surrey, UK,
Correspondence Address:
Daniel Mok
2906 Bank of America Tower, 12 Harcourt Road, Central, Hong Kong
 Source of Support: None, Conflict of Interest: None  | 3 |
DOI: 10.4103/0973-6042.90998

|
|
|
|
| Date of Web Publication | 20-Dec-2011 |
 Abstract Abstract | | |
Purpose: To review whether clavicle plates should be removed after union of the fracture.
Materials and Methods: 48 patients with middle third clavicle fractures treated by plating were assessed with UCLA shoulder rating and Oxford shoulder scores.
Results: At an average follow up of 13 months,96% of 27 patients with plates out recommended its removal. 86% of 21 patients with plates in were happy to keep them.
Conclusions : We recommend leaving clavicle plates in unless requested by the patient.
Level of Evidence: I V-retrospective study.
Keywords: Clavicle fracture, complications, internal fixation
How to cite this article:
Wang J, Chidambaram R, Mok D. Is removal of clavicle plate after fracture union necessary?. Int J Shoulder Surg 2011;5:85-9 |
 Introduction Introduction | |  |
The incidence of midshaft clavicular fracture is common and at 50 fractures per 100,000 person-years. [1],[2] Traditional teaching recommended non-operative treatment as 99% would be expected to heal with little residual symptoms apart from shortening. [3],[4] Esokola in 1986 reported 27% of his patients continued to have pain at 2 years if their united clavicle were short by 15 mm or more. [5] In 1998, Robinson studied 1000 clavicle fractures treated non-operatively. He found delayed union developed in 2.7% and non-union in 4.8%. These were all in displaced fractures. [6] Results of a Canadian multicenter prospective study between non-operative treatment and plating have confirmed superior results in favor of surgery. [7] Since then, open reduction and fixation of displaced clavicle fractures is accepted by most surgeons. While plate fixation is the commonest surgical options, scar-related pain and numbness distal to the scar were often complained by patients with plates. [7] Plates were often not removed unless they became symptomatic. The aim of our study is to assess whether clavicle plates caused symptoms when they were left in.
 Materials and Methods Materials and Methods | |  |
In this retrospective study, patients were divided into two groups. Those who still have their plates in and those whose plates been taken out. We used Oxford Shoulder score and UCLA shoulder rating scale to assess shoulder function at rest, work, and sports. We also administered a patient-based questionnaire to assess the following: presence of discomfort, cosmetic concern related to the plate, ability to return to sports, and ability to carry a backpack. In patients with plate removed, we asked about their shoulder function outcome compared to that with the period when they had the plate-in. We also quantified the severity of pain/discomfort in each patient by asking their symptom at rest, at work, and during sports. For both groups, we asked if they were satisfied with the treatment and whether they would recommend the same if injured again [Table 1]. To assess morbidity of the plate removal procedure, we asked the patients time taken to return to work and sports and whether they had any complications. This study was approved by our institutional committee.
Between 2005 and 2009, 48 patients with displaced middle third clavicle fractures treated with plate fixation at our institution were available for review. Forty-two were male and six were female with an average age of 40 (15-79) years. Their average follow-up was 13 (12-22) months. We classified each fracture according to Robinson's system [5] [Table 2].
Statistical analysis was performed using the SPSS version 16 software. Fisher's exact test was used to assess the patient's satisfaction and if there were any reported complications. Mann-Whitney U test was used to assess the difference of the days returned to work and sports between the plate-in and plate-out groups.
 Results Results | |  |
Of the 48 patients, 27 (56%) had their plates removed (plate-out) and 21 (44%) still have their plates in (plates-in). Five patients had LCDCP (Synthes) and 43 had anatomic plates (Acumed). The mean age in the plate-out group was 40 years compared with 42 years in the plate-in group; 81% of the plate-out group participated in active sports compared with 67% in plate-in group.
Both categories of patients scored well in the Oxford and UCLA score for their shoulder function. The average Oxford Shoulder score is 13 for plate-out patients and 16 for plate-in patients. The average UCLA shoulder rating scale is 34 for both groups. There was no statistical difference between the plate-out and plate-in groups in both Oxford Shoulder score (P = 0.178) and UCLA score (P = 0.293).
Reasons for plate removal included local symptoms of pain and discomfort (6 patients), limited range of motion in the shoulder during rigorous sports (13 patients), interferences of daily living activity (10 patients), and concern of refracture around the plate (3 patients).
In plate-out group, 18 (67%) patients had both discomfort and problems related to the plate prominence prior to its removal. Nine (33%) patients only had problem related to local prominence; 26 (96%) patients had complete resolution of both issues after their plates were taken out. One patient, whose clavicle fracture was associated with a brachial plexus injury from a motor vehicle accident, continued to experience neurologic pain after removal of the plate; 15 (70%) patients who participated in extensive athletic activities expressed an improvement in their shoulder function.
Following plate removal, the mean number of days returning to work was 14 (1-90) days and to sports was 26 (1-150) days. Three patients in the plate-out group sustained a further fracture of their clavicle after plate removal. Two patients were involved in a separate motor vehicle accident and a third through an inter-fragmentary screw hole several weeks after plate removal. One patient in the plate-in group developed infection which responded to oral antibiotics treatment. Twenty-six (96%) of -27 patients who had the plate removed were satisfied with the outcome of the procedure and would recommend removal of the plate.
In the group of patients with their plates still in, 15 (71%) complained of local pain/discomfort and plate prominence. This when the clavicle was impacted upon, or plate getting caught while carrying objects as well as an unusual sensation during weather changes [Table 3]. Patients who had the plate in stated they were never offered to have the plate out (4 patients, 19%) or did not feel symptoms were severe enough to go through another procedure (4 patients, 19%). Eighteen (86%) patients were satisfied with the outcome and would only consider plate removal if it interfere with patients' quality of life. Only three (14%) patients would consider plate removal.
A total of 36 patients participated in extensive sporting activities; 23 had plates out and 13 still had plates in. All 23 (100%) patients without plates had alleviation of their discomfort after plate removal compared with only 2 (15%) with plates in who were asymptomatic.
 Discussion Discussion | |  |
Plating, anatomic with contour matching that of the clavicle, with or without locking as well as intramedullary devices such as locked pins or elastic nails are contemporary fixation devices. In a biomechanical analysis, reconstruction plate was found to be weaker to bending than locking plates and LCDCP, particularly in the presence of cortical defects. Clavicle pins (Rockwood, Depuy) performed poorly compared with the plates. [8] Precontoured plates fixed with unicortical locking screws did not show superior results when compared with those fixed with bicortical non-locking screws. [9] The authors concluded the stiffer plate fixation enables early return to daily functions for the patients.
Intramedullary devices result in better cosmetic appearance for the patients but carried a higher complication rate of 25.8%. [10] The narrow isthmus of the lateral medullary canal is difficult to negotiate for initial pin insertion. The authors experienced non-union of 8.6% requiring revision and 17.2% minor complications related to wound infections, hardware failure, and skin erosions by the pin. In addition, hardware removal is necessary. While pin fixation can be useful in holding the reduction of simple displaced midshaft fractures, those with multifragmentary fractures are not suitable.
Plate fixation remains the treatment of choice for most surgeons. [7],[11],[12],[13],[14],[15],[16],[17] Plating on the superior surface of the clavicle is technically easier than anterior or anteroinferior plating. Most plates mentioned in the literature were often reconstruction plates and LCDCP. The former broke easily and the latter were bulky. [9],[11] Both factors contributed unfavorably to the outcome of plating. Shen reported 171 of 232 patients had their plates removed, mostly for cultural reasons and hardware prominence. [15] In the Canadian multicenter study, most of their 13.4% complications after plate fixation were hardware-related. These complications were resolved after plate removal in all cases. [8] In order to overcome problems of superior plate irritation, some surgeons adopted anterior plating of the fractured clavicle. They argued this has the additional benefit of drilling away from neurovascular structures that lie beneath the clavicle as well as gaining more purchase in the bone compared with the shorter screws of superior plating. [18]
To our knowledge, we are not aware of any prior study on the assessment of patients' symptoms related to their clavicle plates. We used a patient-based subjective questionnaire to analyze the impact of plates in patients who had them left in and compared with a group who had them electively removed.
In spite of introduction of anatomic plates (Acumed, USA) in our practice, 88% of patients with plate fixations complained of local prominence, pain, and discomfort. In patients who have their plates removed, 96% were satisfied as their symptoms completely resolved. They would recommend having the clavicle plate removed. The second operation to remove the plate, however, is not without morbidity. [15] One patient (3.7%) sustained a further fracture through a previous inter-fragmentary screw hole and two other through a separate accident in the group of patients with their plates out. On the contrary, we did not find a single spontaneous fracture in patients with clavicle plate in. This effectively refutes the anecdotal view that clavicle plate left in would become stress riser resulting in a higher incidence of refracture. Review of the group of patients who kept their plate in has shown that plate removal was not universally offered as an option. Although 88% of patients experienced discomfort related to the plate, 86% felt they would not want to go through a second procedure to have their plates taken out. It is worth noting that there was no statistical difference in shoulder function in both groups. On balance, we would not recommend routine plate removal after consolidation of clavicle fracture unless requested by the patient.
Limitations of the study were that being retrospective, patients in each group were likely to have been preselected to have either the plate out or in by surgeons in charge of their care. The patients would have been given an explanation as to why the plates should be removed or not at the index operation. This may have influenced each patient's subsequent assessment about their plates. In addition, the operative experience of different surgeons was variable. This may have resulted in improper plate placement [Figure 1] and in turn may have contributed toward patient's discomfort. In our series, even patients with perfect anatomic plate placement developed symptoms. We did not find any statistical correlation between different plates against symptoms or between plate positions and symptoms.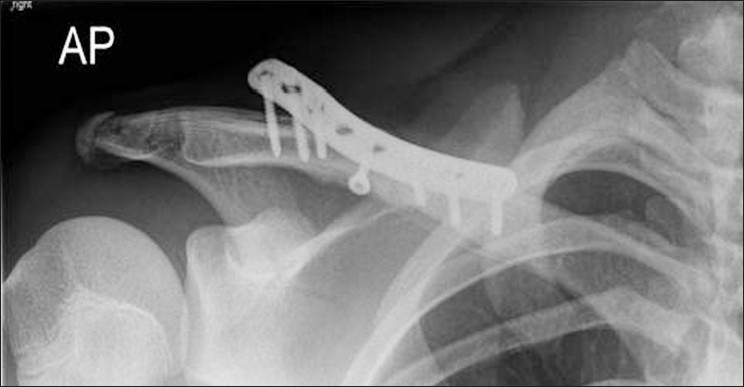 | Figure 1: Eight holes Acumed plate with the lateral end lifted up above the clavicle. Fracture united
Click here to view |
 Conclusion Conclusion | |  |
Our study has shown that over 88% of plates over the united clavicle can cause clinical symptoms, particularly in younger patients who are involved with extensive athletic activities; 96% of patients who had their plate taken out recommended its removal; 86% of those who still have their plates in were happy to keep them. As plate removal is not without its morbidity, we recommend leaving clavicle plates in unless requested by the patient.
 References References | |  |
| 1. | Nowak J, Mallmin H, Larsson S. The aetiology and epidemiology of clavicular fractures. A prospective study during a two-year period in Uppsala, Sweden. Injury 2000;31:353-8. 
[PUBMED] [FULLTEXT] |
| 2. | Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: A prospective study of 222 patients. Acta Orthopaedica 2005;76:496-502. 
[PUBMED] [FULLTEXT] |
| 3. | Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: End result study after conservative treatment. J Orthop Trauma 1998;12:572-6. 
[PUBMED] [FULLTEXT] |
| 4. | Neer CS 2nd. Nonunion of the clavicle. J Am Med Assoc 1960;172:1006-11. 
[PUBMED] |
| 5. | Eskola A, Vainionpaa S, Myllynen P, Patiala H, Rokkanen P. Outcome of clavicular fracture in 89 patients. Arch Orthop Trauma Surg 1986;105:337-8. 
|
| 6. | Robinson CM. Fractures of clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998;80:476-84. 
[PUBMED] [FULLTEXT] |
| 7. | Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am 2007;89:1-10. 
|
| 8. | Drosdowech DS, Manwell SE, Ferreira LM, Goel DP, Faber KJ, Johnson JA. Biomechanical analysis of middle third fractures of the clavicle. J Orthop Trauma 2011;25:39-43. 
[PUBMED] [FULLTEXT] |
| 9. | Renfree T, Conrad B, Wright T. Biomechanical comparison of contemporary clavicle fixation devices. J Hand Surg Am 2010;35:639-44. 
[PUBMED] [FULLTEXT] |
| 10. | Millett PJ, Hurst JM, Horan MP, Hawkins RJ. Complications of clavicle fractures treated with intramedullary fixation. J Shoulder Elbow Surg 2011;20:86-91. 
[PUBMED] [FULLTEXT] |
| 11. | Thyagarajan SD, Day M, Dent C, Williams R, Evans R. Treatment of mid-shaft clavicle fractures: A comparative study. Int J Shoulder Surg 2009;3:23-7. 
[PUBMED]  |
| 12. | Bostman O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma 1997;43:778-83. 
|
| 13. | Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of clavicle gives poor results. J Bone Joint Surg Br 1997;79:537-9. 
[PUBMED] [FULLTEXT] |
| 14. | Nabil AE, Anis OM, Maamun D. Open reduction and internal fixation with bone grafting of clavicular nonunion. J Trauma 1997;42:701-4. 
|
| 15. | Shen, WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury 1999;30:497-500. 
|
| 16. | Verborgt O, Pittoors K, Van Glabbeek F, Declercq G, Nuyts R, Somville J. Plate fixation of middle-third clavicle fractures in the semi-professional athlete. Acta Orthop Belg 2005;71:17-21. 
[PUBMED] |
| 17. | Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD; Evidence-Based Orthopaedic Trauma Working Group. Treatment of Acute midshaft clavicle fractures: Systematic review of 2144 fractures: On behalf of the evidence-based Orthopaedic Trauma Working Group. J Orthop Trauma 2005;19:504-7. 
[PUBMED] [FULLTEXT] |
| 18. | Venkatachalam S, Packer G, Sivaji C, Skipton A. Plating of fresh displaced midshaft clavicular fractures. Internet J Orthop Surg 2007;5:1. 
|
[Figure 1]
[Table 1], [Table 2], [Table 3]
| This article has been cited by | | 1 |
Locking plate osteosynthesis of clavicle fractures: complication and reoperation rates in one hundred and five consecutive cases |
|
| Marie Fridberg,Ilija Ban,Zaid Issa,Michael Krasheninnikoff,Anders Troelsen | | International Orthopaedics. 2013; 37(4): 689 | | [Pubmed] | [DOI] | | | 2 |
Technical complications during removal of locking screws from locking compression plates: a prospective multicenter study |
|
| N. Schwarz,S. Euler,M. Schlittler,T. Ulbing,P. Wilhelm,G. Fronhöfer,M. Irnstorfer | | European Journal of Trauma and Emergency Surgery. 2013; 39(4): 339 | | [Pubmed] | [DOI] | |
|
 |
|
