| |


 |
| Year : 2011 | Volume
: 5
| Issue : 4 | Page : 95-100 |
|
|
|
|
|
ORIGINAL ARTICLE Latissimus dorsi tendon transfers for rotator cuff deficiency
James Donaldson, Adam Pandit, Ali Noorani, Tania Douglas, Mark Falworth, Simon Lambert
The Shoulder and Elbow Unit, Royal National Orthopaedic Hospital, Stanmore, HA7 4LP, United Kingdom
Correspondence Address:
James Donaldson
35 Ripplevale Grove, Islington, London, N1 1HS
United Kingdom
 Source of Support: None, Conflict of Interest: None  | 3 |
DOI: 10.4103/0973-6042.91002

|
|
|
|
| Date of Web Publication | 20-Dec-2011 |
 Abstract Abstract | | |
Purpose : Latissimus dorsi tendon transfers are increasingly being used around the shoulder. We aim to assess any improvement in pain and function following a latissimus dorsi tendon transfer for massive, irreparable postero-superior cuff deficiency.
Materials and Methods : At our institution, between 1996 and 2009, 38 latissimus dorsi tendon transfer procedures were performed. Sixteen of these were for massive irreparable rotator cuff deficiency associated with pain and impaired function. All patients were evaluated by means of interview or postal questionnaire and case note review. Pain and function were assessed using the Stanmore percentage of normal shoulder assessment (SPONSA) score, visual analogue scale and Oxford Shoulder Score. Forward elevation was also assessed and a significant improvement was thought to correlate with the success of the procedure at stabilizing the humeral head upon elevation.
Results : Mean follow-up time was 70 months. There was a significant reduction in pain on the visual analogue scale from 6.4 to 3.4 (P < 0.05), an improved SPONSA score from 32.5 to 57.5 (P < 0.05), and an improved Oxford Shoulder Score from 40.75 to 29.6 (P < 0.05). Forward elevation improved from 40° preoperatively to 75° postoperatively (P < 0.05).
Conclusion : Our results add to the body of evidence that latissimus dorsi tendon transfers for irreparable postero-superior cuff deficiency in selected patients reduce pain and improve shoulder function in the medium term.
Level of Evidence : Level 4.
Keywords: Latissimus dorsi, tendon transfer, rotator cuff deficiency
How to cite this article:
Donaldson J, Pandit A, Noorani A, Douglas T, Falworth M, Lambert S. Latissimus dorsi tendon transfers for rotator cuff deficiency. Int J Shoulder Surg 2011;5:95-100 |
 Introduction Introduction | |  |
Rotator cuff tears can be associated with severe functional impairment and chronic, disabling pain that does not respond to non-surgical treatment. The most consistent deficit is the loss of the supraspinatus and infraspinatus muscle-tendon-bone continuity (the postero-superior cuff). Tearing of these tendons leads to loss of active external rotation and the inability to stabilize the arm in space. Large tendon tears are associated with fatty infiltration and atrophy of the respective muscles. These changes are irreversible even if direct repairs are structurally successful. [1] Massive, irreparable postero-superior rotator cuff tears are not common and their treatment still remains a source of much controversy.
Most tears that involve two or more tendons can be repaired with good results. In some patients, however, the size of the defect and the quality of the tendon tissue preclude secure repair to bone. In such cases, alternative surgical techniques need to be considered. Both open and arthroscopic debridement has been suggested. Some authors advocate this for pain relief and function, but strength is not restored. [2] Furthermore, the durability of pain relief has been questioned. [3] Tendon allografts and synthetic fabrics have also been used, but without reproducible results. [4] Both local and distant tendon transfer (subscapularis, teres minor, anterior deltoid and trapezius) have been used, but again, with limited success.
Gerber [5] in 1988 introduced the idea of a latissimus dorsi tendon transfer (LDTT) for the treatment of irreparable postero-superior cuff tears. Since then, it has become an established procedure in the treatment of massive rotator cuff tears or as a salvage procedure after failed operative treatments with limited elevation and external rotation. [6],[7]
The underlying principle is to stabilize the humeral head and provide a secure glenohumeral fulcrum around which the deltoid can act and exert its pull on the humerus.
Surgical technique
Principles of tendon transfers around the shoulder are as follows:
- Shoulder elevation is most efficiently performed in the plane of the scapula; tendon transfers to restore shoulder elevation should therefore be performed in the plane of the scapula when possible.
- Tendons transferred to the humeral head (or rotator cuff) in order to bring about rotation are more efficient than transfers to the shaft of the humerus as the humeral head has a greater diameter.
Procedure
The procedure is performed in the lateral decubitus position. A lazy posterior hockey stick incision with lateral thoracic extension is used. The inferior border of deltoid is identified and the plane between this and infraspinatus is then developed. Latissimus dorsi and teres major are identified and elevated on the subscapular pedicle, identifying branches to teres major and the main pedicle to latissimus dorsi, freeing this up into the axilla. Both latissimus dorsi and teres major are detached from the humerus and pedicles defined to each.
Latissimus dorsi is separated from teres major as far as the pedicle allows, for later transfer. The deltoid muscle is split posteriorly and partially detached from the acromion. The latissimus dorsi tendon is reinforced with a non-absorbable whipstitch and passed through a plane between infraspinatus/teres minor and the deltoid muscle to the insertion zone of the infraspinatus and posterior supraspinatus on the posterior humeral head. The arm is held in 90° elevation and maximal external rotation. The tendon is then repaired with transosseous sutures to the greater tuberosity. If there is any remaining cuff, it can be repaired end-to-side to the LDTT. Teres major can be used to augment the LDTT if it is neither long nor broad enough. The arm is taken through a range of motion exercises to assess the integrity of the repair.
Deltoid is repaired with a transosseous suture. A drain is placed if needed and the wound closed in layers. A shoulder spica is applied whilst the patient is still under general anesthesia (30° elevation, 30° abduction and neutral rotation), which is then worn continuously for 6-8 weeks.
Rehabilitation
The rehabilitation program at our institution is milestone driven. The time frames mentioned below are averages and may vary from patient to patient.
Phase one: This phase involves resting the operated limb in a position where the transferred tendon can heal without tension. The decision whether to use a brace or plaster spica is made by the surgeon at the time of surgery and is based on the integrity of the graft, the size of the patient and the anticipated compliance with the immobilization restrictions. The patient remains in a shoulder spica or brace for 6-8 weeks during the acute healing phase. The patient is educated on the anatomy of the shoulder, postoperative restrictions, the anticipated rehabilitation, and their short- and long-term goals are discussed. They are given postural advice and simple exercises.
Phase two: Approximately 8 weeks to 3-9 months: The focus of this phase is to learn to successfully recruit the transfer, achieving simple actions of the limb. At the start of this phase, patients wearing plaster spicas are weaned onto an abduction pillow. The arm can be lowered to waist level for washing and dressing, but the patient is advised to rest with the arm in the support or elsewhere in a similar position. Soft tissue mobilization and gentle stretches are carried out to assist the patient in achieving the ranges required for the initial exercises. With the arm supported in the approximate mid length-tension position (45°-90° scaption and approximately 45° external rotation), the patient is encouraged to recruit the latissimus dorsi, using its "old" action of adduction. This should bring about the "new" action of humeral head centering (often referred to as "snugging") and external rotation. The patient attempts to hold this static position independently. Once this is achieved, the arm is once again positioned in this starting position and the patient learns to eccentrically lower the arm to a position of neutral rotation. The purpose of recruiting eccentrically is an attempt to encourage a normal pattern of movement, in relation to the scapula, humeral head and trunk posture, as opposed to concentrically, which is usually the abnormal pattern of compensatory movement that the patient is familiar with, having pre-operatively reinforced this for months, if not years.
Once the transfer is activating appropriately and movement patterns are normalized, first with the demonstration of eccentric control, and then with concentric control at various supported degrees of scaption, the abduction support is gradually deflated and gentle functional use of the arm at waist level is initiated. Further ranging of the shoulder complex is encouraged at this stage ensuring that activation is not lost as the available range is improved.
The most important concept of the rehabilitation is that of developing neuromuscular control of the muscle in its new role. It is the reorganization at a neurological level that allows the patient to recruit latissimus dorsi as an external rotator and stabilizer of the humeral head rather than as an adductor and internal rotator. Several authors [8],[9],[10] demonstrated that EMG activity present in the transfer during active external rotation was associated with improved outcome, and equally poor EMG activity corresponded with a poor outcome both objectively and subjectively. Therefore, any technique that influences motor learning is beneficial. Surface electromyography biofeedback, functional electrical stimulation, a mirror or motor imagery can be used in conjunction with facilitatory movements, sensory stimulation and verbal feedback. Initially, the new action of latissimus dorsi will require cognitive control but should become more automatic as neuroplasticity occurs. Repetition is key in order to influence cortical representation. [11]
Rehabilitation phase three: Approximately 3-9 months onward: Once the patient can demonstrate control via active external rotation at various supported levels, we know that the centering of the humeral head is taking place, allowing for stability, which in turn allows for anterior deltoid to elevate and posterior deltoid to rotate the arm with any residual cuff and potentially the transfer itself. Therefore, progression is essentially an expansion of the physical repertoire, moving the arm into positions of unsupported rotation and elevation, and the ongoing reinforcement to strive to achieve these movements with automatic recruitment of the latissimus dorsi. The potential outcome for each patient will vary according to the pre-operative function and indications for surgery.
Throughout the rehabilitation phases, in conjunction with specific shoulder exercises, all patients should aim to maintain core and postural control and address all other aspects of the kinetic chain as required to maximize function.
 Materials and Methods Materials and Methods | |  |
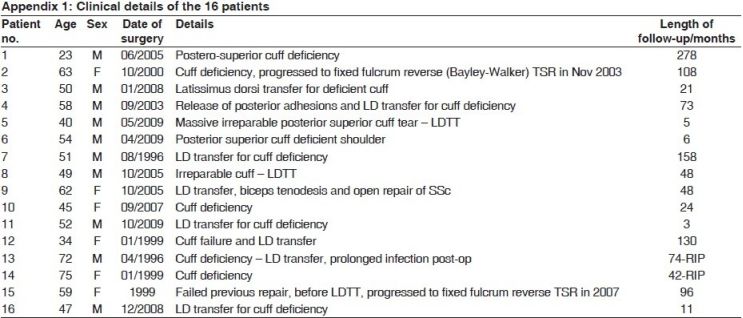
Sixteen patients underwent LDTT for massive irreparable postero-superior rotator cuff deficiency between 1996 and 2009. The indications were a massive rotator cuff tear involving supraspinatus and infraspinatus tendons, confirmed if necessary by magnetic resonance imaging (MRI) or arthroscopy, or a prior failed open repair of a postero-superior rotator cuff tear. All patients had chronic pain, impaired shoulder function with weakness of external rotation or loss of overhead elevation, and an intact subscapularis (in one patient, subscapularis was repaired at the same time as the LDTT (Appendix 1 - patient details).
The average age at the time of surgery was 52 years (range 23-75 years). Patients were evaluated by means of clinical interview, postal questionnaire and case note review. The mean follow-up was 70 months (range 3-278 months).
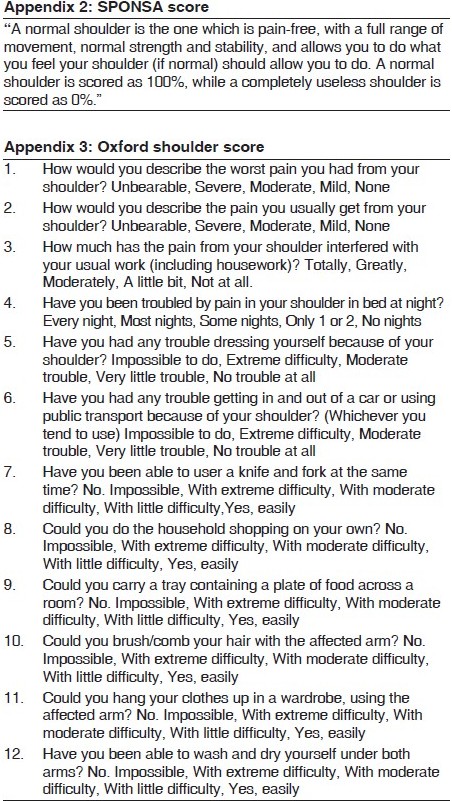
Outcome measures were pain assessed by the visual analogue scale (VAS) from 0 to 10, and function using the Stanmore Percentage of Normal Shoulder Assessment score [12] (SPONSA score - Appendix 2) and the Oxford Shoulder Score [13] (OSS - Appendix 3). Forward elevation (a surrogate for assessing the LDTT's effectiveness in stabilizing the humeral head) was also assessed pre-and postoperatively. Clinical examination by the shoulder and elbow unit doctors and visual inspection was used to measure forward elevation preoperatively in all the patients. Postoperatively, this was ascertained from their last follow-up visit. In those with no recent follow-up (5 of the 16), forward elevation was self-reported with the aid of a questionnaire (3) or by telephone interview and explanation (2). The patients selected the closest approximation of their elevation. We accept the possibility of reporting bias in these five patients.
Results were analyzed using a paired Student's t-test in Microsoft Excel.
 Results Results | |  |
There was a significant reduction in pain from 6.4 to 3.4 (P < 0.05), an improved SPONSA score from 32.5 to 57.5 (P < 0.05), and an improved OSS from 40.75 to 29.6 (P < 0.05). Mean forward elevation, in the 16 patients, improved from 40° preoperatively to 75° postoperatively (to the nearest 5°) [Table 1].
The OSS has been validated in assessing pain and function. Questions 1-4 address pain, questions 5-9 look at function at waist level and questions 10-12 look at function at shoulder level. On further analysis of the OSS results, the greatest improvements can be seen in pain, and function at waist level, which arguably are the functionally more important outcomes following shoulder surgery [Table 2].
There were no significant differences between men and women, although there was a trend toward a greater improvement in forward elevation in men.
The mean follow-up was 70 months (3-278 months). Eleven of the 16 patients had follow-up of over 2 years. There was one postoperative infection, which required a prolonged course of oral antibiotics. Two of the patients progressed to a fixed fulcrum reverse total shoulder replacement for rotator cuff arthropathy - one at 3 years and the other at 8 years post tendon transfer.
 Discussion Discussion | |  |
LDTT to the greater tuberosity has been the most successful tendon transfer procedure for irreparable supraspinatus and infraspinatus tears associated with severe functional impairment and chronic pain. Gerber et al. [14] introduced this idea using a two incision technique - a dorsal incision to mobilize latissimus dorsi and a second, transacromial approach to provide access to the greater tuberosity of the humerus. Others have adopted a single incision technique. [15]
For chronic pain and impaired shoulder function, our results suggest that an LDTT does offer significant improvement. We do acknowledge limitations in our cohort in that five of the patients had less than 2 years follow-up, and therefore may not be completely rehabilitated (these patients may indeed improve further with time, but this cannot be concluded from the existing data). In addition, self-reported data collection may be subjected to bias.
Greatest improvements in the OSS were seen in the pain and functional waist level questions compared to the functional questions at shoulder level. An improvement in forward elevation was also identified, suggesting that LDTT is working effectively in its new role to stabilize the humeral head as the action of the deltoid elevates the arm.
In his original series, Gerber [16] published the results of 16 patients with a mean follow-up of 33 months. His patients regained 73% of an age- and gender-adjusted constant score. He stressed the importance of an intact subscapularis - its deficiency was directly related to poorer results.
In a larger series published in 2006, Gerber et al. [17] reviewed 67 patients with 69 cuff-deficient shoulders who were managed with an LDTT. Significant improvements were seen with an increase in subjective shoulder value from 28.1 to 66%, Constant and Murley score from 55 to 73%, range of movement and strength. Again, in keeping with Gerber's previous work and other studies, those with a subscapularis deficiency performed worse and the value of only an LDTT in these patients was questioned.
Smaller studies have shown similar results. Aoki et al. [18] published the results of 12 LDTTs with a follow-up of 35.6 months. Eight patients were reported to have excellent or good results and four patients had fair or poor results. Miniaci and MacLeod [19] followed up 17 patients who were managed with an LDTT as a salvage procedure; 14 gained significant pain relief and an improvement in shoulder function and 3 were classed as a failure with ongoing pain and impaired function.
Some authors advocate the use of both the teres major tendon and the latissimus dorsi tendon in order to increase the amount of tendon tissue available for coverage of the postero-superior cuff footprint. This combined transfer has been used extensively for the treatment of Erb's palsy in the pediatric population and is supported by biomechanical studies. [20],[21],[22]
An anatomical study by Herzberg et al. [23] showed that re-insertion of the latissimus dorsi flap at the site of insertion of infraspinatus gave superior rotational movement compared with that of insertion at other sites.
Several authors have tried to identify the factors affecting the outcome. Iannotti et al. [24] found female sex, generalized muscle weakness and poor preoperative shoulder function to be negative predictors of outcome. They also noted that poor electrical activity of the LDTT at follow-up was a negative factor. Warner and Parsons [25] found that better results were achieved in primary LDTT compared to salvage procedures. Although others have noted a similar finding with better ultimate outcomes in primary LDTT procedures, [26] comparable increases in pain relief and function are still seen in revision or salvage procedures. [27]
Moursey et al. [28] showed superior results with a modified tendon transfer technique. They harvested the tendon with a small piece of bone, which then allowed bone-to-bone transosseous fixation. Less ruptures were seen on MRI when assessing the integrity of the transfer at follow-up. This correlated with an improvement in patient satisfaction.
 Conclusion Conclusion | |  |
LDTTs significantly improve pain and function in selected patients with postero-superior rotator cuff deficiency. It is successful when primary repair of the rotator cuff proves impossible, or as a salvage procedure. The procedure is reproducible and in the medium term has good results. A significant improvement in all outcome measures was observed in our series, with only one superficial wound infection complication. The authors believe LDTT should not be forgotten as an alternative in the management of massive rotator cuff deficiency, rather than opting for a reverse polarity total shoulder replacement in the non-arthritic shoulder.
 References References | |  |
| 1. | Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy 2004;20:22-33. 
[PUBMED] [FULLTEXT] |
| 2. | Rockwood C, Williams G, Burkhead W. Debridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am 1995;77:857-66. 
|
| 3. | Melillo A, Savoie F, Field L. Massive rotator cuff tears: Debridement versus repair. Orthop Clin North America 1997;28:117-24. 
|
| 4. | Ozaki J, Fujimoto S, Masuhara K, Tamia S, Yoshimoto S. Reconstruction of chronic massive rotator cuff tears with synthetic materials. Clin Orthop 1986;202:173-83. 
|
| 5. | Gerber C, Vinh TS, Hertel R, Hess CW. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff: A preliminary report. Clin Orthop 1988;232:51-61. 
[PUBMED] |
| 6. | Gerber C. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin Orthop Rel Res 1992;275:152-60. 
|
| 7. | Gerber C, Maquieira G, Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am 2006;88:113-20. 
[PUBMED] [FULLTEXT] |
| 8. | Aoki M, Okamura K, Fukuushima S, Takahashi T, Ogino T. Transfer of latissimus dorsi for irreparable rotator cuff tears. J Bone Joint Surg Br 1996;78:761-6. 
|
| 9. | Iannotti JP, Hennigan S, Herzog R, Kella S, Kelley M, Leggin B, et al. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears: Factors affecting outcome. J Bone Joint Surg Am 2006;88:342-8. 
[PUBMED] [FULLTEXT] |
| 10. | Irlenbusch U, Bernsdorf M, Born S, Gansen HK, Lorenz U. Electromyographic analysis of muscle function after latissimus dorsi tendon transfer. J Shoulder Elbow Surg 2008;17:492-9. 
[PUBMED] [FULLTEXT] |
| 11. | Kleim J, Barbay S, Nudo RJ. Functional reorganisation of the rat motor cortex following motor skill learning. J Neurophysiol 1998;80:3321-5. 
|
| 12. | Noorani A, Malone A, Jaggi A, Lambert SM, Bayley JIL. Validation of the stanmore percentage of normal shoulder assessment score. EFORT proceedings 2007. 
|
| 13. | Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg (Br) 1996;78:593-600. 
[PUBMED] [FULLTEXT] |
| 14. | Gerber C, Vinh TS, Hertel R, Hess CW. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff: A preliminary report. Clin Orthop 1988;232:51-61. 
[PUBMED] |
| 15. | Habermayer P, Magosch P, Rudolph T, Lichtenberg S, Liem D. Transfer of the tendon of latissimus dorsi for the treatment of massive tears of the rotator cuff: A new single incision technique. J Bone Joint Surg B 2006;88:208-12. 
|
| 16. | Gerber C. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin Orthop Rel Res 1992;275:152-60. 
|
| 17. | Gerber C, Maquieira G, Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am 2006;88:113-20. 
[PUBMED] [FULLTEXT] |
| 18. | Aoki M, Okamura K, Fukuushima S, Takahashi T, Ogino T. Transfer of latissimus dorsi for irreparable rotator cuff tears. J Bone Joint Surg Br 1996;78:761-6. 
|
| 19. | Miniaci A, MacLeoad M. Transfer of the latissimus dorsi muscle after failed repair of a massive tear of the rotator cuff: A two to five year review. J Bone Joint Surg Am 1999;81:1120-7. 
|
| 20. | Edwards TB, Baghian S, Faust DC, Willis RB. Results of latissimus dorsi and teres major transfer to the rotator cuff in the treatment of Erb's palsy. J Pediatr Orthop 2000;20:375-9. 
[PUBMED] [FULLTEXT] |
| 21. | Magermans DJ, Chadwick EK, Veeger HE, Van der Helm FC, Rozing PM. Biomechanical analysis of tendon transfers for massive rotator cuff tears. Clin BIomech 2004;19:350-7. 
|
| 22. | L'Episcopo JB. Tendon transplantation in obstetric paralysis. Am J Surg 1934;25:122-5. 
|
| 23. | Herzberg G, Schoierer O, Berthonnaud E, Medda N, Dimnet J. 3D mdelization of latissimus dorsi transfer in rotator cuff surgery: what point of fixation on the humeral head. 1 st Closed Meeting European Society Surgery Shoulder Elbow 2001. 
|
| 24. | Iannotti JP, Hennigan S, Herzog R, Kella S, Kelley M, Leggin B, et al. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J Bone Joint Surg Am 2006;88:342-8. 
[PUBMED] [FULLTEXT] |
| 25. | Warner JJ, Parsons IM. Latissimus dorsi tendon transfer: A comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg 2001;10:514-21. 
|
| 26. | Irlenbusch U, Bensdorf M, Gansen HK, Lorenz U. Latissimus Dorsi transfer in case of irreparable rotator cuff tear: A comparative analysis of primary and failed rotator cuff surgery, independent of deficiency grade and additional lesions. Z Orthop Ihre Grenzgeb 2003;141:650-6. 
[PUBMED] [FULLTEXT] |
| 27. | Gerber C, Maquieira G, Espinosa N. Latissimus Dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am 2006;88:113-20. 
[PUBMED] [FULLTEXT] |
| 28. | Moursey M, Forstner R, Koller H, Resch H, Tauber M. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: A modified technique to improve tendon transfer integrity. J Bone Joint Surg Am 2009;91:1924-31. 
|
[Table 1], [Table 2]
| This article has been cited by | | 1 |
Latissimus Dorsi Tendon Transfer for Irreparable Rotator Cuff Tears: A Modified Technique Using Arthroscopy |
|
| Diego Villacis,Jarrad Merriman,Karlton Wong,George F. Rick Hatch | | Arthroscopy Techniques. 2013; 2(1): e27 | | [Pubmed] | [DOI] | | | 2 |
Latissimus Dorsi Tendon Transfer for Irreparable Rotator Cuff Tears: A Modified Technique Using Arthroscopy |
|
| Villacis, D. and Merriman, J. and Wong, K. and Rick Hatch, G.F. | | Arthroscopy Techniques. 2013; 2(1): e27-e30 | | [Pubmed] | |
|
 |
|
