| |


 |
| Year : 2012 | Volume
: 6
| Issue : 4 | Page : 126-129 |
|
|
|
|
|
CASE REPORT Locking plates for displaced fractures of the lateral end of clavicle: Potential pitfalls
Soha Sajid1, Ross Fawdington2, Maneesh Sinha1
1 Department of Trauma and Orthopaedics, Russells Hall Hospital, Dudley, United Kingdom
2 Department of Trauma and Orthopaedics, University Hospital of North Staffordshire, Stoke-on-Trent, United Kingdom
Correspondence Address:
Soha Sajid
Trauma and Orthopaedic Department, Russells Hall Hospital, Dudley Group of Hospitals, Dudley, DY1 2HQ
United Kingdom
 Source of Support: None, Conflict of Interest: None  | 5 |
DOI: 10.4103/0973-6042.106226

|
|
|
|
| Date of Web Publication | 18-Jan-2013 |
 Abstract Abstract | | |
Roughly a quarter of all clavicle fractures occur at the lateral end. Displaced fractures of the lateral clavicle have a higher rate of nonunion. The management of fractures of the lateral clavicle remains controversial. Open reduction internal fixation with a superiorly placed locking plate is a recently developed technique. However, there are no randomized controlled trials to evaluate the efficacy of this procedure. We present a series of four cases which highlight the technical drawbacks with this method of fixation for lateral clavicle fractures. Two cases show that failure of the plate to negate the displacing forces at the fracture site can lead to plate pullout. Two cases illustrate an unusual complication of an iatrogenic injury to the acromioclavicular joint capsule which led to joint instability and dislocation. We advise caution in using this method of fixation. Recent studies have described the success of lateral clavicle locking plate fixation augmented with a coracoclavicular sling. This augmentation accounts for the displacing forces at the fracture site. We would recommend that when performing lateral clavicle locking plate fixation, it should be reinforced with a coracoclavicular sling to prevent plate failure by lateral screw pullout.
Keywords: Lateral clavicle fracture, locking plate, screw pullout
How to cite this article:
Sajid S, Fawdington R, Sinha M. Locking plates for displaced fractures of the lateral end of clavicle: Potential pitfalls. Int J Shoulder Surg 2012;6:126-9 |
 Introduction Introduction | |  |
Fractures of the clavicle are common injuries with an incidence of 29 per 100,000 population per year. [1] Almost a quarter of clavicle fractures occur at the lateral end. [2],[3] While minimally displaced fractures of the lateral end of the clavicle can be managed nonoperatively with good clinical outcome, displaced fractures of the lateral end of the clavicle have a higher rate of nonunion. [1],[3],[4] Therefore operative management is preferred for most displaced fractures. [1],[2] However, the optimum method of fixation remains a subject of controversy. [2],[3]
The use of a precontoured superiorly placed locking plate and screws, for the lateral end of the clavicle, is a recent development. [5],[6] It is advocated as a satisfactory technique for fixation of displaced fractures of the lateral clavicle due to good results seen with this fixation concept in other areas. [5] We report a series of four cases that highlight technical shortcomings of this relatively new technique and present a short review of the existing literature.
 Case Reports Case Reports | |  |
Case 1
A 58-year-old right-hand dominant male presented with painful nonunion of a Neer type II left lateral clavicle fracture in February 2010. His main complaint was of pain and clicking, particularly on heavy lifting. He had no significant past medical history but he was a heavy smoker. (Radiographs in [Figure 1]a and b show the left clavicle after the initial injury sustained in July 2009 and symptomatic non-union in February 2010 respectively).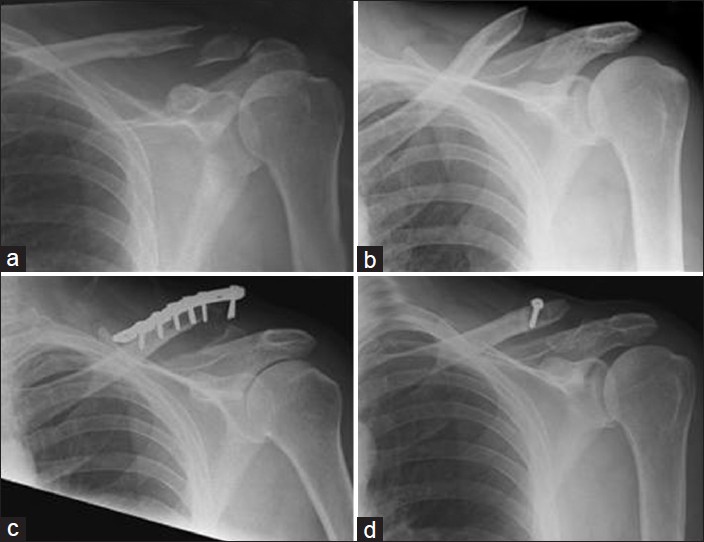 | Figure 1: A 58-year-old male with a nonunion of a left lateral clavicle fracture. (a) Acute lateral clavicle fracture. (b) Nonunion of lateral clavicle fracture. (c) Radiographs at 6 weeks showing plate pullout. (d) Revision using stabilization with a coraco-clavicular sling
Click here to view |
The patient underwent surgical intervention with open reduction and internal fixation (ORIF) using a lateral clavicle locking plate (Periloc, Smith and Nephew) and iliac crest bone grafting of the left lateral clavicle in March 2010. The procedure was performed through a transverse incision. The nonunion site was debrided. Bone graft from the iliac crest was inserted and the fixation was performed using the locking plate; five of the eight lateral 2.7 millimeter (mm) screws allowed by the plate were inserted, though the lateral fragment of the clavicle was only large enough to allow insertion of two screws. The patient was discharged with the arm immobilized in a sling. Outpatient physiotherapy was arranged and instructions were given to perform pendular exercises within a pain free range. Flexion and abduction were restricted for the first 6 weeks.
Follow-up radiographs 6 weeks later showed that the plate had failed and pulled out of the lateral fragment [Figure 1]c. The plate caused significant tenting of the skin and therefore removal of metalwork was done. The nonunion was managed by stabilizing the medial fragment with a coracoclavicular sling, fixed with a 3.5 mm screw and washer.
When reviewed 8 weeks postoperatively, the patient had an Oxford Shoulder Score (OSS) of 28. There was no pain or instability at the site of the fracture. At the last review in December 2011, the patient had an asymptomatic nonunion with no shoulder pain, a full range of movement, and an OSS of 48 [Figure 1]d.
Case 2
A 43-year-old right hand dominant male sustained an isolated fracture of the left lateral clavicle after a motorcycle accident in September 2009 [Figure 2]a. The patient had ORIF using a lateral clavicle locking plate (Periloc, Smith and Nephew) to stabilize the fracture 1 week later [Figure 2]b.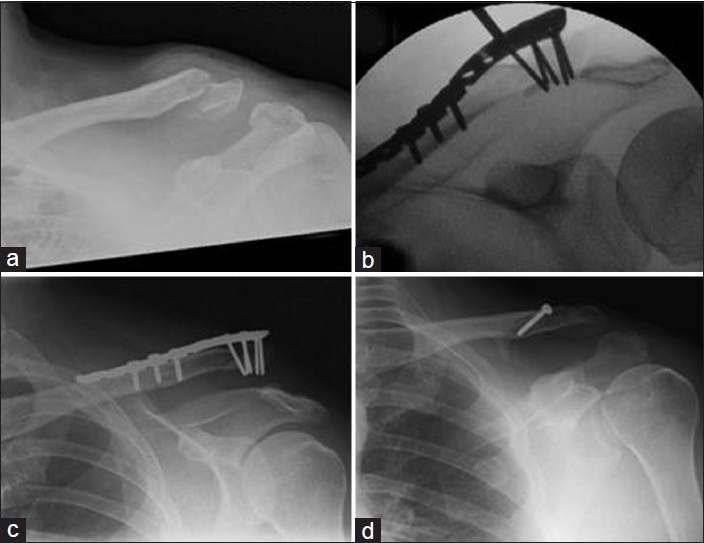 | Figure 2: A 43-year-old male with a left lateral clavicle fracture, sustained in a motorbike accident. (a) Acute lateral clavicle fracture. (b) Intra-op fluoroscopic image showing fracture reduction and fixation with a superiorly placed locking plate. (c) Follow-up radiograph showing AC joint dislocation. (d) Follow-up radiograph showing stabilization with a coraco-clavicular sling
Click here to view |
Four weeks later the patient had a good range of movement but had a prominence over the lateral clavicle. Radiographs showed that the fracture was satisfactorily reduced but the acromioclavicular (AC) joint had subluxed. Radiographs taken on subsequent follow-up appointments showed that although the fracture had healed, the AC joint subluxation progressed to a dislocation [Figure 2]c. The patient complained of ongoing shoulder pain and prominence of the lateral end of the clavicle.
In November 2010, the patient underwent removal of metalwork and stabilization of the AC joint. Intraoperative findings showed that the fracture had united but there was a Rockwood grade III dislocation of the AC joint. The AC joint was stabilized using a coracoclavicular sling [Figure 2]d.
Six weeks later the pain had improved. The range of movement was limited and the patient was referred for physiotherapy. Six months after the procedure, the patient had a full range of movement. However, the patient continued to experience some discomfort when lying on the left side and on heavy lifting. The OSS in December 2011 was 38.
Case 3
A 48-year-old right-hand dominant male sustained a lateral clavicle fracture in December 2011 after landing heavily on his left shoulder while playing rugby. Initial radiographs demonstrated that it was displaced [Figure 3]a. He underwent ORIF with a lateral clavicle locking compression plate system (LCP, Synthes). Fluoroscopic imaging demonstrated a satisfactory reduction [Figure 3]b. Postoperatively he was discharged home with a poly-sling and advised to keep the arm immobilized until review in clinic 2 weeks later.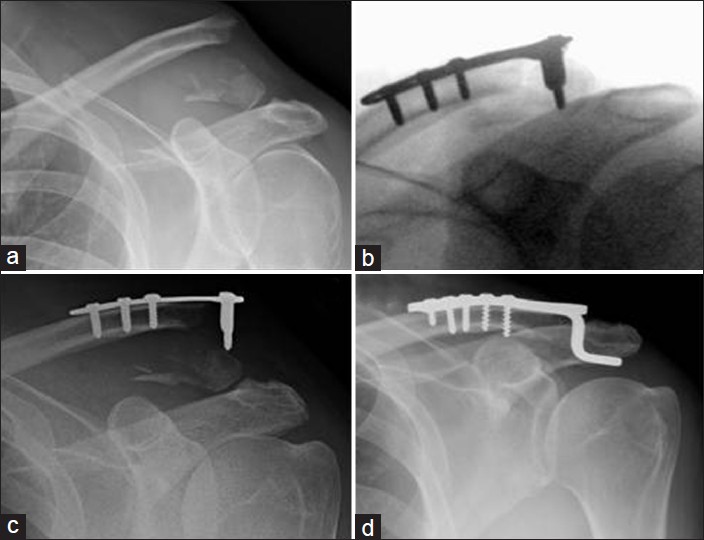 | Figure 3: A 48-year-old male with a left clavicle fracture sustained playing rugby. (a) Acute lateral clavicle fracture. Although the ligaments have not ruptured, they have avulsed the inferior aspect of the clavicle and are therefore de-functioned. (b) Intra-op fluoroscopic image showing satisfactory reduction. (c) Follow-up radiograph showing plate pullout. (d) Revision with hook plate
Click here to view |
The patient returned within 3 days of the surgery complaining of increasing pain and prominence over the lateral clavicle. A radiograph demonstrated that the screws had pulled out of the lateral fragment [Figure 3]c. He then underwent revision surgery and the locking plate was replaced with a hook plate [Figure 3]d. Postoperatively he made an uneventful recovery. Eight weeks after the revision surgery his OSS was 22.
Case 4
A 38-year-old right-hand dominant female fractured her right lateral clavicle when she slipped on wet patio decking [Figure 4]a. Within a week of the injury, she had ORIF of her right clavicle in February 2012 using a Synthes Small Fragment Locking Compression Plate System [Figure 4]b. The postoperative radiographs showed subluxation of the AC joint [Figure 4]c. Her OSS 4 weeks after surgery was 13 [Figure 4]d.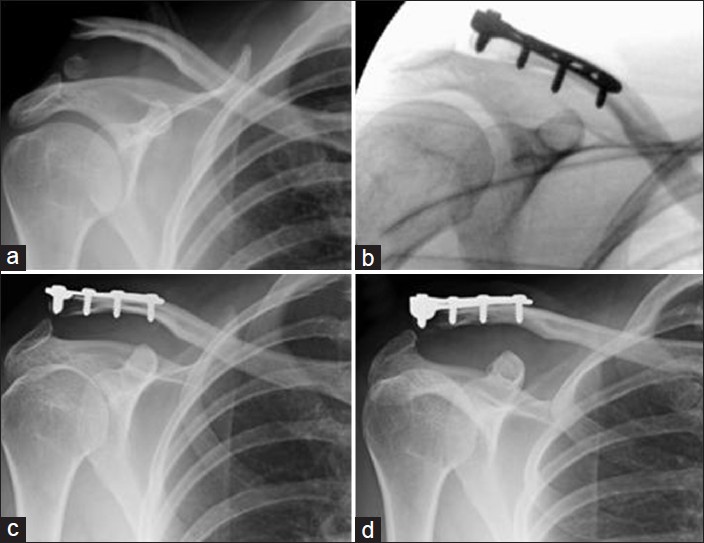 | Figure 4: A 38-year-old female with a right clavicle fracture from a fall on patio decking. (a) Acute lateral clavicle fracture. (b) Intra-op fluoroscopic image showing satisfactory reduction. (c) Two-week follow-up radiograph showing AC joint subluxation. (d) Four-week follow-up radiograph showing no further progression of AC joint subluxation
Click here to view |
 Discussion Discussion | |  |
Management of displaced fractures of the lateral end of the clavicle remains controversial. [2],[3] Neer type 2 and Edinburgh type 3B fractures of the lateral end of clavicle are known to be unstable and have a higher rate of nonunion. [1],[3],[4] It is important to remember that nonoperative management of displaced fractures can achieve acceptable medium term functional results in the middle aged and elderly population despite higher rates of nonunion. [2],[6] However younger patients with greater functional demands are more likely to have ongoing symptoms and require surgery. [2]
A number of surgical interventions for displaced fractures of the lateral end of the clavicle have been described including the following [3],[6] :
Coracoclavicular screws
Hook plates
Suture and sling
Stabilisation with Kirschner wires and tension band wiring
Intramedullary fixation.
However, there have been no randomized controlled trials to evaluate the outcome of these operative interventions. [3],[6]
Fixation of fractures of the lateral clavicle with locking plates is a relatively new technique. [5],[6] This mode of fixation is an extension of the fixed angle, locking screws principle, which has been used in other fractures, most notably fractures of the proximal humerus and distal radius. Although several implant manufacturers have recently introduced locking plates into the market for lateral clavicle fractures, we do not know of any rigorous evaluation of the technique reported in the English literature. A review appraising the different modalities of treatment had proportionally small number of studies which had assessed interfragmentary fixation. [6] This illustrates our point that more research into the use of this technique is required.
We think that it is important to highlight the technical shortcomings of the locking plates for lateral clavicle fixation that are demonstrated by these four cases. Two cases illustrate the complication of plate failure due to a fundamental failure of the technique to negate the displacement forces at the fracture site. The first case shows that the distal fragment can be small and multifragmentary. Therefore, despite fixation using a plate that can allow up to eight lateral 2.7 mm screws, only two of these lateral screws could be fixed into the lateral bony fragment.
Locking plates are fixed angle constructs which have greater resistance to screw pullout. [7] However, this concept does not take into account the significant displacing forces acting at the lateral end of the clavicle. The forces causing clavicle displacement are the weight of the arm, the pull of pectoralis major, pectoralis minor and latissimus dorsi muscles, scapula rotation, and the pull of the sternocleidomastoid muscle. [4],[8] A locking plate placed superiorly over the lateral end of the clavicle does not adequately neutralize all the forces acting at the fracture site, which act predominantly to pull the lateral fragment inferiorly.
The second case and more recently the fourth case illustrate an unusual complication and we believe that the problem may be iatrogenic. The lateral fragment of the fractured clavicle is often small and multifragmentary. Accurate plate placement and adequate fixation with the locking screws on the lateral end can be technically difficult. This technical difficulty has led to the lateral fragment being exposed up to the AC joint and iatrogenic injury to the joint capsule with resultant instability of the joint. Consequently there is displacement at the AC joint leading to subluxation and dislocation.
We accept that this is a small case series and that our patients have had varying follow-up time. However, all the cases demonstrate early complications of this fixation. We also accept that the patients in this series have had surgery after varying duration of time, particularly in the case of the first patient who had ORIF for nonunion. However, the options for fixation were the same as for an acute fracture. Also, this case illustrates early complications for this mode of fixation and our point that it should be used with caution.
In a systematic review of different modes of fixation it was found that rates of nonunion are similar between each mode of fixation. [6] It was also found that the highest rate of complications (excluding nonunion) was encountered with using hook plates and the lowest rate of complication was seen with using intramedullary fixation and coracoclavicular stabilisation. [6] Recent studies reporting the results of lateral clavicle locking plates have almost universally described the use of a coracoclavicular sling or coracoclavicular screw to augment locking plate fixation. [5],[9],[10] This "belt and braces" approach to the locking plate fixation technique reinforces our assertion that the plate itself does little to counteract the displacement forces at the fracture site.
Alternative methods of fixation described include the use of tension band suturing and temporary fixation using Kirschner wires. [11] Though it was a relatively small cohort study, good outcome and minimal complications were reported for this technique, which requires minimal incision and dissection and provides stable fixation of the fracture. [11] Another method of fixation is open reduction and endobutton fixation. [12] This technique allows reduction and internal fixation of the fracture using sutures that pass through an endobutton placed in the clavicle and coracoid process and has shown good short and medium term outcomes. [12] We believe that such techniques must be considered as they can better neutralize the forces acting at the fracture site as described by Neer. [4]
 Conclusion Conclusion | |  |
This case series highlights the potential complications that can occur after ORIF of lateral clavicle fractures with locking plates. Management of lateral clavicle fractures remains controversial and for this reason a number of different techniques have been used to achieve fixation of such fractures. Several manufacturers have introduced precontoured locking plates and advocate the use of this technique for fixation of lateral clavicle fractures. However, we would advise caution with the use of this technique until larger studies, including biomechanical testing has been done to evaluate them.
Care should be taken when using a lateral clavicle locking plate particularly when the lateral fragment is small and comminuted, as in Edinburgh Type 3B fractures. We recommend that if a locking plate is used to fix such fractures, augmenting the fixation with a coracoclavicular sling that helps to neutralize the distracting forces at the fracture site must always be considered.
 References References | |  |
| 1. | Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998;80:476-84. 
[PUBMED] |
| 2. | Robinson CM, Cairns DA. Primary non-operative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am 2004;86-A: 778-82. 
[PUBMED] |
| 3. | Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am 2009;91:447-60. 
[PUBMED] |
| 4. | Neer CS 2 nd . Fractures of the distal third of the clavicle. Clin Orthop Relat Res 1968;58:43-50. 
|
| 5. | Andersen JR, Willis MP, Nelson R, Mighell MA. Precontoured superior locked plating of distal clavicle fractures: A new strategy. Clin Orthop Relat Res 2011;469:3344-50. 
[PUBMED] |
| 6. | Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: A systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg 2011;131:525-33. 
[PUBMED] |
| 7. | Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma 2004;18:488-93. 
[PUBMED] |
| 8. | Post M. Current concepts in the treatment of fractures of the clavicle. Clin Orthop Relat Res 1989;245:89-101. 
[PUBMED] |
| 9. | Largo RD, Rudin MA, Hotz TK, Valderrabano V, Käch KK. Anatomic reconstruction of unstable lateral clavicular fractures. J Trauma 2011;71:1348-51. 
|
| 10. | Klein SM, Badman BL, Keating CJ, Devinney DS, Frankle MA, Mighell MA. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg 2010;19:1049-55. 
[PUBMED] |
| 11. | Rijal L, Sagar G, Joshi A, Joshi KN. Modified tension band for displaced type 2 lateral end clavicle fractures. Int Orthop 2012;36:1417-22, 
|
| 12. | Robinson CM, Akhtar MA, Jenkins PJ, Sharpe T, Ray A, Olabi B. Open reduction and endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br. 2010;92:811-6. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
| This article has been cited by | | 1 |
Temporary Sternoclavicular Plating for an Unusual Double Clavicle Fracture (Medial Nonunion, Lateral Acute) Complicated by an Intraoperative Pneumothorax |
|
| John G. Skedros,Alex N. Knight,Chad S. Mears,Tanner D. Langston | | Case Reports in Orthopedics. 2014; 2014: 1 | | [Pubmed] | [DOI] | | | 2 |
Die laterale Klavikulafraktur – Grundlagen, OP-Indikationen, Versorgungstechniken |
|
| Benedikt Schliemann,Sarah Breiter,Christina Theisen,Kristian N. Schneider,Clemens Kösters,Michael J. Raschke,André Weimann | | Obere Extremität. 2014; | | [Pubmed] | [DOI] | | | 3 |
Outcome of arthroscopic treatment for displaced lateral clavicle fractures using a double button device |
|
| Philippe Loriaut,Pierre-Emmanuel Moreau,Benjamin Dallaudière,Alexandre Pélissier,Hoang Duc Vu,Philippe Massin,Patrick Boyer | | Knee Surgery, Sports Traumatology, Arthroscopy. 2013; | | [Pubmed] | [DOI] | |
|
 |
|
