| |


 |
| Year : 2013 | Volume
: 7
| Issue : 1 | Page : 19-22 |
|
|
|
|
|
ORIGINAL ARTICLE Ossification of the suprascapular ligament: A risk factor for suprascapular nerve compression?
R Shane Tubbs1, Carl Nechtman1, Anthony V D'Antoni2, Mohammadali M Shoja1, Martin M Mortazavi1, Marios Loukas3, Curtis J Rozzelle1, Robert J Spinner4
1 Section of Pediatric Neurosurgery, Children's Hospital, Birmingham, Alabama, USA
2 Division of Pre clinical Sciences, New York College of Podiatric Medicine, New York, USA
3 Department of Anatomical Sciences, St. George's University, Grenada, West Indies
4 Department of Neurosurgery, Mayo Clinic, Rochester, MN, USA
Correspondence Address:
R Shane Tubbs
JFL Building, Children's Hospital, Birmingham, AL 35233
USA
 Source of Support: None, Conflict of Interest: None  | 7 |
DOI: 10.4103/0973-6042.109882

|
|
|
|
| Date of Web Publication | 2-Apr-2013 |
 Abstract Abstract | | |
Introduction: Entrapment of the suprascapular nerve at the suprascapular notch may be due to an ossified suprascapular ligament. The present study was conducted in order to investigate the incidence of this anomaly and to analyze the resultant bony foramen (foramen scapula) for gross nerve compression.
Materials and Methods: We evaluated 104 human scapulae from 52 adult skeletons for the presence of complete ossification of the suprascapular ligament. When an ossified suprascapular ligament was identified, the diameter of the resultant foramen was measured. Also, the suprascapular regions of 50 adult cadavers (100 sides) were dissected. When an ossified suprascapular ligament was identified, the spinati musculature was evaluated for gross atrophy and the diameters of the resultant foramen scapulae and the suprascapular nerve were measured. Immunohistochemical analysis of the nerve was also performed.
Results: For dry scapular specimens, 5.7% were found to have an ossified suprascapular ligament. The mean diameter of these resultant foramina was 2.6 mm. For cadavers, an ossified suprascapular ligament was identified in 5% of sides. Sections of the suprascapular nerve at the foramen scapulae ranged from 2 to 2.8 mm in diameter. In all cadaveric samples, the suprascapular nerve was grossly compressed (~10-20%) at this site. All nerves demonstrated histologic signs of neural degeneration distal to the site of compression. The presence of these foramina in male cadavers and on right sides was statistically significant.
Conclusions: Based on our study, even in the absence of symptoms, gross compression of the suprascapular nerve exists in cases of an ossified suprascapular ligament. Asymptomatic patients with an ossified suprascapular ligament may warrant additional testing such as electromyography.
Keywords: Anatomy, entrapment, neurosurgery, ossification, peripheral nerve, suprascapular nerve, suprascapular ligament
How to cite this article:
Tubbs R S, Nechtman C, D'Antoni AV, Shoja MM, Mortazavi MM, Loukas M, Rozzelle CJ, Spinner RJ. Ossification of the suprascapular ligament: A risk factor for suprascapular nerve compression?. Int J Shoulder Surg 2013;7:19-22 |
How to cite this URL:
Tubbs R S, Nechtman C, D'Antoni AV, Shoja MM, Mortazavi MM, Loukas M, Rozzelle CJ, Spinner RJ. Ossification of the suprascapular ligament: A risk factor for suprascapular nerve compression?. Int J Shoulder Surg [serial online] 2013 [cited 2016 May 22];7:19-22. Available from: http://www.internationalshoulderjournal.org/text.asp?2013/7/1/19/109882 |
 Introduction Introduction | |  |
The suprascapular nerve receives fibers from C5 and C6 nerve roots with an occasional contribution from the C4 root. Therefore, radiculopathy of these sources must be ruled out in cases of suspected suprascapular nerve entrapment. The suprascapular nerve provides motor innervation to the supraspinatus and infraspinatus muscles, in addition to branches to the coracohumeral and coracoacromial ligaments, subacromial bursa, and the acromioclavicular joint.
Along its course to the spinati muscles, the suprascapular nerve enters the incisura scapulae [suprascapular notch-bound by the upper margin of the scapula inferiorly and the suprascapular ligament, (superior transverse scapular ligament)] superiorly. [1] Rarely, the suprascapular nerve becomes entrapped in this region as first described by Thomas [2] in 1936. Although variations of the morphology of the notch have been analyzed, no correlation has been found between notch type and injury frequency. [3],[4],[5] Ossification of the suprascapular ligament results in a bony foramen (foramen scapulae) through which the suprascapular nerve travels and may result in suprascapular nerve compression. [1],[5],[6]
Patients with suprascapular nerve entrapment often present with pain or weakness of the posterolateral shoulder. [7] Additionally, electromyographic tests may show delayed conduction along the suprascapular nerve. [8] Compression of the suprascapular nerve may be due to multiple etiologies, including congenital abnormalities of the upper edge of the scapula, fractures of the scapula, tumors or ganglion cysts, stretching of the nerve, which is fixed proximally, anomalously formed suprascapular ligaments, and an ossified suprascapular ligament. [9],[10] Sporting activities with a predilection for such compression are gymnastics, tennis, weightlifting, boxing, and baseball pitching. [1] Interestingly, a greater incidence of entrapment of the suprascapular nerve has been found in Brazilians. [5]
The present study aimed to examine the histologic nature of suprascapular nerves in the presence of an ossified suprascapular ligament and to quantitate the area of the resultant bony foramen.
 Materials and Methods Materials and Methods | |  |
One hundred and four human scapulae derived from 52 adult (35 male and 17 female) skeletons were evaluated for the presence of complete ossification of the suprascapular ligament. Age ranges were approximately 30 to 80 years at the time of death. When an ossified suprascapular ligament was identified, the diameter of the resultant foramen was measured with microcalipers (Mitutoyo, Japan). In addition, the suprascapular regions from 50 adult Caucasian embalmed cadavers (100 sides) aged 39 to 78 years (mean 72 years; 30 females and 20 males) at death were dissected from a posterior approach. When an ossified suprascapular ligament was identified, the spinati musculature was evaluated for gross atrophy and the diameter of the resultant foramen scapulae was measured with microcalipers, as well as the diameter of the suprascapular nerve 1 cm before, at, and 1 cm distal to the ossified suprascapular ligament. Histologic analysis (Hematoxylin and Eosin, trichrome, Sevier-Munger silver stain, Luxol fast blue) and neurofilament immunohistochemistry were performed on nerve specimens in this cohort of cadavers with an ossified ligament. For controls, random samples of 10 suprascapular nerve were also harvested and analyzed from cadavers without an ossified suprascapular ligament. Statistical analysis was performed between sides and sexes using Statistica 10.0 for Windows with significance set at P < 0.05. For normalization of data, student's t statistics were applied.
 Results Results | |  |
For dry scapular specimens, 3 suprascapular ligaments (5.7%) were found to be ossified [Figure 1]. These were identified in 1 female (left scapula) and 2 male (right scapulae) specimens. The diameters of the resultant foramina ranged from 1.7 to 4.5 mm (mean 2.6 mm). For cadavers, an ossified suprascapular ligament was identified on five sides (5%). These were seen in 4 male specimens (1 left and 3 right scapulae) and 1 female specimen (right scapula). Suprascapular nerve sections ranged in diameter from 2 to 2.8 mm in diameter at the foramen scapulae. For these cadaveric specimens, the resultant scapular foramina ranged in diameter from 1.8 to 3 mm. In all cadaveric samples found to have an ossified suprascapular ligament, the suprascapular nerve was grossly compressed with a waistband appearance of the nerve at this site (e.g., larger diameter of the nerve pre and post foramen scapulae) by approximately 10 to 20% [Figure 2]. Histologic and immunohistochemistry analyses revealed signs of neural degeneration in all nerve specimens at and distal to the site of suprascapular nerve compression. For example, increased perineurial fibrosis, epineural thickening, hyalinized blood vessels, and focal mucinous degeneration were observed [Figure 3]. Sections of nerve proximal to the compressed site did not show signs of neural degeneration and no sections revealed fiber or myelin loss. Additionally, no control specimen demonstrated signs of neural degeneration.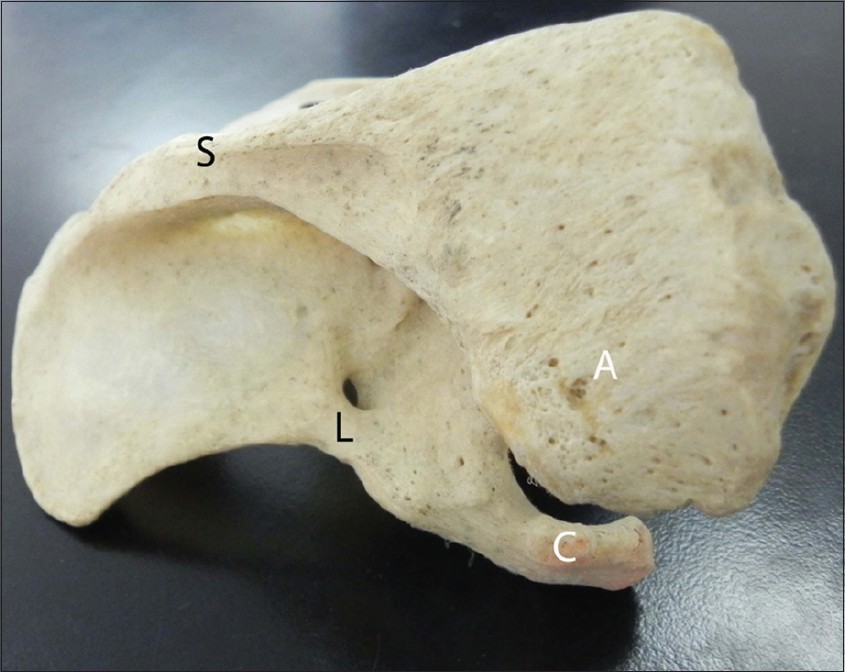 | Figure 1: Example of the left scapula with ossified suprascapular ligament (L) resulting in the foramen scapulae (seen above the L). For reference, note the spine (S), coracoid process (C) and acromion
(A) of the scapula
Click here to view |
 | Figure 2: Schematic drawing illustrating compression of the left suprascapular nerve within the foramen scapulae as found in all of our cadaveric specimens with such a foramen. Note that this is a posterior view
Click here to view |
 | Figure 3: Histologic specimen noting signs of suprascapular nerve compression seen in cadavers with an ossified suprascapular ligament. This section is from the suprascapular nerve distal to the ossified
ligament and notes vascular hyalinization and thickening of the epi and perineuria (Trichrome ×44)
Click here to view |
Although foramen scapulae were more commonly found in male dry scapulae, this did not reach significance. However, the presence of these foramina in male cadavers and on right sides was statistically significant (P < 0.05). No other signs of pathology or previous surgery to the region studied were identified.
 Discussion Discussion | |  |
We did not identify a foramen scapulae bilaterally in any specimen and did not appreciate gross muscle atrophy of the supra or infraspinatus muscles on sides with a foramen scapulae. However, histologic analysis revealed signs of neural degeneration in all nerve specimens distal to the site of compression. It is not known if these individuals experienced symptoms of nerve compression during life such as shoulder pain or spinati muscle weakness. The reason for a greater incidence of these foramina in male specimens is also not clear, but the involvement of right sides more often than left sides may be due to a predilection for right-sided handedness in the general population.
Various classifications have been used to describe the suprascapular notch. Some authors have found no direct correlation between notch type and suprascapular nerve entrapment, but did not take ossification of the suprascapular ligament into consideration. [11] Scapulae with an ossified suprascapular ligament resulting in a foramen scapulae have been classified as type III by Ticker et al. [12] and as type VI by Rengachary et al. [4] and make up approximately 5% of all notch types. [3] This incidence is the same as demonstrated in our cadaveric specimens and comparable to the incidence found in the dry scapular specimens used in our study. For most suprascapular nerve injuries, initial nonsurgical treatment is preferred. [7],[11]
Patients with suprascapular nerve compression may present with a history of symptoms provoked by dominant upper extremity movement. Because the incidence of entrapment of the suprascapular ligament is largely increased with strenuous overhead motion (e.g., volleyball, baseball pitching), it is hypothesized that repetitive overhead motion or trauma contributes to ossification of the ligament.
Treatment for compression of the suprascapular nerve begins with physical therapy aimed at strengthening the rotator cuff musculature. If conservative treatment fails, surgical decompression of the suprascapular ligament is recommended. This may be performed from an anterior, superior, or posterior direction. [8],[13] Generally, a 10-cm incision is made 1 cm proximal and parallel to the spine of the scapula with the trapezius muscle either split or elevated. [8] Arthroscopic decompression may facilitate a more rapid recovery especially when the entrapment is caused solely by the ossified ligament. [7] The subperiosteal technique, according to de Jesus, [13] avoids dissection of the trapezius and supraspinatus muscles and results in less soft tissue damage. Patients found to have an ossified suprascapular ligament may warrant additional testing such as electromyography. [14]
More recent publications on this topic illustrate the continued interest in this variation from various ethnic groups and the potential associated pathology. [15],[16],[17],[18],[19] Additional contributing factors may also be at play such as the fascia of the supraspinatus. [15]
 Conclusions Conclusions | |  |
Based on our study, perhaps even in the absence of symptoms, gross compression of the suprascapular nerve likely exists in cases of an ossified suprascapular ligament. Moreover, neural degeneration of this nerve as seen in our present study may be present.
 References References | |  |
| 1. | Peæina M, Krmpotiæ-Nemaniæ J, Markiewitz A. Tunnel Syndromes. Peripheral Nerve Compression Syndromes 2nd ed. Boca Raton, FL: CRC Press; 1997. 
|
| 2. | Thomas A. La paralysie du muscle sous-épineux. Presse Med 1936;64:1283-4. 
|
| 3. | Dunkelgrun M, Iesaka K, Park SS, Kummer FJ, Zuckerman JD. Interobserver reliability and intraobserver reproducibility in suprascapular notch typing. Bull Hosp Jt Dis 2003;61:118-22. 
|
| 4. | Rengachary SS, Burr D, Lucas S, Brackett CE. Suprascapular entrapment neuropathy: A clinical, anatomical, and comparative study. Part 3: Comparative study. Neurosurgery 1979;5:452-5. 
|
| 5. | Silva JF, Aureliano-Rafael F, Sgrott EA, Silva SF, Babinski MA, Fernandes RMP. High incidence of complete ossification of the superior transverse scapular ligament in Brazilians and its clinical implications. Inter J Morph 2007;25:855-9. 
|
| 6. | Osuagwu F, Imosemi I, Shokunbi M. Complete ossification of the superior traverse scapular ligament in a Nigerian male adult. Inter J Morph 2000;23:121-2. 
|
| 7. | Sergides NN, Nikolopoulos DD, Boukoros E, Papagiannopoulos G. Arthroscopic decompression of an entrapped suprascapular nerve due to an ossified superior transverse scapular ligament: A case report. Cases J 2009;2:8200. 
|
| 8. | Cohen SB, Dines DM, Moorman CT. Familial calcification of the superior transverse scapular ligament causing neuropathy. Clin Orthop Relat Res 1997;334:131-5. 
|
| 9. | Avon M, Weiss S, Fisher B, Dekel S. Bilateral suprascapular nerve entrapment syndrome due to an anomalous transverse scapular ligament. Clin Orthop Relat Res 1988;234:31-3. 
|
| 10. | Gosk J, Urban M, Rutowski R. Entrapment of the suprascapular nerve: Anatomy, etiology, diagnosis, treatment. Ortop Traumatol Rehabil 2007;9:68-74. 
|
| 11. | Cummins CA, Messer TM, Nuber GW. Suprascapular nerve entrapment. J Bone Joint Surg Am 2000;82:415-24. 
|
| 12. | Ticker JB, Djurasovic M, Strauch RJ, April EW, Pollock RG, Flatow EL, et al. The incidence of ganglion cysts and other variations in anatomy along the course of the suprascapular nerve. J Shoulder Elbow Surg 1998;7:472-8. 
|
| 13. | de Jesus RA, Xu J, Ferrari J. Total subperiosteal approach to suprascapular nerve decompression: A technique to relieve entrapment by the superior transverse suprascapular ligament. Plast Reconstr Surg 2009;123:35e-6e. 
|
| 14. | Das S, Suri R, Kapur V. Ossification of superior transverse scapular ligament and its clinical implications. Sultan Qaboos Univ Med J 2007;7:157-60. 
|
| 15. | Duparc F, Coquerel D, Ozeel J, Noyon M, Gerometta A, Michot C. Anatomical basis of the suprascapular nerve entrapment, and clinical relevance of the supraspinatus fascia. Surg Radiol Anat 2010;32:277-84. 
|
| 16. | Sinkeet SR, Awori KO, Odula PO, Ogeng›o JA, Mwachaka PM. The suprascapular notch: Its morphology and distance from the glenoid cavity in a Kenyan population. Folia Morphol 2010;69:241-5. 
|
| 17. | Rengachary SS, Burr D, Lucas S, Hassanein KM, Mohn MP, Matzke H. Suprascapular entrapment neuropathy: A clinical, anatomical, and comparative study. Part 2: Anatomical study. Neurosurgery 1979;5:447-51. 
|
| 18. | Polguj M, Je²drzejewski KS, Podgórski M, Topol M. Correlation between morphometry of the suprascapular notch and anthropometric measurements of the scapula. Folia Morphol 2011;70:109-15. 
|
| 19. | Wang HJ, Chen C, Wu LP, Pan CQ, Zhang WJ, Li YK. Variable morphology of the suprascapular notch: An investigation and quantitative measurements in Chinese population. Clin Anat 2011;24:47-55. 
|
[Figure 1], [Figure 2], [Figure 3]
| This article has been cited by | | 1 |
Suprascapular Notch Asymmetry: A Study on 311 Patients |
|
| Michal Polguj,Marcin Sibinski,Andrzej Grzegorzewski,Piotr Grzelak,Ludomir Stefanczyk,Miroslaw Topol | | BioMed Research International. 2014; 2014: 1 | | [Pubmed] | [DOI] | | | 2 |
Morphological and Radiological Study of Ossified Superior Transverse Scapular Ligament as Potential Risk Factor of Suprascapular Nerve Entrapment |
|
| Michal Polguj,Marcin Sibinski,Andrzej Grzegorzewski,Michal Waszczykowski,Agata Majos,Miroslaw Topol | | BioMed Research International. 2014; 2014: 1 | | [Pubmed] | [DOI] | | | 3 |
The Superior Transverse Scapular Ligament in Fetuses |
|
| José Aderval Aragão,Luiza Neves de Santana Teles,Ana Bárbara de Jesus Chaves,Jéssica Cândida Oliveira Prado,Priscila Soares Pereira,João Gabriel Lima Dantas,Francisco Prado Reis | | Anatomy Research International. 2013; 2013: 1 | | [Pubmed] | [DOI] | |
|
 |
|
