| |


 |
| Year : 2013 | Volume
: 7
| Issue : 1 | Page : 23-27 |
|
|
|
|
|
ORIGINAL ARTICLE Digital photography for assessment of shoulder range of motion: A novel clinical and research tool
Barry J O'Neill1, David O'Briain1, Kieran M Hirpara1, Michelle Shaughnesy2, Elizabeth A Yeatman2, T Kenneth Kaar1
1 Department of Trauma and Orthopaedics, Merlin Park Hospital, Galway, Ireland
2 Department of Physiotherapy, Merlin Park Hospital, Galway, Ireland
Correspondence Address:
Barry J O'Neill
Department of Trauma and Orthopaedics, Merlin Park Hospital, Galway
Ireland
 Source of Support: None, Conflict of Interest: None  | 3 |
DOI: 10.4103/0973-6042.109888

|
|
|
|
| Date of Web Publication | 2-Apr-2013 |
 Abstract Abstract | | |
Purpose: Maintenance of a pain-free functional range of motion is the aim of surgery for shoulder trauma. The aim of this study was to show that the range of motion can be accurately assessed using digital photographs.
Materials and Methods: We reviewed 17 patients who had undergone surgery for shoulder trauma. Each patient's range of motion was assessed by two physicians and two physiotherapists. Digital photographs were taken of each patient at their functional limit. Photographs were assessed by two physicians and two physiotherapists, and by an external physician who had no previous contact with the patients.
Results: Inter-observer and intra-observer reliability trials showed excellent correlation of results. There was no significant difference between observer's results, or between results of physical examination and photographic examination.
Conclusions: Digital photography is a viable adjunct to assessment of range of motion of the shoulder. This has positive implications both clinically, and for shoulder research.
Level of Evidence: Level 3.
Keywords: Assessment, clinical, novel, research, shoulder
How to cite this article:
O'Neill BJ, O'Briain D, Hirpara KM, Shaughnesy M, Yeatman EA, Kaar T K. Digital photography for assessment of shoulder range of motion: A novel clinical and research tool. Int J Shoulder Surg 2013;7:23-7 |
 Introduction Introduction | |  |
The shoulder has the greatest range of motion (ROM) of all human joints, but this mobility is gained at the expense of intrinsic stability. Trauma to the shoulder is common [1],[2],[3],[4] and the aim of treatment is to regain a pain-free functional range of motion (FROM). [5] There are a number of tools designed to measure FROM, [6],[7],[8] but it is commonly measured with simple visual estimation in the out-patient setting. These measurements are documented in clinical records and serial examinations are used to assess clinical progress.
During busy periods trauma clinics can be crowded and waiting times excessive. In areas with a small population spread over a vast geographical area, patients may have to travel long distances for a brief assessment. We hypothesized that patients rehabilitating after shoulder surgery could be assessed locally, and photographic documentation of FROM forwarded to the supervising surgeon. This removes the need for travel, decreases the patient numbers attending clinic, and provides a permanent record of FROM. The aim of our study was to determine whether shoulder FROM could be accurately measured using visual estimation of digital images.
 Materials and Methods Materials and Methods | |  |
We reviewed theatre records at our institution to identify all patients who had undergone a surgical procedure on their shoulder by the senior author (TKK). We reviewed the medical records of all patients to identify those who had undergone shoulder surgery for trauma at our institute between 1999 and 2007. Patients who had undergone elective procedures were excluded, and 111 patients who fulfilled the entry criteria were identified. All the 111 patients were invited to attend for clinical evaluation and estimation of their FROM. Seventeen patients returned for inclusion in the study (15.3%) and no patients were excluded. All subjects who entered the trial gave informed consent for inclusion and for digital photographs to be taken. There were 12 males and 5 females with a mean age of 37 years (range 18-80 years). The presenting pathology and surgical procedure for each patient is given in [Table 1]. Procedures occurred at a mean of 53 months prior to assessment (range 5-90 months).
Two physicians and two physiotherapists (four assessors) visually estimated the maximum range of flexion, abduction, internal rotation, and external rotation (FROM) of 34 shoulders in seventeen patients. Measurements were made in accordance with the recommendations of the European Society for Surgery of the Shoulder and the Elbow (ESSSE), adopted from the system described by Constant and Murley. [9] Each assessor was blinded to the results of the others. Digital photographs were taken of the FROM of the 17 shoulders that had undergone surgery. All photographs were taken by a single physician using a Canon IXUS 55 digital camera. Photographs were then assessed for FROM by the same four observers and a further physician who had had no prior contact with the patients.
Photographs were not available to assessors until at least 21 days after initial assessment (mean 31, range 21-35 days). Photographs did not contain any identifying patient details and were presented to each assessor in a random order.
Range of flexion was measured with the patient sitting upright, weight evenly distributed between the ischial tuberosities, arm in the mid-prone position with the thumb facing anteriorly. The patient flexed their shoulder to elevate the arm until they reached their maximum range of flexion. FROM was measured as the maximum arm-trunk angle. A digital photograph was taken of the patient in profile, with the camera lens parallel to the sagittal plane of the patient and with the arm at maximum flexion [Figure 1].
Range of abduction was measured with the patient sitting upright, weight equally distributed between the ischial tuberosities and the arm in the anatomical position with the thumb pointing laterally. The patient abducted their shoulder to elevate the arm until they reached their maximum range of abduction. FROM was measured as the maximum arm-thorax angle in degrees. A digital photograph was taken of the patient from behind, with the camera lens parallel to the coronal plane of the patient, with the arm at maximum abduction [Figure 2].
Range of internal rotation was measured with the patient sitting upright, weight evenly distributed between the ischial tuberosities, arm in the anatomical position with the thumb pointing laterally. The patient internally rotated their shoulder to place their hand behind their back, and elevated their hand up their back to their maximum range of internal rotation. FROM was measured as the most cephalad vertebral level reached by the tip of the thumb. A digital photograph was taken of the patient from behind, with the camera lens parallel to the coronal plane of the patient and with the arm in maximum internal rotation [Figure 3].
Range of external rotation was measured with the patient sitting upright, weight evenly distributed between the ischial tuberosities, elbow flexed to 90° and held against the thorax (zero abduction). The hand was in the mid-prone position and thumb pointed cephalad. The patient externally rotated their shoulder to their maximum range of external rotation. FROM was measured as the maximum angle between the arm and the sagittal plane of the thorax in degrees. A digital photograph was taken with the patient lying supine on a treatment couch, elbow flexed to 90° and held against the thorax, hand mid-prone with thumb pointed cephalad, and arm externally rotated to their maximum range of external rotation. Photographs were taken from above the patients head with the camera lens parallel to the axial plane of the patient and with the arm at maximum external rotation [Figure 4].
 Results Results | |  |
All statistical analysis was performed using the SPSS (SPSS v16.0; IBM Corporation) statistical package. Inter-observer intra-class correlation coefficients (Rho) were calculated for each movement assessed clinically and photographically. Intra-observer intra-class correlation coefficients (Rho) were calculated for each observer's assessment of clinical and photographic movements. A Rho value of greater than 0.75 represented excellent reliability. [10] 95% confidence intervals were calculated for each test.
The inter-observer intra-class correlation coefficients (Rho) for each movement tested clinically and photographically are given in [Table 2]. Rho values for all ROM measurements were deemed excellent on clinical assessment and photographic assessment. Inter-observer correlation coefficients were greater for clinical examination of flexion, but greater for photographic assessment of internal and external rotation. Inter-observer correlation coefficient for abduction was the same for both assessments.
Intra-observer correlation coefficients for each of the four observers' results of clinical assessment and photographic assessment are given in [Table 3]. All results show good to excellent correlation for all four observers. The inter-observer intra-class correlation coefficients (Rho) for all movements tested by all assessors are shown in [Table 4]. The reliability of results of four observers assessing patients clinically and five observers assessing digital photographs of 17 patients showed excellent reliability.
 Discussion Discussion | |  |
Digital photography is commonly used in clinical situations, and has previously been shown to be an accurate method of measuring range of motion of the elbow [11] and knee, [12] and coronal plane alignment of the lower limb. [13] We are not aware of any previous study that has demonstrated the reliability of digital photographs for assessment of FROM of the shoulder.
Our patient cohort had a wide age range and had undergone a variety of different procedures. This allowed us to assess a wide spectrum of shoulder function. Initial assessments included visual estimation of both shoulders in each patient. The majority of patients had normal function in their noninjured shoulder, and as such we found a "ceiling effect" in measurement. Under these circumstances, the variance of estimated angles will necessarily be small, and so the correlation within and between observers is likely to be high: this is not a discriminatory assessment. Further assessment of 'normal' shoulders was abandoned. The mean visual estimate of FROM of all 'operated' shoulders was calculated. The age range of our cohort was wide (18-80 years, [Table 1]), and the FROM for all four measurements at initial assessment also showed sufficient variability to prevent a further "ceiling effect" [Figure 5].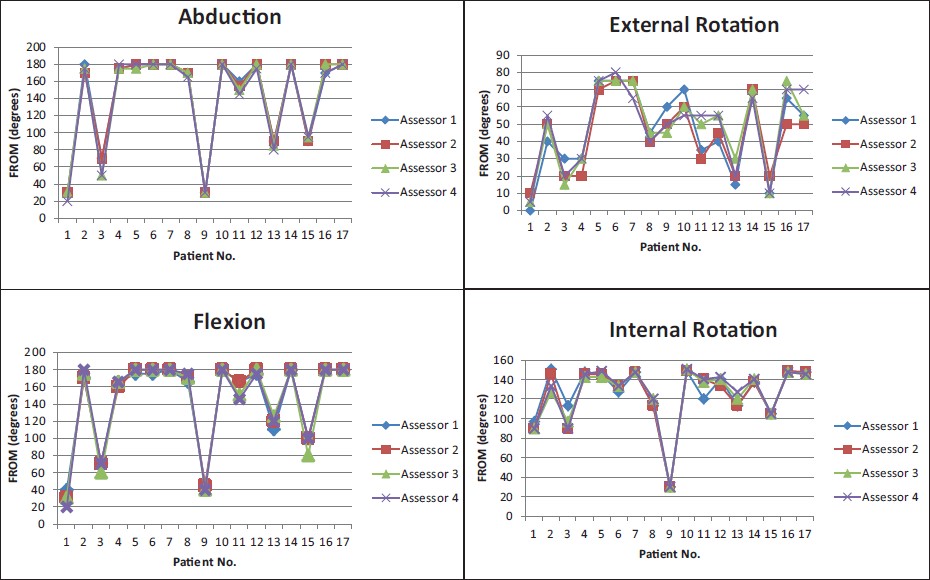 | Figure 5: Functional range of motion for all 4 measurements at initial assessment
Click here to view |
All photographs were taken with a standard digital camera available in any high street electrical store. No specialist equipment is required. Although we tried to ensure that all photographs were taken in exactly the same way, patient factors and space limitations meant that while all photographs were similar, all were slightly different in some way. We feel that this represents a true reflection of what would occur in clinical practice. These minor differences did not adversely affect the results, and demonstrate that while each photograph should be taken according to the criteria above, slight differences that may be introduced by multiple clinicians taking the photographs will not adversely affect the assessment.
We assessed patients using the guidelines set out by ESSSE for shoulder function. We modified the technique when taking photographs of external rotation, in order to make the photography as simple as possible. We expected the change in posture between the clinical assessment and the photographic assessment may affect the result, but it did not. The American Shoulder and Elbow Society (ASES) shoulder scoring system does not assess flexion or abduction, but combines the two movements as elevation. They also assess external rotation at 90° abduction and cross body adduction. These functions could easily be incorporated for photographic assessment.
The Intraclass Correlation Coefficient ICC scores achieved in this study are significantly greater than those of Hayes et al. [3] We compared two methods of assessment, Hayes et al. compared five. We feel that the smaller number of variables in our study is the reason for our higher reliability score. Both studies have shown poorer reliability of measurements of external rotation. Intra-observer scores for visual estimation of external rotation clinically and photographically were good for two assessors and excellent for the other two assessors in this study. The mean score was rated as excellent. As seen in [Table 2], the overall variability patient function in external rotation was greater than that for other measurements, thereby increasing the likelihood of differing results between assessors.
We have demonstrated that appropriately taken digital photographs can be used to accurately assess FROM, without requiring the patient to be present in the clinic. We are not, however, suggesting that digital photographic assessment of FROM alone is adequate for clinical monitoring of patient progress after shoulder surgery. We do feel that this technique is a useful adjunct to other established clinical assessment tools such as the Disabilities of the Arm, Shoulder and Hand (DASH) Questionnaire, the Rowe standard rating scale, [14] the SF-36, [15] and the Oxford Instability Scoring System. [16]
This has positive implications both clinically and in the field of research. In this study, we wrote to 111 patients who had sustained injury to their shoulder and undergone operative treatment. Of them, 63 patients (56.8%) replied but only 38 (34.3%) agreed to return for clinical assessment. All 38 patients were given a clinic appointment but only 17 (15.3%) attended. We asked these 17 patients if they would have preferred to be assessed in their own home, or if they preferred to attend clinic. Fourteen patients would have preferred the assessment to have been done at home; three said that they would not like to be assessed at home for reasons of privacy. All 17 patients stated that they would prefer to be assessed at a clinic/health centre close to their home.
When conducting clinical research it is important to exclude as many variables from a study as possible in order to focus on one aspect and validate results accurately. We have shown in this study that assessing the functional range of motion of the shoulder from digital photographs is as reliable as clinically assessing a patient in person. In our study cohort, 82% (14/17) indicated that they would have been willing to conduct their assessment at home, whereas 18% (3/17) stated that they did not want to be assessed at home. Using digital photography as a tool for clinical assessment of the shoulder at a place convenient to the patient will increase patient participation in research studies as it exempts patients from the financial and time burdens of attending a clinic. Our prospective cohort was located over a large geographical area and we have no doubt that travel time and finance was a factor in the poor response rate of the cohort. Using digital photography, these patients could have been assessed locally, with minimal time or financial cost to themselves, thereby increasing the numbers participating in the study and elevating its clinical relevance. Further clinical data could have been obtained using postal questionnaires like those already mentioned. [15],[16]
This also has implications for large multi-center and international trials. Each patient's ROM can be assessed by a single assessor from digital photographs, without that assessor having to personally assess each patient individually. Equally, a number of different assessors can assess the ROM of shoulders from many geographically diverse locations without having to visit each location individually.
We accept that visiting patients at home to assess their FROM is not financially viable in a clinical setting. Many of our patients could have been assessed by a local physician or physiotherapist with digital photographs being forwarded for clinical assessment. This would have reduced the numbers attending clinic, cut waiting times, negated patient travel, and provided a permanent record of FROM.
 Conclusions Conclusions | |  |
Digital photography is a viable means of assessing the functional range of motion of the shoulder. Photographs can be taken on any digital camera by any physician or therapist who follows the simple protocol. Photographs from different sources will undoubtedly have minor differences, but this will not affect the assessment. This has positive financial and patient satisfaction implications for clinical care, and is also of benefit in the field of research studies.
 References References | |  |
| 1. | Koljonen P, Chong C, Yip D. Difference in outcome of shoulder surgery between workers' compensation and nonworkers' compensation populations. Int Orthop 2009;33:315-20. 
|
| 2. | Fuchtmeier B, Brockner S, Hente R, Maghsudi M, Nerlich M, Prantl L. The treatment of dislocated humeral head fractures with a new proximal intramedullary nail system. Int Orthop 2008;32:759-65. 
|
| 3. | Lau TW, Leung F, Chan F, Chow SP. Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop 2007;31:657-64. 
|
| 4. | Chalidis B, Sachinis N, Dimitriou C, Papadopoulos P, Samoladas E, Pournaras J. Has the management of shoulder dislocation changed over time? Int Orthop 2007;31:385-9. 
|
| 5. | Maier M, Geiger EV, Ilius C, Frank J, Marzi I. Midterm results after operatively stabilised shoulder dislocations in elderly patients. Int Orthop 2009;33:719-23. 
|
| 6. | Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand - which one to choose? Int Orthop 2008;32:1-6. 
|
| 7. | Wagner JM, Rhodes JA, Patten C. Reproducibility and minimal detectable change of three-dimensional kinematic analysis of reaching tasks in people with hemiparesis after stroke. Phys Ther 2008;88:652-63. 
|
| 8. | Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Phys 2001;47:289-94. 
|
| 9. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Rel Res 1987;214:160-4. 
|
| 10. | Fleiss JL. The design and analysis of clinical experiments. New York, NY: Wiley; 1999. 
|
| 11. | Blonna D, Zarkadas PC, Fitzsimmons JS, ODriscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg 2012;21:29-35. 
|
| 12. | Verhaegen F, Ganseman Y, Arnout N, Vandenneucker H, Bellemans J. Are clinical photographs appropriate to determine the maximal range of motion of the knee? Acta Orthop Belg 2010;76:794-8. 
|
| 13. | Moncrieff MJ, Livingston LA. Reliability of a digital-photographic- goniometric method for coronal-plane lower limb measurements. J Sport Rehabil 2009;18:296-315. 
|
| 14. | Rowe CR, Patel D, Southmayd WW. The Bankart procedure: A long term end result study. J Bone Joint Surg Am 1978;60:1-16. 
|
| 15. | Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF36). I. Conceptual framework and item selection. Med Care1992;30:473-83. 
|
| 16. | Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br 1999;81:420-6. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
[Table 1], [Table 2], [Table 3], [Table 4]
|
