| |


 |
| Year : 2013 | Volume
: 7
| Issue : 2 | Page : 52-58 |
|
|
|
|
|
ORIGINAL ARTICLE Management of acute displaced midshaft clavicular fractures using Herbert cannulated screw: Technique and results in 114 patients
Martin Richardson1, Saeed Asadollahi2, Louise Richardson3
1 Department of Orthopaedic, Epworth Healthcare, Richmond VIC 3121, Australia
2 Westmead Hospital, Sydney, NSW 2145, Australia
3 Medical Student, Melbourne University VIC 3010, Australia
Correspondence Address:
Martin Richardson
The Epworth Healthcare Level 7, Suit 7.5, 32 Erin Street, Richmond VIC 3121
Australia
 Source of Support: None, Conflict of Interest: None  | 6 |
DOI: 10.4103/0973-6042.114227

|
|
|
|
| Date of Web Publication | 29-Jun-2013 |
 Abstract Abstract | | |
Purpose: A new and simple operative technique has been developed to provide internal fixation for midshaft clavicle fractures. This involves the use of a large fragment Herbert Screw that is entirely embedded within the bone. Screw fixation is combined with bone grafting from intramedullary reamings of the fracture fragments. The purpose of this report is to assess the outcomes following treatment of midshaft clavicular fracture using this method.
Materials and Methods: One hundred and fourteen patients with acute displaced midshaft fracture were identified between 2002 and 2007. All patients were followed until fracture union. Patients' medical records were reviewed. Disability of the Arm, Shoulder, and Hand questionnaire (DASH), and American Shoulder and Elbow Surgeons Elbow form (ASES) were posted to all patients. Outcome measures included union rate, time to union, implant removal rate, DASH, and ASES scores.
Results: Patients' median age was 29.5 years (interquartile range, 19-44 years). The most common injury mechanism was sports injury (28%). The median time from injury to surgery was 5 days (interquartile range, 2-9 days). Union occurred in an average of 8.8 weeks. Non-union occurred in three cases (2.6%). The re-operation rate for symptomatic hardware prominence screw was 1.7%. The median DASH score was 0.83 and the median ASES was 100 (n = 35).
Conclusions: Intramedullary fixation using cannulated Herbert screw can be used as an effective approach for operative management of midshaft clavicular fractures. Using this method, an appropriate outcome could be achieved and a second intervention for implant removal could be avoided in great majority of cases.
Level of Evidence: Level III
Keywords: Acute fracture, Herbert cannulated screw, internal fixation, intramedullary, midshaft clavicle fractures, open reduction
How to cite this article:
Richardson M, Asadollahi S, Richardson L. Management of acute displaced midshaft clavicular fractures using Herbert cannulated screw: Technique and results in 114 patients
. Int J Shoulder Surg 2013;7:52-8 |
 Introduction Introduction | |  |
"Clavicular fractures are a very common fracture in the upper limb accounting for 2.6to 4% of all adult fractures. [1],[2],[3] Eighty percent of adult clavicle fractures occur in the middle third of the bone. [3] While conservative treatment of clavicle fractures remains the mainstay of management plans in the majority of cases, recent literature has described incidences up to 31% of patients treated non-operatively developing unsatisfactory outcomes due to bony shortening, malunion, poor alignment, deformity or residual pain. [4],[5] In fact, long term sequelae following non-operative treatment in specific subsets of patients is not uncommon. [6],[7],[8]
Operative intervention may be necessary to correct the existing deformity, restore stability, and control pain; thus helping the patient to return to daily activities in a shorter period. [9] Supporting this notion, in a randomized controlled trial, by the Canadian orthopedic trauma society, open reduction internal fixation of acute displaced midshaft clavicular fractures (injury to operation interval ≤4 weeks) resulted in shorter union time, higher union rate, less malunion, and more patient satisfaction compared to non-operative treatment. [9]
This paper presents an alternative technique for intramedullary fixation of midshaft clavicle fractures using large fragment Herbert Screw (HS), [10] which incorporates use of intramedullary reamings of fractured fragments as a source of local bone graft. The main purpose of this study is to present application of this new technique in acute clavicular fractures. To our knowledge, the use of Herbert cannulated screws were previously described in non-unions only.
 Materials and Methods Materials and Methods | |  |
The database (private practice setting, Epworth hospital, Melbourne Australia) was searched for all clavicle fractures treated surgically between 2002 and 2007. Two hundred and twenty one clavicle fractures were identified. The medical records of the identified patients were reviewed for midshaft clavicular fractures treated surgically using the Herbert cannulated bone screw (Zimmer, Warsaw, US). During this period, 135 patients were surgically managed for fractures of the middle third of the clavicle. Twenty one patients had the operation performed >4 weeks post injury. One hundred and fourteen fractures in 114 patients were performed within 28 days after injury, who are the focus of this review.
The main indications for surgical intervention were: Complete displacement, shortening of the clavicle of more than 2 cm, associated chest injuries, floating shoulder, and fracture with comminution. Patient preference (i.e., quick return to job due to economic pressure) was also considered when planning management. All operations were performed by a single surgeon (M. R.). Preoperative radiologic exams (anteroposterior view and 15° cephalic tilt view) were used to assess fracture configuration. Fractures were classified, according to the orthopedic trauma association classification for diaphyseal clavicle, fracture into simple (15-B1), wedge (15-B2), and complex (15-B3). [11]
In order to assess the functional outcome, Disabilities of the Arm, Shoulder and Hand (DASH) [12] and American shoulder and elbow surgeons questionnaires (ASES) (self-evaluation part) [13] were mailed to the patients to complete and return it in an enclosed envelope. The fracture was considered united when there was no mobility or pain on stressing the fracture site, and/or evidence of bridging callus on radiographs. [14] Nonunion was defined as the lack of radiographic healing with clinical evidence of pain and mobility at the fracture site at 6 months after surgery. [14]
Operative technique
The operation was conducted under general anesthesia using Keflin (1 gram) at induction. The patient was positioned supine with the arms parallel to the body and head secured on a head ring. An incision 2-3 cm long was made directly over the fracture, extending to expose both main fracture fragments. Care was taken to protect the supraclavicular nerves when identified.
The medial fragment was then grasped with a reduction clamp and lifted out of the wound. Often the medullary canal was identified with a fine curette and then reamed [Figure 1]. The medial canal was hand drilled [Figure 2]. It is important not to perforate the antero-medial cortex. A depth gauge was used to measure the length of the prepared canal. A guide wire was then inserted. The medial canal was tapped to the previous measured length.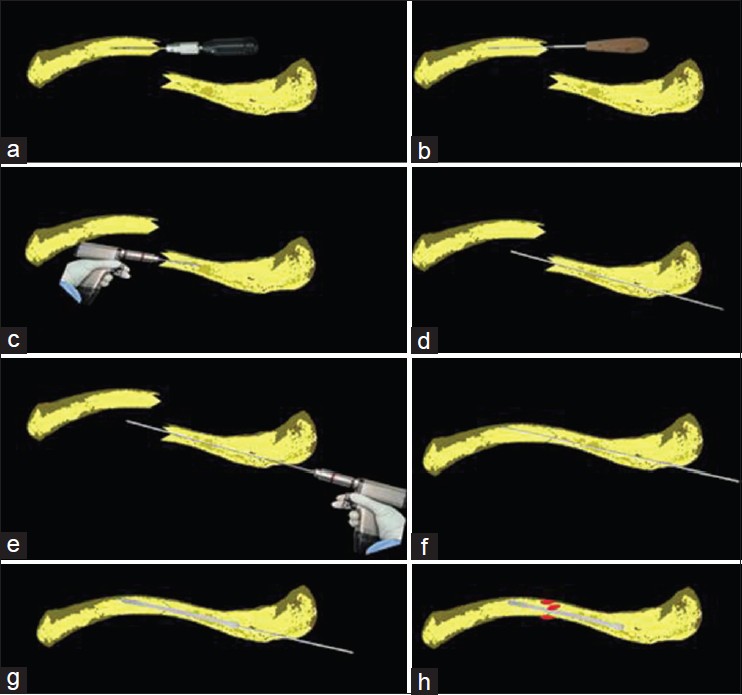 | Figure 1: Operative technique: (a) The intramedullary canal of the medial fragment hand drilled. (b) The intramedullary canal of the medial fragment tapped. (c) The intramedullary canal of the lateral fragment
power drilled (d) Guide wire is inserted retrogradely. (e) Posterolateral cortex drilled out using step drill. (f) Guide wire reinserted and fracture reduced. (g) Introduction of cannulated Herbert screw to fracture site.
(h) Bone graft harvested from the intramedullary source placed around the fracture site
Click here to view |
Next, the intramedullary canal of the lateral fragment was power drilled until it penetrated through the poster-lateral cortex behind the acromion-clavicular joint [Figure 3]. The length of the canal was measured and tapped accordingly. A guide wire was passed retrogradely through the canal and lateral cortex allowing a postero-lateral portal to be made, and the lateral fragment tapped with an appropriately sized tape. A step drill was used to enlarge the lateral cortex over guide wire through the lateral stab incision.
The main medial and lateral fracture fragments were then reduced over the guide wire. Using a cannulated screw driver, the Herbert cannulated screw of appropriate diameter and length was inserted over the guide wire. As the trailing threads engaged, the bone reduction was achieved. Care is taken to prevent shortening (over reduction) in comminuted fractures. The butterfly fragments in comminuted fractures were reduced and held with a suture, taking care not to further devascularize the soft tissue attachments. Autogenous bone graft obtained during reaming of fractured fragments was packed around the fracture site.
The wounds were closed and local anesthetic was injected around skin incisions. No drain tube was used. After surgery, the patient's arm was supported in a sling. Postoperative anteroposterior and 15° cephalad radiographs were taken in the recovery room and at subsequent follow-up appointments until fracture union. Gentle passive range of motion, with the arc limited to 90°, was commenced as soon as possible and active assisted motion was commenced at 2 weeks. Patients were advised to avoid vigorous exercise or work with heavy loads, during the first 6 weeks after surgery.
Statistical analysis
Statistical analysis was performed with the Statistical Package for the Social Sciences (SPSS) software (version 14; SPSS, Chicago, Illinois). Simple descriptive and frequency analyses were performed on multiple variables. Data are presented as median and interquartile ranges when not normally distributed. The Kruskal Wallis test was used to test for any significant differences between age in various mechanism groups. The Mann-Whitney test was used to compare age differences between respondent and non-respondents. A Chi-square test was used to test for a significant relationship between categorical variables. P values of <0.05 were considered significant for all tests.
 Results Results | |  |
Eighty percent were male (n = 91). The median age at the time of operation was 29.5 years (interquartile range, 19-44 years). The dominant hand was affected in 49% of cases. A summary of injury mechanism as well as age distribution is given in [Table 1]. There was no significant difference between age distributions in various mechanism groups. Sports injury was the most common mechanism of injury (28%). Eight patients had associated injuries, which included rib fractures (four patients), scapular fracture (two patients), pneumothorax (one patient), pelvic fracture (one patient), and metacarpal fracture (one patient). There were no open fractures. There was no motor or sensory dysfunction of the upper extremity before surgery.
Fracture configurations were as follows: 35 (31%) simple fractures (15-B1), 56 (49%) with a butterfly fragment (15-B2), and 23 (20%) comminuted (15-B3). There was no significant relationship between mechanism of injury and fracture configuration (P = 0.38, chi square test). [Table 2] and [Table 3] demonstrate the distribution of the different sizes of cannulated HS used in the treated population. Either 4.5 mm or 6.5 mm screws were used for clavicle fracture fixation (14% and 86% of patients, respectively). The median interval between injury date and operation was 5 days (interquartile range, 2-9 days). All patients were followed up until fracture union [Figure 4] and [Figure 5]. The mean time to union was 8.8 weeks (median 7.7 weeks, interquartile range, 6-10 weeks).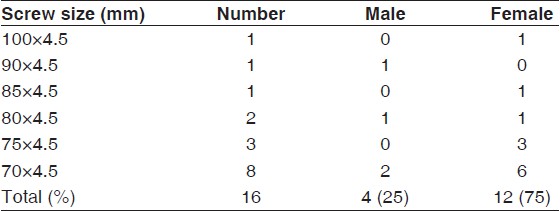 | Table 2: Distribution of 4.5 mm cannulated Herbert screw of different lengths in the treated male and female patients with fracture of middle third of clavicle
Click here to view |
 | Table 3: Distribution of 6.5 mm cannulated Herbert screw of different lengths in the treated male and female patients with fracture of middle third of clavicle
Click here to view |
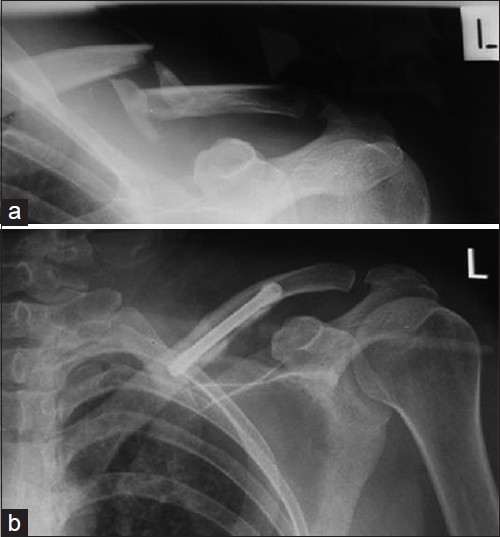 | Figure 4: (a) A 30-year-old lady sustained a displaced comminuted fracture of right clavicle due to a fall. (b) Postoperative radiograph shows restoration of clavicle alignment. Precise anatomic reduction is one of the advantages of intramedullary fixation of clavicle fracture using cannulated Herbert screw
Click here to view |
 | Figure 5: (a) Displaced midshaft fracture of right clavicle in an 18-yearold student. (b) Postoperative radiograph: Cannulated Herbert screw is completely buried in the clavicle. Special design of screw obviates
the need for reoperation in great majority of cases
Click here to view |
Thirty-five patients filled and returned the questionnaire (response rate = 31%). Details of respondents are: Median age 35 (range, 11-61), male 80% (n = 28), dominant side fracture 43% (n = 15), injury mechanism (traffic accident 29%, fall 29%, sports injury 29%, direct blow 6%, not known 7%), and median follow-up (from injury to assessment) of 14 months (interquartile range, 10-25 months). No difference was found in age, gender, dominant side fracture, mechanism, fracture type, and associated injuries between respondents and non-respondents.
The median DASH score was 0.83 (interquartile range, 0-2.5). The median ASES score was 100 (97.5-100). After converting the scores to nominal rating: 91% of cases were excellent (n = 32) and 9 percent as good (n = 3) based on ASES scores, 97% (n = 34) were rated as excellent and 3% (n = 1) as fair according to DASH measurement.
Complications and subsequent procedures
The incidence of the postoperative complications is shown in [Table 4]. There were only three cases of non-union in this study (2.6%). First case was a 33-year-old man with displaced midshaft fracture that was primarily fixed with a 4.5 × 70 mm HS. Postoperative follow-up revealed hypertrophic non-union five months post operation [Figure 6]. A revision procedure was performed using a 6.5 × 70 mm HS and the fracture united 12 weeks later.
The second case was of a 64-year-old man, who refractured his right clavicle 4 years ago in motor bike accident. Initially, the fracture was treated surgically, using cannulated (100 × 6.5 mm) and united. The subsequent fracture occurred at the medial end of the original screw (junction of medial third and lateral two-thirds of clavicle). The original HS was removed; the lateral cortex was over drilled and a 100 × 6.5 mm HS was reinstituted to hold the fracture in place. However, the HS could not achieve a good bite on the medial fragment, resulting in superior displacement and non-union. This was subsequently managed with plate fixation and iliac crest bone grafting. | Figure 6: Hypertrophic non-union of the midshaft of the clavicle 5 months after operative treatment with 4.5 × 75 mm Herbert cannulated bone screw. There is a clear zone of lucency around the leading head
of screw
Click here to view |
The third case was a 42 year old man with a displaced fracture of the middle third of his right clavicle, with one large butterfly fragment. His fracture was internally fixed with a 100 × 6.5 mm HS. During follow-up, he developed increasing pain over the fracture site associated with limited shoulder movement, which was subsequently diagnosed as atrophic non-union and treated with dynamic compression plating and a local bone graft. Bony union occurred within three months of the revision surgery.
One patient experienced asymptomatic delayed union. He was a 33-year-old cricket player with refracture of the right midshaft clavicle, after 4 years. His initial fracture was surgically fixed using a modified Hagie pin (before the start of the new technique), which was removed after 3 months. He refractured the right clavicle while playing cricket. The fracture line ran through the callus site, with one butterfly fragment. The refracture was internally fixed using a HS. In this case, the fracture united after 7 months.
One 54-year-old businessman developed a deep vein thrombosis after treatment for a right mid third clavicle fracture (shortened with one butterfly fragment) 2 weeks after initial injury. He developed a swollen right arm, within 1 to 2 days post-surgery, and the axillary vein thrombosis was managed with anticoagulation therapy.
There was no case of medial migration of pin in the current study, nor was any intraoperative neurologic injury reported. Only one case of deep infection was recorded, which settled with antibiotic treatment and screw removal at 9 weeks, at which point the fracture had united.
 Discussion Discussion | |  |
Although plate osteosynthesis is a well-known method for rigid fixation of clavicle fractures and nonunions; [3],[9],[15] it has the disadvantage of more extensive soft tissue stripping, a larger skin incision, and tendency for re-fracture after removal. [3],[15] Compared to plate fixation, an intramedullary screw is an effective alternative, which is less invasive, involves limited further soft tissue trauma, and a lower risk of neurovascular damage. [3],[16],[17] An ideal intramedullary device needs to be strong enough to hold the fractured fragments in a stable manner, and as well as being biocompatible, it should be technically simple for use. [18] The large fragment cannulated HS seems to offer these advantages and is well suited in size for the management of clavicle fractures.
The HS was first introduced by T. J. Herbert in 1984 as a new headless double-threaded screw and used in the management of scaphoid fractures. [19] Since then, there has been increasing interest in its use for other fractures. [20] A unique design of the HS is threading of a different pitch at either end of a smooth central shaft, with threads at the leading head (proximal) being wider than the trailing (distal) head. The pitch differential between the two threads causes compression as the leading threads advances more rapidly through the distal bony fragment. [19]
One of the problems traditionally associated with intramedullary fixation of clavicle fractures was that in many cases the pin had to be removed due to hardware irritation. [21] Another advantage afforded by the HS is that it does not have a head to protrude on the surface of the bone, which is especially of value in clavicle fractures in which a prominent screw head might cause skin irritation and the need for removal. [22] In the current study, only three patients complained of skin irritation due to prominent screw head, two of which (1.7% treated population) required removal. Early in the learning curve, lengths were over estimated resulting in the prominence in these cases.
There are few studies applying the cannulated HS in the management of clavicle fractures. Proubasta et al., compared mechanical strength of plating to that of the intramedullary HS, in midshaft clavicle fracture fixation. [23] The HS showed the same mechanical strength to failure as the plate did under bending force. Furthermore, Proubasta et al., successfully used the 4.5mm Herbert cannulated screw in the treatment of five clavicular non-unions. [18] The current review of 114 midshaft clavicular fractures, also demonstrates that the cannulated HS provides adequate stability of the fracture site against considerable tension, bending, and torsional forces; to allow for early postoperative activities and proper healing course.
In a systematic review by Houwert et al., in 2011, high quality evidence from one study and low quality evidence from three studies showed no difference in functional outcome and complications after plate fixation or intramedullary fixation for displaced midshaft clavicle fracture. [24] Another meta analysis by Zlowodzki et al., showed the overall nonunion rate for displaced midshaft fractures treated with plating is 2.2%, [4] significantly lower than the non-union rate following non-operative treatment of displaced midshaft clavicular fractures (15.1% in 159 analyzed fractures). The nonunion rate of 2.6% in this study compares favorably with the overall nonunion rate following plate fixation of displaced midshaft clavicle fractures, and is considerably lower than the nonunion rate following non-operative treatment of displaced midshaft clavicle fractures. [5]
Two out of three nonunion cases in this series were potentially related to technical issues. The 1 st nonunion case in the 33-year-old man was possibly due to lack of adequate stability at the fracture site using 4.5 mm cannulated screw in this case union was achieved by revising the screw to a larger diameter screw. In order to reduce the chance of nonunion following surgery, we suggest a 6.5 mm cannulated HS for fixation of acute displaced midshaft clavicle fractures, for most fractures. The smaller 4.5 mm cannulated HS is mostly used for females and teenagers (75% and 25% in this series, respectively). In the 2 nd nonunion case, the peri-prosthetic fracture was at the junction of medial third and lateral two thirds of clavicle. Probably due to a relatively short engaged length, purchase of the screw to the bone on the medial side was not strong enough to secure the medial fragment in revision fixation. The cannulated HS is not recommended for internal fixation of either medial and lateral third clavicular fractures or peri-prosthetic fractures in which the fracture line seems too far lateral or medial for the screw to have adequate purchase.
One limitation to the functional outcome part of our study is a low response (31%), that limits its validity or generalizability. However, there were no significant difference between the respondent and non-respondents in terms of demographics, injury mechanism and fracture configuration. Another limitation of our study is its retrospective nature, with all the inherent weaknesses associated with a retrospective design. For example, union time was assessed, retrospectively. However, effort was made to extract the data regarding union time as accurately as possible. A randomized controlled trial is warranted, to compare results of acute displaced midshaft clavicular treatment using cannulated HS versus other methods or non-operative treatment. The complication rate is subject to underreporting due to the short duration of follow-up. Selection bias is another potential limitation of this study as it reports the outcome of patients managed in a private setting only.
To conclude, the described technique of clavicle fixation with a large fragment cannulated HS is an alternative approach for the treatment of acute midshaft clavicular fractures and offers several advantages. As well as restoring the precise anatomy, limited exposure leaves a small skin scar with acceptable cosmetic appearance. Being completely buried within the clavicle bone, application of Herbert cannulated screw minimizes postoperative skin irritation and the need for secondary procedures for implant removal. Finally, this technique of internal fixation of clavicle fractures is simple and can be easily mastered and practiced. In properly selected cases, the technique is effective and can yield good functional outcomes.
 Acknowledgment Acknowledgment | |  |
We are grateful to Alexandra Gorelik from the epidemiology unit of the Royal Melbourne hospital for the statistical analysis of data.
 References References | |  |
| 1. | Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002;11:452-6. 
[PUBMED] |
| 2. | Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res 1994;127-32. 
|
| 3. | Hubner EJ, Hausschild O, Sudkamp NP, Strohm PC. Clavicle fractures--is there a standard treatment? Acta Chir Orthop Traumatol Cech 2011;78:288-96. 
|
| 4. | Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD, Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: Systematic review of 2144 fractures: On behalf of the evidence-based orthopaedic trauma working group. J Orthop Trauma 2005;19:504-7. 
[PUBMED] |
| 5. | Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537-9. 
[PUBMED] |
| 6. | Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: A prospective study of 222 patients. Acta Orthop 2005;76:496-502. 
[PUBMED] |
| 7. | van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: Current concepts review. J Shoulder Elbow Surg 2012;21:423-9. 
[PUBMED] |
| 8. | Davies D, Longworth A, Amirfeyz R, Fox R, Bannister G. The functional outcome of the fractured clavicle. Arch Orthop Trauma Surg 2009;129:1557-64. 
[PUBMED] |
| 9. | Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am 2007;89:1-10. 
|
| 10. | Zimmer Herbert™ Cannulated Bone Screw, Warsaw: Zimmer, Inc., [last updated 10/21/2011]. Available from: http://www.zimmer.com/z/ctl/op/global/action/1/id/9214/template/MP/prcat/M7/prod/y 
|
| 11. | Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium-2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 2007;21:S1-133. 
[PUBMED] |
| 12. | SooHoo NF, McDonald AP, Seiler JG 3 rd , McGillivary GR. Evaluation of the construct validity of the DASH questionnaire by correlation to the SF-36. J Hand Surg Am 2002;27:537-41. 
|
| 13. | Richards RR, Ann KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for assessment of shoulder function. J Shoulder Elbow Surg 1994;3:347-52. 
|
| 14. | Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004;86-A:1359-65. 
[PUBMED] |
| 15. | Poigenfurst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: Results of 122 operations. Injury 1992;23:237-41. 
|
| 16. | Parsons M, Blitzer C. Small-Incision, Intramedullary compression osteosynthesis of acute and non-united midshaft clavicle fractures. Tech Shoulder Elbow Surg 2005;6:218-25. 
|
| 17. | Smekal V, Oberladstaetter J, Struve P, Krappinger D. Shaft fractures of the clavicle: Current concepts. Arch Orthop Trauma Surg 2009;129:807-15. 
[PUBMED] |
| 18. | Proubasta IR, Itarte JP, Lamas CG, Caceres E. Midshaft clavicular non-unions treated with the Herbert cannulated bone screw. J Orthop Surg (Hong Kong) 2004;12:71-5. 
|
| 19. | Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br 1984;66:114-23. 
[PUBMED] |
| 20. | Reimer H, Kreibich M, Oettinger W. Extended uses for the Herbert/Whipple screw: Six case reports out of 35 illustrating technique. J Orthop Trauma 1996;10:7-14. 
[PUBMED] |
| 21. | Strauss EJ, Egol KA, France MA, Koval KJ, Zuckerman JD. Complications of intramedullary Hagie pin fixation for acute midshaft clavicle fractures. J Shoulder Elbow Surg 2007;16:280-4. 
[PUBMED] |
| 22. | Ngarmukos C, Parkpian V, Patradul A. Fixation of fractures of the midshaft of the clavicle with Kirschner wires. Results in 108 patients. J Bone Joint Surg Br 1998;80:106-8. 
[PUBMED] |
| 23. | Proubasta IR, Itarte JP, Caceres EP, Llusá MP, Gil JM, Planell JA, et al. Biomechanical evaluation of fixation of clavicular fractures. J South Orthop Assoc 2002;11:148-52. 
|
| 24. | Houwert RM, Wijdicks FJ, Steins Bisschop C, Verleisdonk EJ, Kruyt M. Plate fixation versus intramedullary fixation for displaced mid-shaft clavicle fractures: A systematic review. Int Orthop 2012;36:579-85. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6]
[Table 1], [Table 2], [Table 3], [Table 4]
|
