| |


 |
| Year : 2013 | Volume
: 7
| Issue : 2 | Page : 59-64 |
|
|
|
|
|
ORIGINAL ARTICLE Floating shoulders: Clinical and radiographic analysis at a mean follow-up of 11 years
ReĢ gis Pailhes1, Nicolas Bonnevialle1, JeanMichel Laffosse1, JeanLouis Tricoire2, Etienne Cavaignac1, Philippe Chiron1
1 Department of Orthopeadic and Traumatology, Musculoskeletal Institute, Toulouse, France
2 Department of Orthopeadic and Traumatology, Musculoskeletal Institute; Laboratory anatomy, University Hospital of Toulouse, Toulouse, France
Correspondence Address:
Nicolas Bonnevialle
Centre Hospitalier Universitaire de Toulouse-Purpan, Place du Docteur Baylac, 31059 Toulouse Cedex
France
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/0973-6042.114230

|
|
|
|
| Date of Web Publication | 29-Jun-2013 |
 Abstract Abstract | | |
Context: The floating shoulder (FS) is an uncommon injury, which can be managed conservatively or surgically. The therapeutic option remains controversial.
Aims: The goal of our study was to evaluate the long-term results and to identify predictive factors of functional outcomes.
Settings and Design: Retrospective monocentric study.
Materials and Methods: Forty consecutive FS were included (24 nonoperated and 16 operated) from 1984 to 2009. Clinical results were assessed with Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Single Assessment Numeric Evaluation (SANE), Short Form-12 (SF12), Disabilities of the Arm Shoulder and Hand score (DASH), and Constant score (CST). Plain radiographs were reviewed to evaluate secondary displacement, fracture healing, and modification of the lateral offset of the gleno-humeral joint (chest X-rays). New radiographs were made to evaluate osteoarthritis during follow-up.
Statistical Analysis Used: T-test, Mann-Whitney test, and the Pearson's correlation coefficient were used. The significance level was set at 0.05.
Results: At mean follow-up of 135 months (range 12-312), clinical results were satisfactory regarding different mean scores: SST 10.5 points, OSS 14 points, SANE 81%, SF12 (50 points and 60 points), DASH 14.5 points and CST 84 points. There were no significant differences between operative and non-operative groups. However, the loss of lateral offset influenced the results negatively. Osteoarthritis was diagnosed in five patients (12.5%) without correlation to fracture patterns and type of treatment.
Conclusions: This study advocates that floating shoulder may be treated conservatively and surgically with satisfactory clinical long-term outcomes. However, the loss of gleno-humeral lateral offset should be evaluated carefully before taking a therapeutic option.
Keywords: Arthritis, clavicle, floating shoulder, fracture, scapula
How to cite this article:
Pailhes Rg, Bonnevialle N, Laffosse J, Tricoire J, Cavaignac E, Chiron P. Floating shoulders: Clinical and radiographic analysis at a mean follow-up of 11 years. Int J Shoulder Surg 2013;7:59-64 |
 Introduction Introduction | |  |
The so-called floating shoulder (FS) was first introduced by Herscovici in 1992, [1] and was described as a combination of a scapular-neck fracture and a mid-clavicular ipsilateral fracture. According to Goss, [2] it consists of a double disruption of the superior suspensory complex of the shoulder and therefore, can involve the osseous structure and ligament complex as well. Williams et al., [3] reported on a cadaveric model that the stability of glenoid neck and clavicular fracture depends on the coracoacromial and acromioclavicular ligament integrity.
There is controversy in the literature with regard to treatment and outcome after this rare injury. [4],[5],[6],[7] Thus, the aim of our study was to evaluate the long-term results of conservative and surgical options, and to determine predictive factors of functional outcomes.
We hypothesized firstly, that operative treatment lead to better results than conservative one, and secondly that fracture displacement was a major predictive factor.
 Materials and Methods Materials and Methods | |  |
Inclusion and exclusion criteria
This investigation is based on a retrospective monocentric study. All patients gave their agreement to use the clinical and radiographic data for scientific study.
Inclusion criteria were: (1) a floating shoulder defined by Goss, (2) treated operatively or non-operatively, (3) reviewed clinically and radiographically, and (4) with a minimum follow-up of 12 months. Patients who were excluded were (1) less than 15 years old, (2) with history of previous injury of the shoulder affected, and (2) those who died secondary to associated injury.
From 1984 to 2009, 48 consecutive patients were treated for a floating shoulder injury in our institution. One patient died consecutively of multiple associated injuries and seven were lost to follow-up, leaving 40 patients (40 shoulders) included in this study.
Epidemiological data
Thirty-four were males and six were females; the mean age was 39 years old (16-72); the dominant side was involved in 33 cases and the right shoulder in 30. Sixteen patients sustained the injury during a motorbike accident, two during a bicycle accident, and five during a car accident. Ten were struck as a pedestrian and seven had a fall during a domestic accident. Twelve patients were admitted in an intensive care unit for multiple associated injuries as detailed in [Table 1].
The most common association was a mid-shaft fracture of the clavicle and a fracture of the anatomical neck of the scapula. But in seven cases, the lesion of the scapula included a fracture of the glenoid. Fracture patterns are reported in [Table 2].
Therapeutic methods
Of the 40 patients, 24 were treated nonoperatively (Group I) and 16 were treated surgically (Group II). Indications for the surgical treatment were a significant displacement of one of the fractures (>1 cm), fractures with impending skin complicationsor the senior surgeon's preference for the remainder. These patients underwent operation within a mean of 8.4 days (1-45) since the trauma.
In 10 cases, the clavicle was fixed alone with a plate (eight cases) or K-wire (two cases) via an anterior approach; in three cases the scapula was simply stabilized with pins and plates via a posterior approach described by Judet; [8] and in three other cases both fractures were fixed with a double approach. Postoperatively, a sling was maintained during 6 weeks. Passive mobilization and pendulum exercises were allowed immediately.
Conservative treatment was proposed for patients with minimally displaced fracture and those who for whom surgery was contra-indicated because of hemodynamic instability. It consisted in a sling immobilization of the shoulder in internal rotation for a minimum of 6 weeks. Pendulum exercise were delayed at 3 weeks and as soon as associated injuries allowed it. Progressively self-passive mobilization was performed under a physiotherapist control; plain radiograph determined the time of healing in order to allow strengthening exercises.
Clinical and radiographic evaluation
During follow-up cessions, patients were reviewed specifically for this study with clinical examination and radiographic evaluation. Active and passive shoulder motion, including forward elevation, external rotation at side, and internal rotation (reaching spinous process with one's thumb), were collected.
Clinical results were assessed with questionnaires regarding objective data and general quality of life: Simple Shoulder Test (SST), [9] Oxford Shoulder Score (OSS), [10] Single Assessment Numeric Evaluation (SANE), [11] Short Form-12 (SF12), [12] and Disabilities of the Arm Shoulder and Hand score (DASH). [13] The Constant and Murley system (CST) scoring pain (15 points), range of motion (40 points), activities (20 points), and strength (25 points) was performed by the examiner. [14]
Plain radiographs of the shoulder in an AP view were collected during a chart review in order to evaluate secondary displacement and time of healing. The glenopolar angle (GPA) was measured. [15] Moreover, the chest X-ray analysis allowed to measure the decrease of the lateral offset of the shoulder involved in comparison of the healthy side: The offset was defined as the distance between the medial border of clavicle and the tangent to the greater tuberosity of the humerus [Figure 1]. At the last follow-up, a new radiograph including the whole clavicle allowed to evaluate radiological outcomes of the involved shoulder. Osteoarthritis of gleno-humeral joint was classified according to Samilson. [16]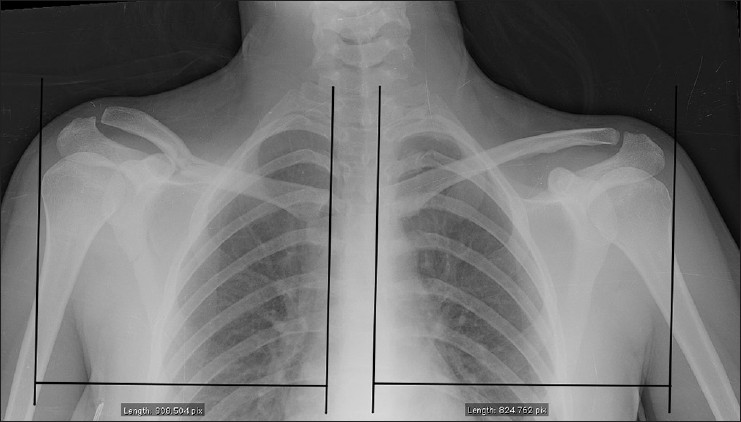 | Figure 1: Comparison of the lateral offset of the gleno-humeral joint between involved (right) and healthy (left) side on a chest X-ray. Figures were calculated using a measuring tool and do not have a metric unit correlation
Click here to view |
Statistical methods
Descriptive statistics, including means, or counts, percentages, standard deviation were calculated. The distribution of data was analysed with the d'Agostino-Pearson test. Means were compared in different groups of patients; for paired results a t-test was used whereas unpaired results were compared using the Mann-Whitney test. In cases where the two variables were continuous, the Pearson's correlation coefficient was used to determine whether the two variables were significantly related. The significance level was set at 0,05. SAS software was used (SAS Institute, Cary, NC).
 Results Results | |  |
Forty patients were reviewed clinically and radiographically by an independent observer at a mean follow-up of 135 months (range 12-312).
Complications and reoperations
One patient developed a superficial wound infection after plating the scapula which warranted an immediate surgical revision and antibiotherapy. The hardware was not removed and after follow-up it was noticed that the fracture healed and clinical outcome was satisfactory.
In one case treated conservatively, a secondary displacement was encountered at 15 days. A surgical procedure was not allowed immediately, because of associated injuries requiring resuscitation therapy. At 6 months, the clavicle shaft non-union was successfully treated with a plate fixation without bone graft.
In another case, a pin migration occured without secondary damage. It was a complex fracture which combined a comminutive scapula neck/glenoid fracture and midshaft clavicular fracture treated with a lag pin and cannulated screws.
Eight (50%) patients needed a material removal mainly because of a discomfort in the clavicle area.
No intraoperative vascular and neurologic damage was reported.
Clinical results
Objective results according to clinical scores are described in [Table 3]. There were no significant differences between Group I (operative) and II (non-operative).
The overall mean forward elevation was 148° (90-170), external rotation elbow at side was 49° (20-70) and internal rotation reached D10 (L5 - D7). Range of motions between groups I and II was not statistically different in forward elevation (144° versus 157°, respectively), external rotation (46° versus 53, respectively), and internal rotation.
Radiographic results
At follow-up, all but one fracture healed after the index therapy. As previously reported, one clavicular non-union needed a secondary surgery which was successful.
Osteoarthritis was diagnosed in five patients (12,5%): Four cases of stage 1 and one case of stage 4 according to Samilson. Neither the intra-articular position of the scapula fracture nor the type of treatment affected significantly this radiographic outcome. Moreover, with the present number of patients, we did not find a significant correlation between osteoarthritis and follow-up (Pearson's correlation; r = 0.2 P = 0.09).
The lateral offset of the shoulder was evaluated in 22 shoulders with an available chest X-ray. Six had been treated operatively and 16 non-operatively. A loss of the lateral offset was measured in 17 (77%) shoulders comparatively to the healthy side, without correlation with the type of treatment (operative or non-operative). The mean reduction expressed in percentage was 2.7% (1-12.2), and significantly influenced the decrease of the CST score, the SST, the OSS, and the DASH score (Pearson's correlation; r = 0.51 P = 0.02; r = 0.59 P = 0.004; r = 0.62 P = 0.001; r = 0.61 P = 0.002, respectively). No correlation was found with general quality of life scores: SF12 mental, SF12 physical, and SANE [Figure 2].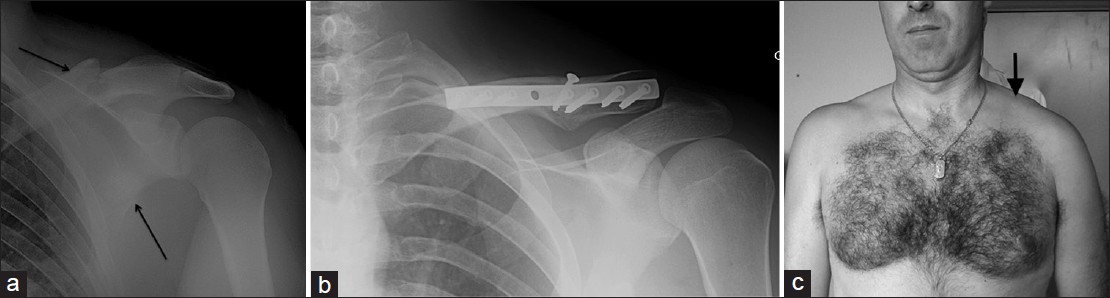 | Figure 2: (a) Floating shoulder with midshaft clavicular fracture and surgical scapular neck fracture (black arrows). (b) Open reduction and internal fixation of the clavicle with fracture healing. (c) Clinical presentation with a slight persistent drooping shoulder at 61 months of follow-up (white arrow)
Click here to view |
In the entire series, the mean GPA was 33.5° (19 -44). Only four patients (10%) had a GPA equal to 20 or less, without significant correlation with clinical results.
 Discussion Discussion | |  |
Floating shoulder is an uncommon injury, which is mainly associated to a high-energy trauma and multiples lesions. These associated injuries and their treatment may influence either the therapeutic decision making and the overall outcome of the FS. [5],[17],[18],[19],[20]
Based on the concept of the superior shoulder suspensory complex described by Goss, [2] a double disruption of this anatomical entity explains the potentially unstable situation for the upper limb. Therefore, a wide variety of bone and soft tissue injuries may be described. The FS is one of such double disruption and consists in an association of a scapula neck and clavicle fracture. According biomechanical cadaver study of Williams et al., [3] this lesion is stable unless associated with coracoacromial and acromioclavicular ligament disruption or spine or acromion fracture.
The displacement of the glenoid is not in caudal but in medial direction, secondary to contraction of the rotator cuff muscles. [1],[4] The alternative theory could be a lateral displacement of the scapula body with shortening of the fracture in the neck area. [20] The weight of the arm and contraction of biceps, coracobrachialis, and triceps muscles would pull the body of the scapula downward and laterally and create a clinical drooping shoulder.
Our study supports that the loss of lateral offset of the glenohumeral joint leads to worse functional objective results according to the Constant score. The shortening of the lever arms of the rotator cuff muscles and the modification of glenoid surface orientation may partially explain this result. Previously, in a 3D musculo-skeletal model, Chadwick et al., [21] had argued this biomechanical theory. Unfortunately, with the number of patient studied, we could not identify a (numeric) value of loss of lateral offset above which clinical consequences would be considered significant. Many authors reported pain and weakness in abduction in patients with unreduced scapular neck fractures but they did not allow to clearly define the limits of acceptable and non-acceptable displacement. [4],[22],[23]
Romero et al., [15] introduced the GPA as indicative of clinical outcomes of scapular neck fracture. A GPA less than 20° was defined as a severe rotational displacement, which could be one of the criteria for surgical reduction and internal fixation. [16],[24] However, the poor number of patients (four patients) concerned in our study did not allow us to share this conclusion.
In another way we did not find statistical differences in clinical outcomes between operative and conservative group and we could not highlight benefits of one option over the other. But according to radioclinical correlation, severe displacement seems to lower the results.
Previously, several series compared surgical and conservative treatment. [1],[17],[19],[25],[26]
Van Noort et al., [25] in a retrospective multicenter study did not prove the superiority of surgical treatment in seven patients over 28 treated conservatively (mean Constant score of 71 points versus 76 points, respectively). However, a severe caudal dislocation of the glenoid had a negative influence on the results.
Egol et al., [17] compared 12 patients treated conservatively (mean follow-up of 53 months) to 7 patients operated (mean follow-up of 36 months). Despite a clavicular non-union after non-operative treatment and a iatrogenic plexus injury after surgical treatment, the authors did not find a significant difference between objective clinical scores. But forward elevation was better in operative group. Therefore, they recommend an individualized treatment for each patient.
Labler et al., [19] reported excellent results in five of nine patients treated surgically and five of eight treated conservatively. However, because of inclusion of two patients with brachial plexus palsies, the mean constant score was lower in the operative versus non-operative group (90 points versus 66 points). That is why the authors confirmed that associated injuries influence the outcome of these patients and only recommend operative treatment for displaced fractures.
The choice of isolated stabilization of the clavicle may be debated. [1],[18],[27] The fixation of the clavicle can indirectly reduce the glenoid fracture. [28] Herscovici et al., [1] stabilized the clavicle with a plate in seven patients with excellent outcomes. According to the authors, this safe procedure prevents a drooping shoulder syndrome. Interestingly, Rikli et al., [27] included in their study patients with not only clavicular shaft fracture, but also acromioclavicular or sternoclavicular dislocation. Surgical treatment of the clavicular injury alone led to excellent functional results in nearly all 12 cases.
Long-term radiographic analysis is poorly reported in the literature. At a mean follow-up of 6.5 years, Hardegger et al., [4] reported one case (3%) of severe glenohumeral osteoarthritis after a floating shoulder syndrome. The present study suggests that incidence of osteoarthitis is higher (5 cases-12.5%) with a longer follow-up.
Our study has several weaknesses. Firstly, different surgeons with heterogeneous experience of such injury managed patients included. Secondly, the index therapeutic option was hedged by associated injuries, which may divert attention from the optimal treatment required.
However, it is the longest follow-up study of clinical and radiographic outcomes to date. Moreover, this is the first study, which reported exhaustively the rate of osteoarthritis at a long-term follow-up, and analysed the loss of lateral offset of the gleno-humeral joint.
This study advocates that floating shoulder may be treated conservatively and surgically with satisfactory clinical outcomes at long-term follow-up. The loss of glenohumeral lateral offset seems to have negative effect on clinical results and should be evaluated before the therapeutical decision proceeding. Large multicenter controlled study should be performed so as to offer clear recommendations.
 References References | |  |
| 1. | Herscovici D Jr, Fiennes AG, Allgöwer M, Rüedi TP. The floating shoulder: Ipsilateral clavicle and scapular neck fractures. J Bone Joint Surg Br 1992;74:362-4. 
|
| 2. | Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma 1993;7:99-106. 
[PUBMED] |
| 3. | Williams GR Jr, Naranja J, Klimkiewicz J, Karduna A, Iannotti JP, Ramsey M. The floating shoulder: A biomechanical basis for classification and management. J Bone Joint Surg Am 2001;83:1182-7. 
[PUBMED] |
| 4. | Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg Br 1984;66:725-31. 
[PUBMED] |
| 5. | Leung KS, Lam TP. Open reduction and internal fixation of ipsilateral fractures of the scapular neck and clavicle. J Bone Joint Surg Am 1993;75:1015-8. 
[PUBMED] |
| 6. | Ramos L, Ricardo M, Alberto A, Ferrandez L. Conservative treatment of ipsilateral fractures of the scapula and clavicle. J Trauma 1997;42:239-42. 
|
| 7. | Webber MC, Haines JF. The treatment of lateral clavicle fractures. Injury 2000;31:175-9. 
[PUBMED] |
| 8. | Judet R. Surgical treatment of scapular fractures. Acta Orthop Belg 1964;30:673-8. 
[PUBMED] |
| 9. | Roddey TS, Olson SL, Cook KF, Gartsman GM, Hanten W. Comparison of the University of California-Los Angeles Shoulder Scale and the Simple Shoulder Test with the shoulder pain and disability index: Single-administration reliability and validity. Phys Ther 2000;80:759-68. 
[PUBMED] |
| 10. | Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996;78:593-600. 
[PUBMED] |
| 11. | Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the single assessment numeric evaluation method and two shoulder rating scales. Am J Sports Med 1999;27:214-21. 
[PUBMED] |
| 12. | Ware J, Kosinski M, Keller S. A 12-item short-form health survey. Construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. 
|
| 13. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29:602-8. 
[PUBMED] |
| 14. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;1:160-4. 
|
| 15. | Romero J, Schai P, Imhoff AB. Scapular neck fracture. The influence of permanent malalignement of the glenoid neck on clinical outcome. Arch Orthop Trauma Surg 2001;121:313-6. 
[PUBMED] |
| 16. | Samilson RL, PrietoV. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am 1983;65:456-60. 
|
| 17. | Egol KA, Connor PM, Karunakar MA, Sims SH, Bosse MJ, Kellam JF. The floating shoulder: Clinical and functional results. J Bone Joint Surg Am 2001;83:1188-94. 
[PUBMED] |
| 18. | Hashiguchi H, Ito H. Clinical outcome of the treatment of floating shoulder by osteosynthesis for clavicular fracture alone. J Shoulder Elbow Surg 2003;12:589-91. 
[PUBMED] |
| 19. | Labler L, Platz A, Weishaupt D, Trentz O. Clinical and functional results after floating shoulder injuries. J Trauma 2004;57:595-602. 
[PUBMED] |
| 20. | van Noort A, van der Werken C. The floating shoulder. Injury 2006;37:218-27. 
[PUBMED] |
| 21. | Chadwick EK, van Noort A, van der Helm FC. Biomechanical analysis of scapular malunion: A simulation study. Clin Biomech (Bristol, Avon) 2004;19:906-12. 
[PUBMED] |
| 22. | Ada JR, Miller ME. Scapular fractures. Analysis of 113 cases. Clin Orthop Relat Res 1991;269:174-80. 
[PUBMED] |
| 23. | Edwards SG, Whittle AP, Wood GW. Nonoperative treatment of ipsilateral fractures of the scapula and clavicle. J Bone Joint Surg Am 2000;82:774-80. 
|
| 24. | Kim KC, Rhee KJ, Shin HD, Yang JY. Can the glenopolar angle be used to predict outcome and treatment of the floating shoulder? J Trauma 2008;64:174-8. 
[PUBMED] |
| 25. | van Noort A, te Slaa RL, Marti RK, van der Werken C. The floating shoulder. A multicentre study. J Bone Joint Surg Br 2001;83:795-8. 
[PUBMED] |
| 26. | Oh CW, Jeon IH, Kyung S, Park C, Kim T, Ihn C. The treatment of double disruption of the superior shoulder suspensory complex. Int Orthop 2002;26:145-9. 
|
| 27. | Rikli D, Regazzoni P, Renner N. The unstable shoulder girdle: Early functional treatment utilizing open reduction and internal fixation. J Orthop Trauma 1995;9:93-7. 
[PUBMED] |
| 28. | Owens BD, Goss TP. The floating shoulder. J Bone Joint Surg Br 2006;88:1419-24. 
[PUBMED] |
[Figure 1], [Figure 2]
[Table 1], [Table 2], [Table 3]
|
