| |


 |
| Year : 2013 | Volume
: 7
| Issue : 3 | Page : 116-119 |
|
|
|
|
|
CASE REPORT Lipoma arborescens associated with osseous/chondroid differentiation in subdeltoid bursa
Ryuh Sup Kim1, Young Tae Kim1, Jong Min Choi1, Sang Hyun Shin1, Yeo Ju Kim2, Lucia Kim3
1 Department of Orthopaedic Surgery, School of Medicine, Inha University, Incheon, Korea
2 Department of Radiology, School of Medicine, Inha University, Incheon, Korea
3 Department of Pathology, School of Medicine, Inha University, Incheon, Korea
Correspondence Address:
Sang Hyun Shin
Department of Orthopedic Surgery, Inha University Hospital, 7-206, 3rd Street Shinheung-Dong, Jung-Gu, Incheon, 400-103
Korea
 Source of Support: This study was financially supported by a grant from
Inha University., Conflict of Interest: None  | 2 |
DOI: 10.4103/0973-6042.118916

|
|
|
|
| Date of Web Publication | 25-Sep-2013 |
 Abstract Abstract | | |
Lipoma arborescens (LA) is a rare benign lesion of unknown etiology. It is characterized histologically by villous proliferation of the synovial membrane and diffuse replacement of the subsynovial tissue by mature fat cells. This condition affects the knee joint most commonly. Cases involving other locations including glenohumeral joint, [1] hip, [2] elbow, [3] hand [4] and ankle [5] have been rarely described. Involvement of the subdeltoid bursa has also been reported, but to date no case has described LA with osseous/chondroid differentiation of this bursa. Another significant finding in our case was the coexistence of LA with intermuscular lipoma, SLAP lesion and labral cyst.
Keywords: Labral cyst, lipoma, lipoma arborescens, osseous/chondroid differentiation, shoulder, SLAP lesion, subdeltoid bursa
How to cite this article:
Kim RS, Kim YT, Choi JM, Shin SH, Kim YJ, Kim L. Lipoma arborescens associated with osseous/chondroid differentiation in subdeltoid bursa. Int J Shoulder Surg 2013;7:116-9 |
 Introduction Introduction | |  |
Shoulder pain and limitation of motion comprise a multifactorial disorder. Tumoral lesions are a relatively rare cause of shoulder pain, but should be considered, especially when clinical presentation is unusual. Lipoma arborescens (LA) is a rare benign hyperplastic tumor which rarely involves the shoulder region. The term "arborescens" originate from the Lain word arbor meaning tree, describing the characteristic tree like morphology. To the best of our knowledge, previous cases of LA located in subdeltoid bursa were associated with a rotator cuff tear. We present a case of LA coexisting lipoma, SLAP lesion and paralabral cyst. However, this case had intact rotator cuff. A review of the medical literature related to this entity is also reported.
 Case Report Case Report | |  |
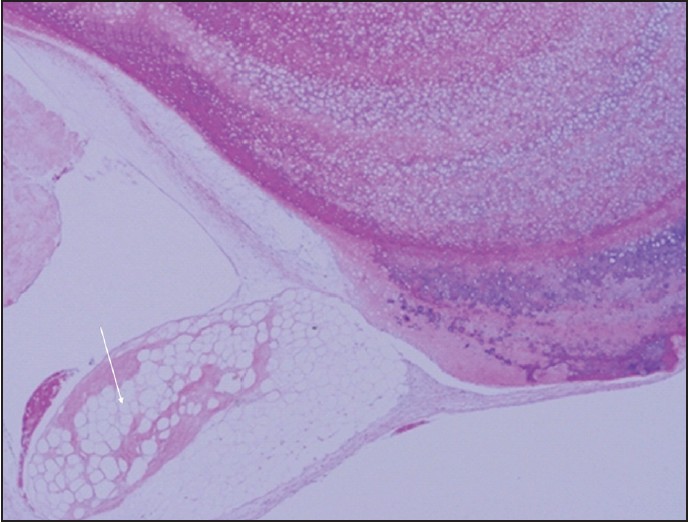
A 43-year-old, right-handed woman presented with complaints of pain and discomfort in her right shoulder. She had no history of previous injury or minor problems with her shoulder. The symptoms had begun after labor related to institutional food service for 1½ years. She had occasionally experienced a catching sensation and aggravated pain in the shoulder with labor activity. Symptoms were not alleviated by rest or non-steroidal anti-inflammatory drugs. Physical examination revealed positive findings for Neer's sign and Hawkins impingement test, Speed test and O'Brien's test. Patient's rotator cuff muscle strength was normal and no musculature atrophy was observed. The active range of motion (ROM) of the shoulder joint was mildly restricted during flexion, abduction and internal rotation, but passive ROM showed full range. The laboratory investigations including erythrocyte sedimentation rate and serology showed no significant results. Plain radiograph of shoulder demonstrated multiple rounds and ring like calcifications at the right glenohumeral joint with entheophyte at greater tuberosity of right humeral head [Figure 1]. Magnetic resonance imaging (MRI) of the shoulder showed a fluid-filled paralabral ganglion cyst that originated at the posterior superior labrum, forming a large cystic mass located at suprascapular and spinolgenoid notch around the spine of scapula [Figure 2]a and b. The cyst originated at a tear of the superior labrum and extended to the posterior aspect of biceps long head origin [Figure 2]a and b]. The axial MRI also revealed fatty mass, which showed iso-signal intensity to the subcutaneous fat on all sequences, under intermuscular space located between anterolateral cortex of the humeral head and anterior belly of the deltoid muscle [Figure 2]b. Another encapsulated mass was found in intermuscular space between infraspinatus and the deltoid muscle [Figure 2]b. Abundant villous projection on the medial portion of the mass was located with multiple rings like or round low intensities on all pulse sequences. It showed background low signal intensity on T1-weighted image and high signal intensity on T2-weighted image, representing calcification arising from chondroid matrix [Figure 2]c and d. Arthroscopy revealed a type II SLAP lesion with mild synovitis, but the articular cartilage of the humeral head and glenoid was intact. The detached posterior-superior labrum was fixed with sutures by insertion of two metal anchors. Patient subsequently underwent a separate incision laterally around the acromion and medially along the lateral one-third of the spine of the scapula. The origin of the deltoid was detached from the acromion and from the exposed part of the spine of the scapula. We retrieved LA and lipoma respectively. Lipoma size was 1.8 cm × 2.2 cm × 1.7 cm. LA size was 7.1 cm × 2.8 cm × 2.6 cm in the form of encapsulated mass. Opening the capsule revealed villous projection of fatty synovial tissue associated with central large whitish cartilaginous nodules attached to villous synovium [Figure 3]. Histologic examination demonstrated that diffuse papillary proliferation of the synovium with near total replacement of subsynovial tissue into mature fat tissue. Extensive area of osteochondral metaplasia in villous fat tissue was also seen [Figure 4] and [Figure 5].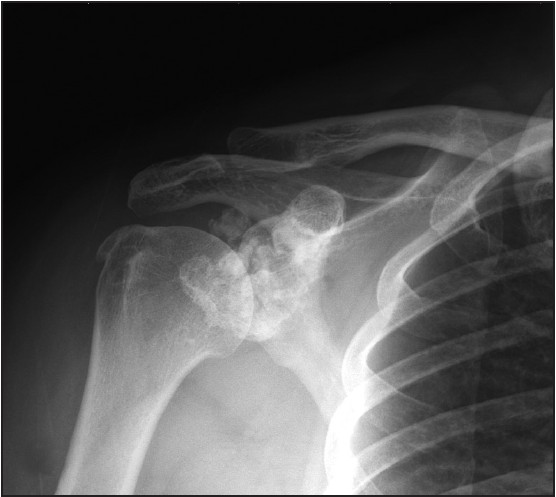 | Figure 1: Anteroposterior radiographs shows multiple round and ring like calcifications at glenohumeral joint
Click here to view |
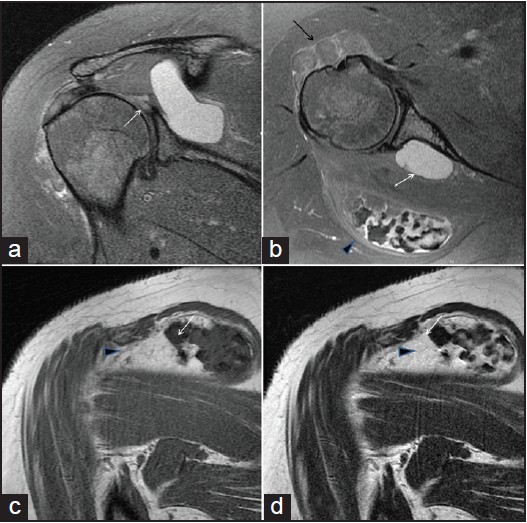 | Figure 2: Oblique coronal (a) and axial (b) fat suppressed proton density, oblique coronal T1-weighted (c) and T2-weighted magnetic resonance images (d). (a) There is T2 high signal intensity (short arrow) at posterosuperior labrum, suggesting labral tear. (b) Large T2 high signal intensity cystic lesion (white arrow) is seen adjacent to the labral tear extending into spinoglenoid notch, suggesting paralabral ganglion cyst. A fatty mass is seen between anterolateal cortex of the humeral head and anterior belly of the deltoid muscle, indicating intramuscular lipoma (black arrow). Another encapsulated mass is also seen in intermuscular space between infraspinatus and deltoid muscles (arrow head). (c and d) Arrow heads in c and d indicates encapsulated mass as seen b. It had abundant villous projections on the medial portion. It also had multiple rings like or round low signal intensities on all pulse sequences with background low signal intensity on T1-weighted image and high signal intensity on T2-weighted image. This represents calcification arising from chondroid matrix (white arrow)
Click here to view |
 | Figure 3: Grossly, central whitish cartilaginous excrescences are surrounded by papillary proliferation of fat tissue. Lipoma arborescens is indicated with the white arrow
Click here to view |
 | Figure 4: Microscopic examination confirms focal osteochondral metaplasia of villous fat tissue in lipoma arborescens (H and E, ×40)
Click here to view |
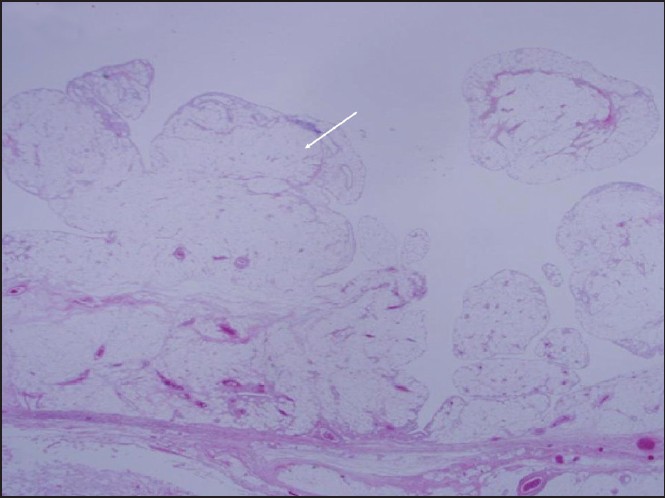 | Figure 5: Histologic examination reveals hypertrophic nodular villous proliferation with adipocytes in subsynovial connective tissue, consistent with lipoma arborescens (H and E, ×12.5)
Click here to view |
Post-operatively, the arm was placed at the side in a sling for 3 weeks. Passive motion including external rotation of the shoulder and ROM of the elbow were started immediately. This was followed by a home-based rehabilitation program of progressive ROM. Strengthening exercises for the rotator cuff, scapular stabilizers and deltoid were started 6 weeks post-operatively. She achieved full recovery in her affected shoulder within 3 months of surgery. At 2-month follow-up, the ultrasonogram demonstrated complete removal of LA, lipoma and cyst. She was asymptomatic and showed no recurrence of calcification on plain radiographs at a final follow-up 3 years after surgery.
 Discussion Discussion | |  |
The lesion in the joint or bursa, which contains a substantial amount of fat may be considered as a lipoma or LA. Lipomas, one of the most common benign neoplasms of soft-tissues, are composed of mature adipocytes and can arise as a solitary mass in any part of the human body where there is fatty tissue. The etiology of lipomas remains obscure. Chronic irritation, trauma and spontaneous development have been mentioned. Lipomas occur predominantly in middle-aged men within the subcutaneous tissue of the posterior neck, shoulder and arms. They may occur at other tissue depths including intermuscular planes. [6]
LA is a benign intra-articular lesion characterized by diffuse replacement of the subsynovial tissue into mature fat cells, producing villous transformation of the synovium. [2],[7],[8],[9],[10] Although it generally involves the knee joint, LA has been described rarely in multiple joints including glenohumeral joint, [1] hip, [2] elbow, [3] hand [4] and ankle. [5] Differential diagnosis must be carried out between synovial proliferative disorders and synovial processes with a fatty tissue component such as synovial lipoma [6],[11] and synovial osteochondromatosis (SO). Synovial proliferative disorders such as hemangioma, rheumatoid synovitis and pigmented villonodular synovitis have a characteristic MRI appearance that should not create a diagnostic problem. [12] Synovial lipoma is very rare and it is usually a single circumscribed round or oval mass that shows the same signal intensity as fat tissue. This is, however, distinguished from LA by the absence of the tree-like aspect of LA on MRI finding. Osteochondral bodies in SO present a low peripheral signal due to calcification and are visible in the radiological studies. Our case with lipomatous lesion associated with osseous/chondroid differentiation, resembled a primary SO. The following features supported the diagnosis of LA, rather than synovial chondromatosis: Fatty villi interspersed with effusion on MRI [Figure 2]b and c, macroscopic fatty synovial proliferation with villous configuration and the histological evidence of diffuse subsynovial fat [Figure 4]. The etiology of LA remains controversial. It has been considered to be a reactive process of the synovial tissue, which could be associated with joint trauma, [2] rheumatoid arthritis, [13] osteoarthritis, [8] and psoriatic arthritis. [14] Only five case reports have previously described LA located in subdeltoid bursa in the literature. [7],[15],[16],[17],[18] Four cases among them were associated with rotator cuff tears. [7],[15],[16],[18] A significant finding in our case was the coexistence of intermuscular lipoma, SLAP lesion and labral cyst. It is not clear whether pathologic lesions such as rotator cuff tears, SLAP lesion, labral cyst or lipoma, cause LA in subdeltoid bursa, or they are merely coincidental.
Ikushima et al. have hypothesized that LA could be a reaction of the synovial tissue involving adipose differentiation. Similarly, synovial chondromatosis is a more frequent form of osteochondral differentiation, suggesting a common etiology of these two synovial disorders. [19] Recent studies have noted an inverse relation between adipocyte differentiation and the osteogenic activity of bone marrow stromal cells [20] and that it is reciprocally regulated by bone mophogenetic proteins. [21] Two case reports published by Kurihashi et al. and Vilanova et al. have described presence of LA with osseous/chondroid differentiation together in the knee joint bursa. [18],[22] It is reasonable to presume that the neoplastic transformation occurs at the multipotential undifferentiated mesenchymal cellular level that later differentiates into lipoblasts, chondroblasts and/or osteoblasts. This may have led to differentiation of both adipose and osseous/chondroid tissues simultaneously in our case.
 References References | |  |
| 1. | In Y, Chun KA, Chang ED, Lee SM. Lipoma arborescens of the glenohumeral joint: A possible cause of osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2008;16:794-6. 
|
| 2. | Hubscher O, Costanza E, Elsner B. Chronic monoarthritis due to lipoma arborescens. J Rheumatol 1990;17:861-2. 
|
| 3. | Dinauer P, Bojescul JA, Kaplan KJ, Litts C. Bilateral lipoma arborescens of the bicipitoradial bursa. Skeletal Radiol 2002;31:661-5. 
|
| 4. | Hill GN, Phyo N. Extra-articular lipoma arborescens of the hand: An unusual case report. J Hand Surg Eur Vol 2011;36:422-3. 
|
| 5. | Huang GS, Lee HS, Hsu YC, Kao HW, Lee HH, Chen CY. Tenosynovial lipoma arborescens of the ankle in a child. Skeletal Radiol 2006;35:244-7. 
|
| 6. | Murphey MD, Carroll JF, Flemming DJ, Pope TL, Gannon FH, Kransdorf MJ. From the archives of the AFIP: Benign musculoskeletal lipomatous lesions. Radiographics 2004;24:1433-66. 
|
| 7. | Dawson JS, Dowling F, Preston BJ, Neumann L. Case report: Lipoma arborescens of the sub-deltoid bursa. Br J Radiol 1995;68:197-9. 
|
| 8. | Hallel T, Lew S, Bansal M. Villous lipomatous proliferation of the synovial membrane (lipoma arborescens). J Bone Joint Surg Am 1988;70:264-70. 
|
| 9. | Kim RS, Song JS, Park SW, Kim L, Park SR, Jung JH, et al. Lipoma arborescens of the knee. Arthroscopy 2004;20:e95-9. 
|
| 10. | Ryu KN, Jaovisidha S, Schweitzer M, Motta AO, Resnick D. MR imaging of lipoma arborescens of the knee joint. AJR Am J Roentgenol 1996;167:1229-32. 
|
| 11. | Marui T, Yamamoto T, Kimura T, Akisue T, Nagira K, Nakatani T, et al. A true intra-articular lipoma of the knee in a girl. Arthroscopy 2002;18:E24. 
|
| 12. | Adelani MA, Wupperman RM, Holt GE. Benign synovial disorders. J Am Acad Orthop Surg 2008;16:268-75. 
|
| 13. | Santiago M, Passos AS, Medeiros AF, Sá D, Correia Silva TM, Fernandes JL. Polyarticular lipoma arborescens with inflammatory synovitis. J Clin Rheumatol 2009;15:306-8. 
|
| 14. | Fraser AR, Perry ME, Crilly A, Reilly JH, Hueber AJ, McInnes IB. Lipoma arborescens co-existing with psoriatic arthritis releases tumour necrosis factor alpha and matrix metalloproteinase 3. Ann Rheum Dis 2010;69:776-7. 
|
| 15. | Laorr A, Peterfy CG, Tirman PF, Rabassa AE. Lipoma arborescens of the shoulder: Magnetic resonance imaging findings. Can Assoc Radiol J 1995;46:311-3. 
|
| 16. | Nisolle JF, Blouard E, Baudrez V, Boutsen Y, De Cloedt P, Esselinckx W. Subacromial-subdeltoid lipoma arborescens associated with a rotator cuff tear. Skeletal Radiol 1999; 28:283-5. 
|
| 17. | Pandey T, Alkhulaifi Y. Bilateral lipoma arborescens of the subdeltoid bursa. Australas Radiol 2006;50:487-9. 
|
| 18. | Vilanova JC, Barceló J, Villalón M, Aldomà J, Delgado E, Zapater I. MR imaging of lipoma arborescens and the associated lesions. Skeletal Radiol 2003;32:504-9. 
|
| 19. | Ikushima K, Ueda T, Kudawara I, Yoshikawa H. Lipoma arborescens of the knee as a possible cause of osteoarthrosis. Orthopedics 2001;24:603-5. 
|
| 20. | Beresford JN, Bennett JH, Devlin C, Leboy PS, Owen ME. Evidence for an inverse relationship between the differentiation of adipocytic and osteogenic cells in rat marrow stromal cell cultures. J Cell Sci 1992;102:341-51. 
|
| 21. | Gimble JM, Morgan C, Kelly K, Wu X, Dandapani V, Wang CS, et al. Bone morphogenetic proteins inhibit adipocyte differentiation by bone marrow stromal cells. J Cell Biochem 1995;58:393-402. 
|
| 22. | Kurihashi A, Yamaguchi T, Tamal K, Saotome K. Lipoma arborescens with osteochondral metaplasia - A case mimicking synovial osteochondromatosis in a lateral knee bursa. Acta Orthop Scand 1997;68:304-6. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|
