| |


 |
| Year : 2013 | Volume
: 7
| Issue : 4 | Page : 143-148 |
|
|
|
|
|
CASE REPORT Management of failed metal-backed glenoid component in patients with bilateral total shoulder arthroplasty
Xinning Li1, Josef K Eichinger2, Laurence D Higgins3
1 Assistant Professor, Sports Medicine and Shoulder and Elbow Surgery, Department of Orthopaedics, Boston University School of Medicine, 720 Harrison Avenue - Suite #808, Boston, MA 02118, USA
2 Assistant Professor of Surgery, Chief of Shoulder & Elbow Surgery, Madigan Army Medical Center, Tacoma, WA 98431, USA
3 Assistant Professor, Chief of the Sports Medicine and Shoulder Service. Harvard Medical School. Brigham and Women's Hospital, Boston, MA, USA
Correspondence Address:
Xinning Li
Assistant Professor, Sports Medicine and Shoulder and Elbow Surgery, Department of Orthopaedics, Boston University School of Medicine, 720 Harrison Avenue - Suite #808, Boston, MA 02118
USA
 Source of Support: None, Conflict of Interest: None  | 1 |
DOI: 10.4103/0973-6042.123527

|
|
|
|
| Date of Web Publication | 24-Dec-2013 |
 Abstract Abstract | | |
Total shoulder arthroplasty (TSA) is successful in providing pain relief and functional improvements for patients with shoulder arthritis. Outcomes are directly correlated with implant position and fixation, which ultimately affects wear and longevity. Metal-backed glenoid components were introduced as an alternative to the standard cemented glenoid fixation. Early loosening and cavitary glenoid bone loss has been reported as a major complication associated with these metal-backed glenoids, which presents the surgeon with a challenging revision situation. Furthermore, failure of bilateral TSA in patients with metal-backed glenoids is extremely rare. We present two patients with early failure of bilateral TSA secondary to loosening of the metal-backed glenoids. Both patients had significant glenoid bone loss and were treated with four different types of revision techniques. A description of treatments and outcomes of both patients are reported along with the simple shoulder test and American Shoulder and Elbow Surgeons scores. One patient underwent revision to bilateral reverse prosthesis and experienced a much-improved outcome in comparison to the patient revised to a hemiarthroplasty and resection arthroplasty, for each shoulder respectively. In patients who present with failed TSA, revision to a reverse prosthesis with or without staged glenoid bone graft should be considered as an option of treatment. It is also important to rule out infection with intraoperative tissue biopsy before proceeding to revision surgery. However, in patients with catastrophic glenoid bone loss, both hemiarthroplasty and resection arthroplasty can provide an alternative treatment option, but they are associated with a poorer functional outcome and pain relief.
Keywords: Custom reverse, hemiarthroplasty, illiac crest bone graft, reverse shoulder arthroplasty, revision, total shoulder arthroplasty
How to cite this article:
Li X, Eichinger JK, Higgins LD. Management of failed metal-backed glenoid component in patients with bilateral total shoulder arthroplasty. Int J Shoulder Surg 2013;7:143-8 |
 Introduction Introduction | |  |
Total shoulder arthroplasty (TSA) is a reliable procedure for pain relief with good to excellent outcomes in patients with arthritis. [1] The most common reason for failure of TSA is loosening of the glenoid component with subsequent glenoid bone loss. [2] Several different designs of glenoid components have been utilized in TSA and can be categorized into two basic categories: All-polyethylene (PE) glenoid component or metal-backed designs consisting of a metal implant fixed directly onto the glenoid with a snap-in PE component. [3] Metal-backed glenoid components; however, have resulted in a higher rate of loosening than that of traditional cemented PE components in several series. [4],[5],[6] Metal-backed glenoids were first introduced as an alternative to cemented PE components according to the theory that a metal in-growth component would result in a lower incidence of loosening. [3] Additional metal screws were also incorporated into the metal-backed components to further augment the fixation onto the glenoid. Unfortunately, as the previous outcome studies identified, a number of these metal-backed implants ultimately failed and requiring revision surgery. Revision surgery in this scenario is difficult, but good results can be obtained when converting a failed anatomical shoulder arthroplasty with glenoid loosening to a reverse shoulder arthroplasty. [7] Other complicating factors in revision shoulder surgery include the presence of latent infection and bone loss from both glenoid and humerus. Managing these failed TSA scenarios may require staged surgical procedures to eradicate the infection and restore glenoid bone integrity/stability, etc., through bone grafting procedures.
Management of a failed anatomic unconstrained TSA presents a challenging problem. Failure of bilateral TSA secondary to metal-backed glenoid component loosening is extremely rare and difficult to manage. We present two patients with failed bilateral total shoulder arthroplasties and their treatments and outcomes.
 Case Reports Case Reports | |  |
Case 1
An 80-year-old male presented with a history of bilateral glenohumeral arthritis status post-bilateral total shoulder replacements (left shoulder in 1996 and right shoulder in 1997). Both shoulders were replaced with the Kirschner modular II-C components (Kirschner Medical Corp., Fair Lawn, New Jersey), which is comprised of a modular humeral head/proximal porous coated stem and a metal-backed pressed fitted glenoid component with proximal and distal interlocking fixation screws. Patient experienced a routine intraoperative and post-operative course after both shoulder replacements without any complications.
In terms of the left shoulder, patient reported a few years of good pain relief and functional improvements after the shoulder replacement. However, he started to have intermittent left shoulder pain about 3 years after surgery that progressed to constant pain and significant limitation in terms of his range of motion and also functional activities. On physical examination, his forward flexion (FF) was 0-60, external rotation (ER) of 0-15 and internal rotation to his back pocket only. He also had significant pain with any range of motion on examination. Strength testing demonstrated 4/5 in supraspinatus and 4/5 in ER. Anteroposterior radiograph of the left shoulder showed significant loosening of the metal-backed glenoid component and cavitary bone loss with failure of fixation of both screws [Figure 1]b. Computed tomography scan confirms the massive bone loss in the glenoid with associated rotator cuff tear. Due to the significant glenoid bone loss, patient underwent a resection arthroplasty in 2010 (14 years from the original procedure). At the most recent follow-up (2012), patient had no pain on the left shoulder. His range of motion measurements were: FF [8] = 0-90, abduction = 0-50, ER = 0-45 [Figure 2]. Radiographs revealed of the resection arthroplasty revealed a small amount of heterotopic bone formation around the humeral shaft [Figure 1]d.
His simple shoulder test (SST) score was 16 and American Shoulder and Elbow Surgeons (ASES) score was 23.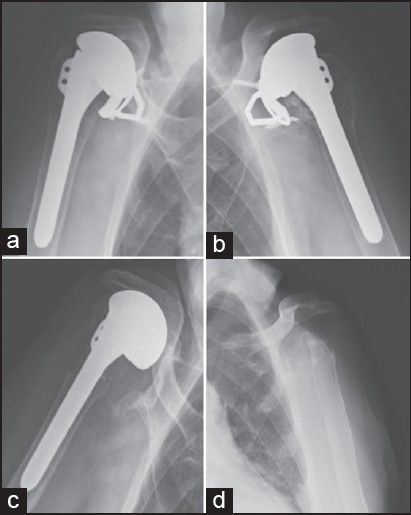 | Figure 1: Anteroposterior radiograph of the patient in case one with the right (a) and left (b) shoulder showing the failed bilateral metalbacked glenoids. The right shoulder was revised to a large head hemiarthroplasty (c) and the left shoulder was revised with resection arthroplasty (1d)
Click here to view |
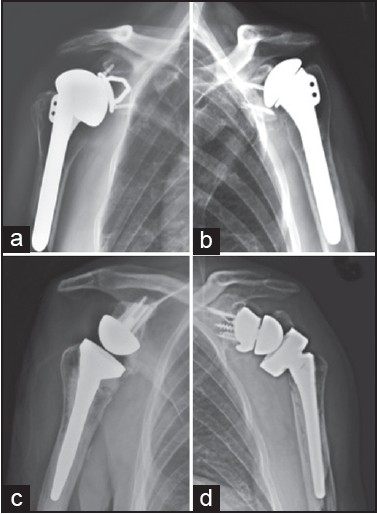 | Figure 2: Anteroposterior radiograph of patient in case two with the right (a) and left (b) shoulder showing the failed bilateral metal-backed glenoids. The right shoulder was revised to a reverse arthroplasty (c) and the left shoulder was revised with a custom reverse arthroplasty after staged glenoid bone grafting with iliac crest autograft (d)
Click here to view |
On the right shoulder, patient also reported progressive intermittent pain that started about 4-5 years after the initial procedure. This also progressed to constant pain and significant limitations of his activities of daily living. On physical examination, patient range of motion was FF = 0-90 passive and 0-30 active, ER = 0-20 and internal rotation (IR) to the back pocket only. Patient also demonstrated significant weakness with supraspinatus and ER strength testing. Radiographs revealed failure of the metal-backed glenoid with obvious radiolucency indicating lysis around the glenoid component [Figure 1]a. Patient underwent a revision arthroplasty to a large head hemiarthroplasty (2012) with removal of both failed metal-backed glenoid and the loose humeral stem. At the time of surgery, it was noted that the PE was worn with resulting metal on metal articulation and metallosis of the soft-tissue around the failed glenoid component. At the most recent follow-up (7 months post-op), range of motion was: FF = 0-70, abduction = 0-50 and ER = 0-65 [Figure 2]. He reports minimal pain on the right; however, he does have limitations of his daily activities due to his decreased range of motion. Radiographs demonstrate superior migration of the hemiarthroplasty without evidence of loosening [Figure 1]c. His outcome scores included a SST score of 16 and an ASES score of 25.
Case 2
A 75-year-old male presented to the clinic with a history hemochromatosis and bilateral glenohumeral arthritis status post-bilateral total shoulder replacements (left shoulder in 1999 and right shoulder in 2002). Both shoulders were also replaced with the Kirschner modular II-C components (Kirschner Medical Corp., Fair Lawn, New Jersey, USA).
In terms of the left shoulder, patient reported several years of good pain relief and functional improvements after the shoulder replacement. However, he started to have intermittent left shoulder pain about 8 years after surgery that progressed to constant pain and significant limitation in terms of his range of motion and also functional activities. On physical examination, his FF was 0-80, ER of 0-45 and internal rotation to L3. He also had significant pain with any range of motion on examination and strength testing demonstrated 4+/5 in supraspinatus and 4−/5 in ER. Anteroposterior radiograph of the left shoulder showed catastrophic failure of the metal-backed glenoid component with breakage of both screws [Figure 3]b. Given the pain and functional impairment, the patient underwent revision arthroplasty with removal of the metal-backed glenoid and humeral components. Intraoperatively, significant metallosis was encountered. In addition, there was a concern for infection. Intraoperative frozen section indicated acute inflammatory reaction with a high WBC seen on the high-powered field. Based on the high probability of a coexistent infection, a decision was made to place prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) antibiotic humeral component and bone graft the glenoid cavitary defect with iliac crest autograft bone graft. Subsequently, intraoperative cultures grew both Methicillin-resistant Staphylococcus aureus (MRSA) and Propionibacterium acnes. Patient was treated with 8 weeks of intravenous antibiotics and Peripherally Inserted Central Catheter (PICC) line. Arthroscopic biopsy was then performed and demonstrated no evidence of persistent infection. Patient underwent revision arthroplasty to a custom reverse prosthesis component (Biomet comprehensive custom reverse prosthesis, Warsaw, IN) in 2008. Patient tolerated the procedure well with no intraoperative or post-operative complications. On the most recent follow-up (2012), patient had no pain on the left shoulder. His range of motion measurements were: FF = 0-170, abduction = 0-95, ER = 0-30 [Figure 4]. Radiographs revealed the custom reverse prosthesis was stable without evidence of loosening or failure [Figure 3]d. His SST and ASES measured 83 and 78 respectively.
On the right shoulder, patient also reported progressive intermittent pain that started about 6 years after the initial procedure. This progressed to constant pain and significant limitations on the overall range of motion. On physical exam, patient's range of motion was: FF = 0-60 passive, ER = 0-20 and IR to the side only. He also had significant weakness with supraspinatus and ER testing. Radiographs revealed lucency behind the metal-backed glenoid without failure of the two screws as well as marked decrease in the space between the humeral head and metal-backed glenoid indicating wear [Figure 3]a. Patient underwent revision arthroplasty with removal of the glenoid component and humeral modular head. An intraoperative biopsy was also obtained, which was positive for P. Acnes and subsequent placement of a PROSTALAC spacer was performed. Furthermore, he had a prolonged course of IV penicillin via PICC line. In 2010, patient underwent a revision arthroplasty with reverse shoulder prosthesis (Tornier Aequalis Reverse system. Bloomington, MN) and iliac crest bone graft of the glenoid. Harvesting of the iliac crest was performed with an oscillating saw and a 3 cm × 3 cm tri-cortical crest was obtained. The iliac crest was shaped to fit the glenoid defect and the metaglene was fixed onto the crest and native glenoid with a central plug and two compression screws. Patient tolerated the procedure well with no intraoperative or post-operative complications. On the most recent follow-up (2 years post-op), range of motion: FF = 0-120, abduction = 0-80, ER 0-75 and IR to back pocket [Figure 4]. He reports minimal pain on the right and no limitations to his activities of daily living. Radiographs demonstrate the reverse prosthesis in a good position without evidence of loosening or failure [Figure 3]c. His SST and ASES scores measured 100 and 88 points respectively.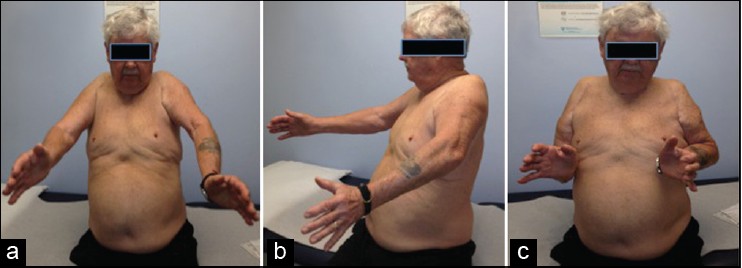 | Figure 3: Clinical photograph of the patient in case one demonstrating limited range of motion in forward flexion (a and b) and external rotation (c). On the right shoulder, patient had a revision to a large head hemiarthroplasty and on the left shoulder; patient had a resection arthroplasty
Click here to view |
 | Figure 4: Clinical photograph of the patient in case two demonstrating excellent range of motion in forward flexion (a and b) and external rotation (c). On the right shoulder, patient had a revision to a reverse arthroplasty and on the left shoulder; patient had a staged glenoid bone graft and subsequent revision to a custom reverse prosthesis
Click here to view |
 Discussion Discussion | |  |
The overall number of TSA performed in the United States for degenerative pathologies affecting the shoulder joint have increased dramatically over the last decade. [9] Survival analysis of 2588 TSA's from the Mayo clinic projected a prosthetic survival of 94.2% at 5 years, 90.2% at 10 years and 81.4% at 20 years. The incidence of revision shoulder arthroplasty relating to the initial procedure was 8.2% or 212 TSA. [10] Failure of anatomical shoulder arthroplasty can be from a myriad of reasons, with the most common reason being glenoid loosening. [11],[12] In particular, metal-backed glenoid components fail at a higher rate than that of cemented all PE glenoids and may be related to the fact that the PE component experiences greater amounts of stress when analyzed experimentally using finite element analysis. [13] In a series of 42 TSAs with symptomatic failed glenoids requiring revision surgery, 32 or 76% were metal-backed glenoids. [12] The main mode of failure in an all-PE glenoid component is aseptic loosening, whereas in a metal-back glenoid design, failure may also be related to PE liner wear and dissociation. [5],[12],[14] Despite the poor outcomes for metal-backed glenoids, newer designs are being introduced with different materials comprised of porous coating, such as trabecular metals. Unfortunately, even the newer trabecular metal designs appear to be subject to higher failure rates. [15]
Failure or loosening of the glenoid component in anatomical shoulder arthroplasty almost universally results in glenoid bone loss. [16],[17] Options for revision surgery in the setting of a failed glenoid with significant bone loss are varied and include removal of the loose glenoid without re-implantation (hemiarthroplasty), re-implantation of another glenoid component with or without staged bone grafting, revision to a reverse shoulder arthroplasty and resection arthroplasty. [3],[6],[12],[17],[18],[19] Bonnevialle et al. [12] reported the results of all PE glenoid re-implantation in a series of failed TSA and at the final follow-up of 74 months, 7 patients (17%) had re-revision and another additional 50% of patients showed radiographic loosening of the cemented all-PE glenoid component. Thus, the authors concluded that revision of a TSA with re-implantation of an all-PE cemented glenoid component does not solve the problem of glenoid loosening with bone loss. Both hemiarthroplasty and resection arthroplasty have been indicated for failed TSA and associated with poor functional outcomes and patient satisfaction in the literature. [11],[20],[21],[22],[23] In our first patient, there was massive glenoid bone loss and metallosis associated with the metal-backed glenoids. Thus, our surgical options were limited and the decision was made to proceed with a large-head hemiarthroplasty and resection arthroplasty for the right and left shoulder, respectively. At the most recent follow-up, patient reported limitation in range of motion of both shoulders and also low SST and ASES scores.
Modern day reverse total shoulder arthroplasty (rTSA) was designed in Europe in 1985 for indications of rotator cuff tear arthropathy associated with pseudoparesis of the shoulder. [24] The FDA recently approved this prosthesis for use in the United States in 2004. As surgeons gain more experience with the rTSA, the indications have expanded to the treatment of the proximal humerus fractures in the elderly and also for failed TSA. [25],[26] Although utilizing the rTSA for a failed TSA is a viable option, the surgeon must be cognizant of the high complication rates associate with the rTSA. [27] In our second patient, we elected to convert his failed TSA to a reverse arthroplasty. On the left shoulder, there was significant glenoid bone loss; thus, we performed a staged procedure with iliac crest bone graft and revision with a custom reverse prosthesis after bone incorporation. One the right side, even with the glenoid bone loss, we were able to perform a single staged revision with iliac crest bone graft after eradication of the infection. Patient at the final follow-up had significant improvement in his range of motion and also function (ASES and SST (Simple Shoulder Test)). Patel et al.[18] evaluated 31 patients with rTSA for a failed TSA and reported significant improvement in their functional outcome (UCLA, ASES, SST and VAS) and decrease in pain with a 5 year follow-up period. Ortmaier et al.[8] also reported similar findings in a series of 57 patients that had revision of failed TSAs to a reverse prosthesis. With an average follow-up of 51 months, all functional outcome scores improved (Constant-Murley, UCLA, SST) with high patient satisfaction.
Factors to carefully consider and evaluate in the setting of failed TSA are, first and foremost, patient factors (age, occupation, health status and desired activity level), presence of infection, severity of glenoid bone loss, status of the rotator cuff and the types of components present [Table 1]. The evaluation of the humeral stem and assessment of the modularity and ability to retain the stem are particularly important considerations in accommodating a reverse prosthesis. For patients with bilateral failed anatomical shoulder arthroplasty, a step-wise, critical assessment is crucial. First, a thorough evaluation of infection must be performed. If infection is confirmed through pre-operative analysis through laboratory and aspiration then a debridement and removal of prosthetic components is performed. While a PROSTALAC spacer has provided satisfactory outcomes, some patients may desire a revision reconstruction. [28] If infection is suspected intraoperatively, additional cultures, frozen section and immediate, intraoperative gram stain and white blood cell counts under high powered field may be utilized in the decision making process. [29] Another critical step in evaluation is that of the glenoid bone stock. More than likely some level of bone loss is present that requires bone grafting. Given the difficulty of performing revision with an anatomical shoulder arthroplasty in the setting of glenoid bone loss, reverse shoulder arthroplasty represents a likely superior method as bone grafting in conjunction with the placement of a glenoid baseplate can allow for a potentially single stage revision procedure. [19] Because the native humeral head is absent in the revision setting, several alternatives and techniques have been described including using autograft iliac crest and allograft femoral neck. [19],[30] 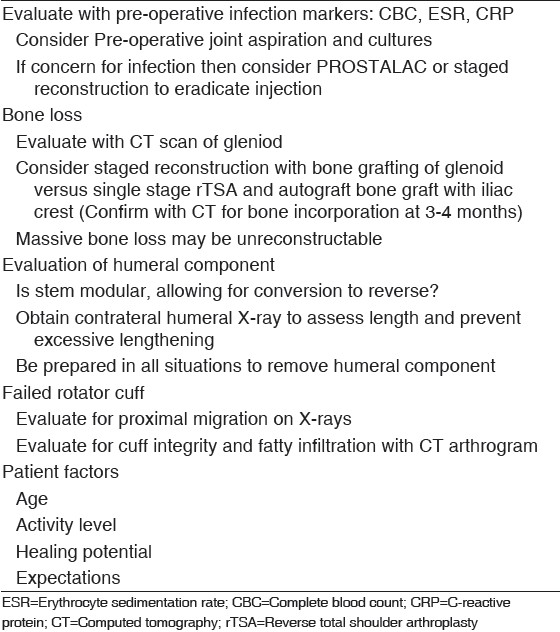 | Table 1: Evaluation and surgical planning factors for revision surgery in the setting of failed shoulder arthroplasty
Click here to view |
 Conclusion Conclusion | |  |
Bilateral failed TSA is a rare problem. Metal-backed glenoids have a high failure rate and represent a difficult subset of revision cases due to the glenoid bone loss. Multiple treatment options are possible, but careful consideration based on multiple factors must be performed. Conversion to a reverse shoulder arthroplasty resulted in better functional results in comparison to resection arthroplasty and conversion to hemiarthroplasty particularly in the two patients that presented with failed bilateral anatomic shoulder arthroplasties.
 References References | |  |
| 1. | Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Némoz C, et al. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: Results of a multicenter study. J Shoulder Elbow Surg 2003;12:207-13. 
|
| 2. | Gonzalez JF, Alami GB, Baque F, Walch G, Boileau P. Complications of unconstrained shoulder prostheses. J Shoulder Elbow Surg 2011;20:666-82. 
[PUBMED] |
| 3. | Namdari S, Goel DP, Romanowski J, Glaser D, Warner JJ. Principles of glenoid component design and strategies for managing glenoid bone loss in revision shoulder arthroplasty in the absence of infection and rotator cuff tear. J Shoulder Elbow Surg 2011;20:1016-24. 
[PUBMED] |
| 4. | Boileau P, Avidor C, Krishnan SG, Walch G, Kempf JF, Molé D. Cemented polyethylene versus uncemented metal-backed glenoid components in total shoulder arthroplasty: A prospective, double-blind, randomized study. J Shoulder Elbow Surg 2002;11:351-9. 
|
| 5. | Fox TJ, Cil A, Sperling JW, Sanchez-Sotelo J, Schleck CD, Cofield RH. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg 2009;18:859-63. 
[PUBMED] |
| 6. | Taunton MJ, McIntosh AL, Sperling JW, Cofield RH. Total shoulder arthroplasty with a metal-backed, bone-ingrowth glenoid component. Medium to long-term results. J Bone Joint Surg Am 2008;90:2180-8. 
[PUBMED] |
| 7. | Melis B, Bonnevialle N, Neyton L, Lévigne C, Favard L, Walch G, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: Is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg 2012;21:342-9. 
|
| 8. | Ortmaier R, Resch H, Matis N, Blocher M, Auffarth A, Mayer M, et al. Reverse shoulder arthroplasty in revision of failed shoulder arthroplasty-outcome and follow-up. Int Orthop 2013;37:67-75. 
[PUBMED] |
| 9. | Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg 2010;19:1115-20. 
[PUBMED] |
| 10. | Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: Analysis of 2588 shoulders over three decades (1976 to 2008). J Bone Joint Surg Br 2011;93:1513-7. 
[PUBMED] |
| 11. | Hasan SS, Leith JM, Campbell B, Kapil R, Smith KL, Matsen FA 3 rd . Characteristics of unsatisfactory shoulder arthroplasties. J Shoulder Elbow Surg 2002;11:431-41. 
|
| 12. | Bonnevialle N, Melis B, Neyton L, Favard L, Molé D, Walch G, et al. Aseptic glenoid loosening or failure in total shoulder arthroplasty: Revision with glenoid reimplantation. J Shoulder Elbow Surg 2013;22:745-51. 
|
| 13. | Stone KD, Grabowski JJ, Cofield RH, Morrey BF, An KN. Stress analyses of glenoid components in total shoulder arthroplasty. J Shoulder Elbow Surg 1999;8:151-8. 
[PUBMED] |
| 14. | Kasten P, Pape G, Raiss P, Bruckner T, Rickert M, Zeifang F, et al. Mid-term survivorship analysis of a shoulder replacement with a keeled glenoid and a modern cementing technique. J Bone Joint Surg Br 2010;92:387-92. 
[PUBMED] |
| 15. | Budge MD, Nolan EM, Heisey MH, Baker K, Wiater JM. Results of total shoulder arthroplasty with a monoblock porous tantalum glenoid component: A prospective minimum 2-year follow-up study. J Shoulder Elbow Surg 2013;22:535-41. 
|
| 16. | Deutsch A, Abboud JA, Kelly J, Mody M, Norris T, Ramsey ML, et al. Clinical results of revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg 2007;16:706-16. 
[PUBMED] |
| 17. | Neyton L, Sirveaux F, Roche O, Molé D, Boileau P, Walch G. Results of revision surgery for glenoid loosening: A multicentric series of 37 shoulder prosthesis. Rev Chir Orthop Reparatrice Appar Mot 2004;90:111-21. 
|
| 18. | Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg 2012;21:1478-83. 
[PUBMED] |
| 19. | Kelly JD 2 nd , Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg 2012;21:1516-25. 
|
| 20. | Braman JP, Sprague M, Bishop J, Lo IK, Lee EW, Flatow EL. The outcome of resection shoulder arthroplasty for recalcitrant shoulder infections. J Shoulder Elbow Surg 2006;15:549-53. 
[PUBMED] |
| 21. | Cofield RH. Shoulder arthrodesis and resection arthroplasty. Instr Course Lect 1985;34:268-77. 
[PUBMED] |
| 22. | Hax PM, Hörster G. Alloarthroplasty, resection-arthroplasty and arthrodesis of the shoulder-joint - Indications and technic (author′s transl). Unfallchirurgie 1980;6:245-9. 
|
| 23. | Sperling JW, Cofield RH, Rowland CM. Minimum fifteen-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elbow Surg 2004;13:604-13. 
[PUBMED] |
| 24. | Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: Design, rationale, and biomechanics. J Shoulder Elbow Surg 2005;14:147S-61. 
[PUBMED] |
| 25. | Wall B, Nové-Josserand L, O′Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: A review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85. 
|
| 26. | Garrigues GE, Johnston PS, Pepe MD, Tucker BS, Ramsey ML, Austin LS. Hemiarthroplasty versus reverse total shoulder arthroplasty for acute proximal humerus fractures in elderly patients. Orthopedics 2012;35:e703-8. 
[PUBMED] |
| 27. | Kempton LB, Ankerson E, Wiater JM. A complication-based learning curve from 200 reverse shoulder arthroplasties. Clin Orthop Relat Res 2011;469:2496-504. 
|
| 28. | Jawa A, Shi L, O′Brien T, Wells J, Higgins L, Macy J, et al. Prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) use for the treatment of infection after shoulder arthroplasty. J Bone Joint Surg Am 2011;93:2001-9. 
[PUBMED] |
| 29. | Morman M, Fowler RL, Sanofsky B, Higgins LD. Arthroscopic tissue biopsy for evaluation of infection before revision arthroplasty. J Shoulder Elbow Surg 2011;20:e15-22. 
[PUBMED] |
| 30. | Bateman E, Donald SM. Reconstruction of massive uncontained glenoid defects using a combined autograft-allograft construct with reverse shoulder arthroplasty: Preliminary results. J Shoulder Elbow Surg 2012;21:925-34. 
[PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1]
|
