| |


 |
| Year : 2014 | Volume
: 8
| Issue : 3 | Page : 65-71 |
|
|
|
|
|
ORIGINAL ARTICLE Decreased scapular notching with lateralization and inferior baseplate placement in reverse shoulder arthroplasty with high humeral inclination
Brian T Feeley, Alan L Zhang, Jeffery J Barry, Edward Shin, Julianne Ho, Ehsan Tabaraee, C Benjamin Ma
Department of Orthopaedic Surgery, University of California, San Francisco, CA, USA
Correspondence Address:
Brian T Feeley
1500 Owens Ave, Box 3004, San Francisco, CA 94158
USA
 Source of Support: Dr. Ma received educational support and research support from Zimmer, Inc., Conflict of Interest: None
DOI: 10.4103/0973-6042.140112
Clinical trial registration 10-02764

|
|
|
|
| Date of Web Publication | 4-Sep-2014 |
 Abstract Abstract | | |
Background: Scapular notching is a radiographic finding of unknown clinical significance following reverse total shoulder arthroplasty (RTSA). The purpose of this study was to determine how baseplate position affects the incidence of scapular notching and measure the clinical outcomes.
Hypothesis: We hypothesized that low base plate position on the glenoid and new prosthesis design with a higher humeral inclination angle would decrease the incidence of notching at 2 years follow-up.
Materials and methods: A total of 54 patients with an average follow-up of 30 months met inclusion criteria and underwent radiographic analysis of scapular notching and radiographic measures to determine glenoid component placement. Clinical measures including visual analog score, American Shoulder and Elbow Surgeons (ASES) scores, and range of motion (ROM) were prospectively collected.
Results: Thirty-nine of the 54 patients had no notching. 7 had Grade 1 notching, 7 had Grade 2 notching, one had Grade 3, and one had Grade 4 notching. Notching was associated with higher placement of the glenoid component as measured by peg-glenoid rim distance and base plate distance. All patients with no evidence of notching at 1-year, continued to have no notching after multi-year follow-up. Clinical outcome measures including ASES scores, ROM, and visual analog pain scores were improved at follow-up.
Conclusion: We concluded that lower neck-shaft angle and low baseplate positioning led to a low incidence of significant scapular notching as only 6 out of 57 (16%) patients had notching Grade 2 and above. At short-term follow-up, this RTSA results in excellent clinical outcomes and a significantly lower scapular notching rate than traditional techniques.
Keywords: Reverse shoulder arthroplasty, rotator cuff arthropathy, scapular notching
How to cite this article:
Feeley BT, Zhang AL, Barry JJ, Shin E, Ho J, Tabaraee E, Ma C B. Decreased scapular notching with lateralization and inferior baseplate placement in reverse shoulder arthroplasty with high humeral inclination. Int J Shoulder Surg 2014;8:65-71 |
How to cite this URL:
Feeley BT, Zhang AL, Barry JJ, Shin E, Ho J, Tabaraee E, Ma C B. Decreased scapular notching with lateralization and inferior baseplate placement in reverse shoulder arthroplasty with high humeral inclination. Int J Shoulder Surg [serial online] 2014 [cited 2016 Aug 23];8:65-71. Available from: http://www.internationalshoulderjournal.org/text.asp?2014/8/3/65/140112 |
 Introduction Introduction | |  |
Reverse total shoulder arthroplasty (RTSA) has gained popularity for the treatment of many complex shoulder problems including massive rotator cuff tears and revision procedures with an incompetent or poorly functioning rotator cuff. [1],[2],[3],[4] Although initial complication rates were high, [5],[6],[7],[8],[9],[10] improvements in design and surgeons' experience have decreased the frequency of complications. [11],[12],[13],[14]
One of the most common radiographic findings seen following RTSA is the development of scapular notching. [15],[16] Notching is thought to be due to the medicalization and lowering of the center of rotation, which causes impingement of the medial aspect of the humeral component at the lateral border of the scapula. The clinical significance of notching is not fully defined with a limited number of studies reporting on long-term patient outcomes. [16],[17],[18],[19] Although these studies do not show significant functional compromise with early notching, advanced notching has been correlated with loosening of the glenosphere and component failures. [17] Initial implant designs had a high rate of notching, with some studies showing up to 96%. [15],[18] More recent designs and surgical techniques have decreased this, with some authors recommending positioning the glenosphere under the inferior margin of the glenoid. [19],[20],[21]
The primary purpose of this study was to determine the incidence of notching in lateralized and lower neck-shaft angle prosthesis in a consecutive series of patients that underwent RTSA. The secondary purpose was to correlate the presence of notching with changes in clinical outcome. We hypothesized that lower placement of the baseplate would correlate with a lower incidence of scapular notching. We also hypothesized that notching would lead to higher pain scores with lower satisfaction scores.
 Patients and methods Patients and methods | |  |
This is a retrospective study performed as part of a prospective follow-up of all patients who underwent shoulder arthroplasty procedures by two surgeons from 2007 to 2011. The study received approval from the institutional review board. Inclusion and exclusion criteria are listed in [Table 1].
Surgical protocol
The patient was positioned in a semi-beach chair position. A standard deltopectoral approach was utilized. A higher humeral inclination angle (35°) and 3 mm lateral offset of the glenosphere prosthesis was used (Zimmer Reverse Trabecular Metal System) for every patient. The humeral component was prepared for a cemented stem with approximately 10-20° of retroversion. The glenoid was performed with the goal of the glenosphere to be placed at the inferior aspect of the glenoid. We used round flat, trabecular metal backed baseplates. We did not place the baseplate with any significant inferior tilt and all baseplates used were 28 mm with 36 mm glenospheres. Two locking screws were aimed to be at approximately 12 o'clock and 6 o'clock position on the glenoid face or at the superior and inferior margins, respectively. The patient was paralyzed for trial and final reduction to assure a tight fit between the components. All patients had an ultra-high molecular weight polyethylene liner. Postoperatively, the patient was kept in a sling for 6 weeks with physical therapy starting after 6 weeks with no further restrictions on movement. Strengthening occurs at 12 weeks postoperatively.
Radiographic evaluations
Radiographic evaluation was performed at the preoperative visit, and at sequential postoperative visits. Standard anteroposterior (AP) of the shoulder, AP of the glenohumeral joint, and axillary views were obtained. In order to assess inferior and posterior notching, the AP of the glenohumeral joint and axillary view were evaluated at each visit by two independent evaluators. Notching was classified similar to the classification of Sirveaux et al. [6] with the only change being that a Grade 1 notch did not have to enter the baseplate area [Figure 1]. Other factors that were evaluated were the peg-glenoid rim distance (PGRD), which measures the distance from the superior aspect of the peg to the inferior aspect of the glenoid, the prosthesis-scapular neck angle (PSNA), and the base plate distance (BPD) [Figure 2], the distance from the inferior aspect of the base plate to the inferior rim of the glenoid. The radiographs were reviewed by two independent reviewers for inter- and intra-observer reliability.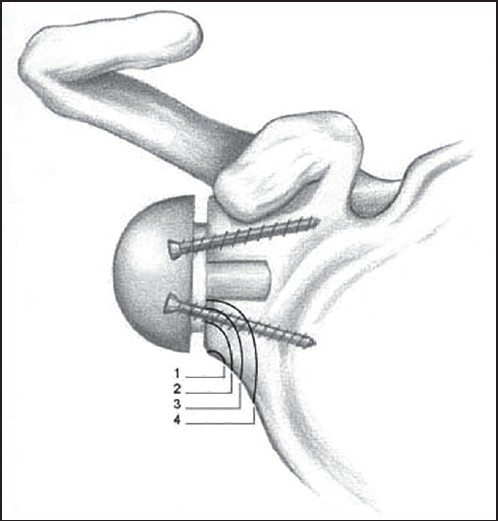 | Figure 1: Notching classification similar to the classification described by Sirveaux et al.[6] In the current study, a Grade 1 notch did not enter the baseplate, but did in the original description
Click here to view |
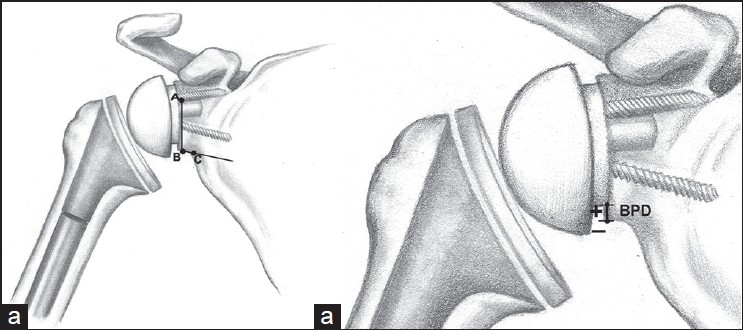 | Figure 2: (a) Measurement of prosthesis-scapular neck angle (PSNA) and peg-glenoid rim distance (PGRD). The distance from A to B is the PGRD, and the angle AB to BC is the PSNA. (b) Measurement of base plate distance. Positive numbers denote placement of the glenoid baseplate above the inferior rim of the glenoid, negative numbers denote placement below the inferior rim of the glenoid
Click here to view |
Clinical evaluation
Patients were assessed clinically for range of motion (ROM) and clinical outcome scores at each follow-up after 6 weeks by an independent evaluator. All planes of rotation were assessed with a hand held goniometer. American Shoulder and Elbow Surgeons (ASES) and visual analog score (VAS) were obtained by an independent evaluator at each time point.
Statistical analysis
Statistical analysis was performed using the SPSS statistical package (IBM Inc. Armonk, NY). Assessment of inter-and intra-observer reliability was performed with kappa and interclass correlation (ICC) and Bland-Altman analysis. The Chi-squared test was used for qualitative data analysis. Differences in quantitative parameters were evaluated with parametric tests (ANOVA) or nonparametric tests (Mann-Whitney U-test) based on the conformation of the distribution. In order to determine factors that contributed to the presence of notching, a multivariate analysis was performed. The significance level was set at P < 0.05.
 Results Results | |  |
There were a total of 54 patients (24 males and 30 females) that had follow-up of a minimum of 2 years and quality radiographic images. The average follow-up was 2.5 years, with a range of 2.0 years to 5.1 years. Of those that did not meet the criteria, two were excluded for poor quality films at 1-year and 2 years follow-up, two were excluded for revision due to fracture of the scapula and need for glenosphere revision after new trauma, and two for death. The average follow-up was 30 months (range: 24-60 months). The most common indication for RTSA was cuff tear arthropathy with degenerative signs present on radiographs such as decreased acromial-humeral interval, acetabularization of the acromion, femoralization of the humeral head or loss of glenohumeral joint space. This was the primary indication in 38 of the 54 patients. There were 9 patients treated with RTSA for fractures, four for failed total shoulder arthroplasty and 2 patients were treated with RTSA after a chronic infection after rotator cuff repair. One patient was treated with RTSA for brachial plexus palsy. The demographics are presented in [Table 2].
The VAS at the time of most recent follow-up was 1.12 ± 1.8 (range: 0-7). The average ASES score was 69.9 ± 19.2 (range: 30-100). One patient had suffered a fall and a subsequent acromial fracture that was managed nonoperatively with no change in clinical function. There was one dislocation in the series; the patient had an original diagnosis of a nonunion. The patient was revised with polyethylene exchange and has done well clinically since their revision. There was one infection that was revised with a two-stage revision procedure. One patient suffered a fall and scapula fracture that required glenosphere revision. Thus, 3 out of 54 RTSA required revision surgeries. There was no evidence of baseplate failures or aseptic loosening.
In order to evaluate the reliability of assessing radiographic changes, the reproducibility and repeatability for all radiographic measures were assessed. The kappa for notching grade was 0.84 (P = 0.02). The ICC for PSNA was low (0.38), but the ICC for PGRD and BPD were much higher (0.79 and 0.92). Using Bland and Altman evaluations, [22] the coefficient of repeatability was 1.27° for PSNA, 0.38 mm for PGRD, and 0.34 mm for BPD.
A majority (39 of 54, 72%) had no evidence of notching at an average follow-up of 2.4 years (range 2.0-4.8 years). Seven patients (13%) had Grade 1 notching at an average follow-up of 2.7 years (range: 2.0-3.9 years), and 7 patients had Grade 2 notching at an average follow-up of 2.7 years (range: 2.0-5.0 years). One patient each (1%) had Grade 3 and 4 notching, both at 3-4 years follow-up. There was no significant difference in time to follow-up when comparing notching scores.
Of the 2 patients with advanced (Grade 3 and 4) notching, both patients were clinically doing well and demonstrated no overt signs of failure of the glenoid component [Figure 3].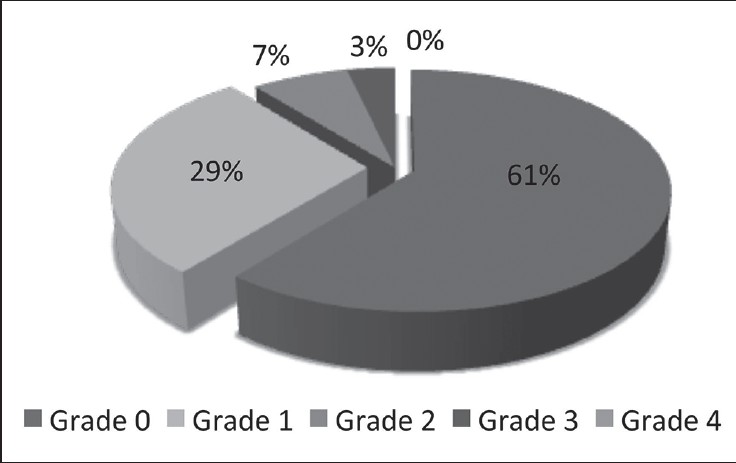 | Figure 3: Evaluation of notching following reverse total shoulder arthroplasty in patients with an average of 30 months follow-up. The majority of patients had Grade 0 or Grade 1 notching
Click here to view |
We evaluated whether notching was a static or progressive process by comparing early (1-year) to late (most recent follow-up) images. If the patient did not have any evidence of notching at 1-year follow-up, no subsequent evidence of notching developed at later follow-up. At 1-year, 12 patients had Grade 1 notching, but 6 would later progress to Grade 2 (5) or Grade 3 (1). One additional patient had progressed from Grade 3 to Grade 4.
Patients were divided into groups with no notching (39 patients) and 15 patients with evidence of notching in order to determine demographic, radiographic and functional factors associated with the presence of notching. A higher PGRD was associated with the presence of a scapular notch (19.7 ± 2.6 mm vs. 22.2 mm ± 3.1 mm, P = 0.005). Similarly, a higher BPD - associated with higher placement of the glenoid baseplate - was also associated with the presence of a scapular notch (0.6 ± 2.0 mm vs. 2.8 ± 3.3 mm, P = 0.03) [Figure 4]. The PSNA was not significantly associated with the presence or absence of a scapular notch (97.7° ± 17° no notching vs. 117.4° ± 17.4°, P = 0.15). There was an increase in the PGRD as well as the BPD from Grade 0 to Grade 2+ notching [Table 3]. However, since the number of patients with Grade 2+ notching was so low (n = 9), the numbers were not statistically significant.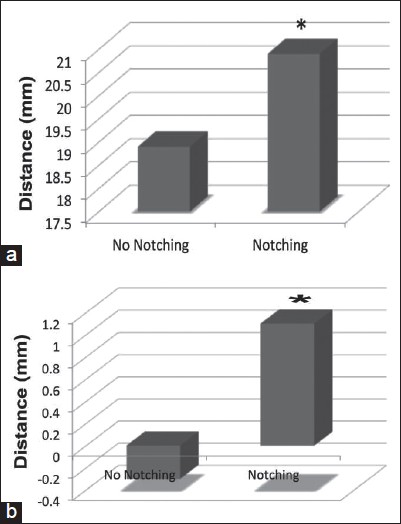 | Figure 4: (a) Evaluation of peg-glenoid rim distance (PGRD) and notching. Patients with notching had a higher PGRD. (b) Evaluation of baseplate distance (BPD) and notching. Patients with notching had a significantly higher BPD compared to those without notching *P < 0.05
Click here to view |
Gender did not make a difference in the development of scapular notching. There was also no difference in patient age, diagnosis, primary or revision procedure, handedness of the patient, surgeon, or body mass index (BMI) of the patient. When evaluating functional outcomes of the patients and their relationship to notching, ROM in all planes did not have a relationship with scapular notching. VAS and ASES scores were not significantly different with the presence or absence of scapular notching [Table 4].
A multivariate analysis was performed in order to determine what factors are associated with scapular notching. When evaluating all independent factors for the presence of notching (age, gender, diagnosis, revision, BMI, radiographic findings, clinical outcome scores, and ROM), only PGRD and BPD are found to be significantly related to scapular notching.
 Discussion Discussion | |  |
The focus of this study was to determine the incidence of scapular notching using a lateralized prosthesis placed inferiorly on the glenoid and to investigate the clinical outcomes of this technique. We found an overall low rate of scapular notching, as 89% of patients demonstrated no notching or mild Grade 1 notching with an average of 30 months follow-up. Only 10% of patients demonstrated Grade 2 or higher notching. We found that base plate position was the most important factor in determining if notching would develop with this prosthesis, with a lower base plate positioned close to the bottom of the glenoid resulting in a lower rate of notching.
The use of a lower neck-shaft angle (125-130°) or higher humeral inclination angle (35-40°) prosthesis has been associated with a lower incidence of scapular notching when compared with other series. Lévigne et al. found that scapular notching overall had a very high incidence (76%) in their series, with a higher percentage of patients with a higher neck-shaft angle prosthesis or lower humeral inclination angle demonstrating significant notching. [15] The lower inclination angle implants (<30°) had a much higher rate of Grade 3 (22%) and Grade 4 (15%) notching compared to the current implant (4% Grade 3 only). Although it is attractive to attribute the lower incidence of notching to the inclination angle of this implant, there are other factors that differ that may have a role. The implant utilized in this study does not sit flush on the Morse taper of the baseplate, thus allowing for 3 mm of increased lateralization of the humerus relative to the glenoid. Kempton et al. similarly found a lower incidence of notching in a prosthesis with a lower neck-shaft angle and a lateralized center of rotation in a recent study. [23] Based on our data and other recent studies, it appears that both humeral inclination angle and lateralized center of rotation may decrease the presence of any notching, and in particular decrease the presence of clinically significant advanced scapular notching.
It stands to reason that placement of the baseplate at the inferior margin of the glenoid would decrease the incidence of notching. In this study, we used two different parameters to measure the position of the baseplate. First, we used the PGRD popularized by Simovitch et al. [24] However, since the prosthesis used in this study has a lateralized glenosphere, we were also able to measure the BPD to the inferior rim of the glenoid. This allowed for two measurements of base plate position. Both of these measurements were reliable and repeatable in this test. With univariate and multivariate analysis, both these measures were predictors of scapular notching. In addition, the PGRD and BPD both increased from Grade 0 to Grade 2+ notching, suggesting that there is a direct correlation with glenoid implant position and the presence of clinically significant notching. Biomechanical studies have confirmed that the placement of the base plate at or below the inferior glenoid rim has an important consequence on decreasing notching. Gutiérrez et al. evaluated multiple factors on the risk of developing scapular notching. They found that both inferior glenoid position and the inferior tilt of the component avoided adduction ROM deficits, which theoretically would decrease the risk of notching. [25] Clinical studies also support the placement of the base plate inferior on the glenoid rim. Kowalsky et al. found a decrease in the amount of notching with lower base plate positioning. [21] In addition, although some biomechanical studies suggest inferior tilt of the glenoid decreases notching, [25],[26] recent clinical studies [27] showed no difference in notching rates or clinical outcomes with or without an inferior tilt of the glenoid components. [19] Placement of the base plate too inferior, however, can be a problem with prosthetic designs with only two base plate screws as one of the screws may not achieve sufficient purchase in the inferior neck if the screws are aimed inferiorly [Figure 5]. Thus, we recommend placement of the baseplate right at the inferior margin of the glenoid rim with screws placed perpendicular to the inferior neck of the glenoid without coming out of the screw as demonstrated in [Figure 5] in order to decrease the risk of notching and maximize the chances of stable fixation.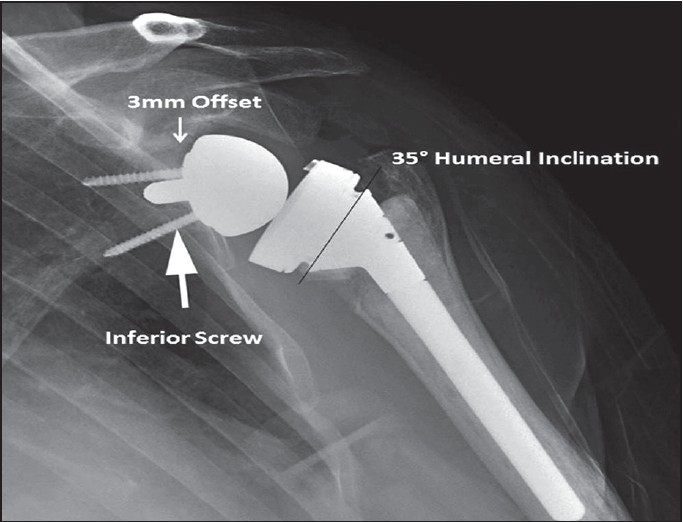 | Figure 5: Clinical example of a baseplate placed on the inferior margin of the glenoid with an inferior trajectory of the screw. The screw penetrates the inferior neck of the scapula, possibly leading to inferior fixation as highlighted by the arrow. The baseplate has 3 mm of offset which is also illustrated, and the humeral inclination angle of 35° is also shown
Click here to view |
Despite the fact that notching has been well described in the RTSA literature, [15],[19],[20],[23],[27],[28],[29],[30],[31] relatively few studies examined whether scapular notching leads to worse clinical outcomes. In a recent study, Sadoghi et al. evaluated 60 RTSA shoulders at a minimum of 2 years after surgery. [30] The study found that there was no significant correlation between infraglenoidal scapular notching and clinical outcomes at 24-60 months, but at the final follow-up of 60 months and more, there was a correlation between infraglenoidal scapular notching and the Constant pain score as well as active ROM. Lévigne et al. [15] did not report a correlation of scapular notching with pain scores and clinical findings, but Sirveaux et al. demonstrated a negative effect of scapular notching on clinical outcome, when evaluated with a constant score. [6] In our study, there was no correlation between notching grade and clinical outcome, but there may not have been enough patients with clinically significant notching. It stands to reason that high grade (Grade 2+) notching may result in an increased risk of poor outcomes, especially at long-term follow-up.
One important finding of our study was that notching did not progress after 1-year in patients with no evidence of notching. All 39 patients with no evidence of notching at 1-year had no evidence of notching at their most recent follow-up. However, patients who did have evidence of notching tended to progress over an average of 18 months by one notching grade. These data suggest that notching is an early phenomenon that likely is progressive in those who develop it, but will present late with clinical symptoms after an RTSA. This is similar to the data presented by Lévigne et al. [15] who demonstrated that notching progressed over a 3-year period. Thus, it appears that those patients with notching should be followed closely to monitor for progression.
Other factors did not appear to influence the development of notching in our study. BMI has been implicated in the development of notching in some studies, [21] but in our study we did not find that this was a significant factor. It is possible that longer-term follow-up will lead to more notching in patients with increased internal rotation, but at 30 months, most patients have gained their entire ROM, and it appears that the notching is stable in the majority of patients.
There are several weaknesses to this study. This is a retrospective review with a 10% of patients lost to follow-up. This can lead to detection bias and alter our findings, but our rate of patients lost to follow-up is consistent with other RTSA studies in the literature. The follow-up is over a short period of time as well. However, most studies suggest that notching is a short-term phenomenon, and does not often progress, especially with low-grade notching. However, we did see that our patients with more advanced notching were progressing. Clearly, this study cohort will be followed for longer-term follow-up to determine the rate of progression and correlation with long-term clinical and radiographic outcomes. Interpretation of radiographs can also be a weakness, but we only had two radiographic series that we were not able to review due to poor image quality. Finally, it was difficult to make conclusions regarding the development of high-grade notching as there were only 6 patients with Grade 2+ notching. This is consistent with other studies evaluating this prosthesis, [21] but makes statistical comparisons difficult.
We found that the current higher inclination angle with a lateral offset center of rotation prosthesis led to a low incidence of scapular notching without any increase in complications. At short-term follow-up, notching was associated with base plate position, but not related to ROM or other clinical outcome measures. Based on these results, we recommend placement of the glenoid base plate at the inferior aspect of the glenoid so as to decrease the risk of notching and improve the likelihood of long-term clinical success.
 References References | |  |
| 1. | Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 2009;18:600-6. 
|
| 2. | Matsen FA 3 rd , Boileau P, Walch G, Gerber C, Bicknell RT. The reverse total shoulder arthroplasty. J Bone Joint Surg Am 2007;89:660-7. 
|
| 3. | Wall B, Nové-Josserand L, O′Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty : a0 review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85. 
|
| 4. | Nolan BM, Ankerson E, Wiater JM. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res 2011;469:2476-82. 
|
| 5. | Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics 2002;25:129-33. 
|
| 6. | Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 2004;86:388-95. 
|
| 7. | Vanhove B, Beugnies A. Grammont′s reverse shoulder prosthesis for rotator cuff arthropathy. A retrospective study of 32 cases. Acta Orthop Belg 2004;70:219-25. 
|
| 8. | Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am 2005;87:1697-705. 
|
| 9. | Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis : r0 esults in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006;15:527-40. 
|
| 10. | Frankle M, Levy JC, Pupello D, Siegal S, Saleem A, Mighell M, et al. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients surgical technique. J Bone Joint Surg Am 2006;88 Suppl 1:178-90. 
|
| 11. | Mulieri P, Dunning P, Klein S, Pupello D, Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am 2010;92:2544-56. 
|
| 12. | Nam D, Kepler CK, Neviaser AS, Jones KJ, Wright TM, Craig EV, et al. Reverse total shoulder arthroplasty : c0 urrent concepts, results, and component wear analysis. J Bone Joint Surg Am 2010;92 Suppl 2:23-35. 
|
| 13. | Naveed MA, Kitson J, Bunker TD. The Delta III reverse shoulder replacement for cuff tear arthropathy: A single-centre study of 50 consecutive procedures. J Bone Joint Surg Br 2011;93:57-61. 
|
| 14. | Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg 2012;21:514-22. 
|
| 15. | Lévigne C, Boileau P, Favard L, Garaud P, Molé D, Sirveaux F, et al. Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2008;17:925-35. 
|
| 16. | Lévigne C, Garret J, Boileau P, Alami G, Favard L, Walch G. Scapular notching in reverse shoulder arthroplasty : i0 s it important to avoid it and how? Clin Orthop Relat Res 2011;469:2512-20. 
|
| 17. | Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005;87:1476-86. 
|
| 18. | Levy J, Blum S. Inferior scapular notching following encore reverse shoulder prosthesis. Orthopedics 2009;32: (10). pii: orthosupersite.com/view.asp?rID=43779. doi: 10.3928/01477447-20090818-23.818-20. 
|
| 19. | Edwards TB, Trappey GJ, Riley C, O′Connor DP, Elkousy HA, Gartsman GM. Inferior tilt of the glenoid component does not decrease scapular notching in reverse shoulder arthroplasty : r0 esults of a prospective randomized study. J Shoulder Elbow Surg 2012;21:641-6. 
|
| 20. | Falaise V, Levigne C, Favard L; SOFEC. Scapular notching in reverse shoulder arthroplasties : t0 he influence of glenometaphyseal angle. Orthop Traumatol Surg Res 2011;97:S131-7. 
|
| 21. | Kowalsky MS, Galatz LM, Shia DS, Steger-May K, Keener JD. The relationship between scapular notching and reverse shoulder arthroplasty prosthesis design. J Shoulder Elbow Surg 2012;21:1430-41. 
|
| 22. | Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307-10. 
|
| 23. | Kempton LB, Balasubramaniam M, Ankerson E, Wiater JM. A radiographic analysis of the effects of prosthesis design on scapular notching following reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2011;20:571-6. 
|
| 24. | Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am 2007;89:588-600. 
|
| 25. | Gutiérrez S, Comiskey CA 4 th , Luo ZP, Pupello DR, Frankle MA. Range of impingement-free abduction and adduction deficit after reverse shoulder arthroplasty. Hierarchy of surgical and implant-design-related factors. J Bone Joint Surg Am 2008;90:2606-15. 
|
| 26. | Gutiérrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE 3 rd . Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg 2007;16:S9-12. 
|
| 27. | Kempton LB, Balasubramaniam M, Ankerson E, Wiater JM. A radiographic analysis of the effects of glenosphere position on scapular notching following reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2011;20:968-74. 
|
| 28. | Boughebri O, Duparc F, Adam JM, Valenti P. Arthroscopic dynamic analysis of scapular notching in reverse shoulder arthroplasty. Orthop Traumatol Surg Res 2011;97:779-84. 
|
| 29. | Chou J, Malak SF, Anderson IA, Astley T, Poon PC. Biomechanical evaluation of different designs of glenospheres in the SMR reverse total shoulder prosthesis : r0 ange of motion and risk of scapular notching. J Shoulder Elbow Surg 2009;18:354-9. 
|
| 30. | Sadoghi P, Leithner A, Vavken P, Hölzer A, Hochreiter J, Weber G, et al. Infraglenoidal scapular notching in reverse total shoulder replacement : a0 prospective series of 60 cases and systematic review of the literature. BMC Musculoskelet Disord 2011;12:101. 
|
| 31. | Valenti P, Sauzières P, Katz D, Kalouche I, Kilinc AS. Do less medialized reverse shoulder prostheses increase motion and reduce notching? Clin Orthop Relat Res 2011;469:2550-7. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
[Table 1], [Table 2], [Table 3], [Table 4]
|
