| |


 |
| Year : 2014 | Volume
: 8
| Issue : 3 | Page : 72-75 |
|
|
|
|
|
ORIGINAL ARTICLE Short stem shoulder replacement
Simon N Bell, Jennifer A Coghlan
Department of Surgery, Melbourne Shoulder and Elbow Centre, Monash University, Melbourne, Australia
Correspondence Address:
Simon N Bell
Melbourne Shoulder and Elbow Centre, Monash University, 31 Normanby St. Brighton, Victoria 3186
Australia
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/0973-6042.140113
Clinical trial registration ACTRN12613001183774

|
|
|
|
| Date of Web Publication | 4-Sep-2014 |
 Abstract Abstract | | |
Context: It is agreed that it is important to anatomically reproduce the proximal humeral anatomy when performing a prosthetic shoulder replacement. This can be difficult with a long stemmed prosthesis, in particular if there is little relationship of the metaphysis to the humeral shaft. The 'short stem' prosthesis can deal with this problem.
Aims: A prospective study assessed the results of total shoulder arthroplasty using a short stem humeral prosthesis, a ceramic humeral head, and a pegged cemented polyethylene glenoid.
Materials and methods: Patients with primary shoulder osteoarthritis were recruited into this prospective trial and pre-operatively had the ASES, Constant, SPADI, and DASH scores recorded. The patients were clinically reviewed at the two weeks, eight weeks, one year, and two year mark with completion of a data form. Radiological evaluation was at the eight week, one year and two year follow-up. At the one and two year follow-up the satisfaction rating, the range of passive and active motion, Constant, ASES, SPADI, DASH and pain results were recorded and analysed with SPPS 20.
Results: During the study period 97 short stem, ceramic head total shoulder replacements were carried out. At the time of follow-up 12 were two years from operation and 38 one year from operation. Active elevation was overall mean 160 degrees. Constant scores were 76 at 1 year, and 86 at 2 years, ASES 88 and 93, and satisfaction 96% and 98% respectively at one and 2 year follow up. There were no problems during insertion of the humeral prosthesis, or any radiolucent lines or movement of the prosthesis on later radiographs.
Conclusion: The short stem prosthesis had no complications, and on follow up radiographs good bone fixation. These fairly short term clinical results were overall good.
Keywords: Ceramic prosthesis, short stem humeral prosthesis, shoulder arthroplasty, shoulder replacement, stemless
How to cite this article:
Bell SN, Coghlan JA. Short stem shoulder replacement. Int J Shoulder Surg 2014;8:72-5 |
 Introduction Introduction | |  |
The prosthetic anatomic shoulder arthroplasty has been shown to produce quite successful results in reducing pain and improving function when performed in patients with glenohumeral arthritis and an intact rotator cuff. For many years, the standard humeral prosthesis followed the example of a hip replacement with a long stem extending down the medulla. [1] This creates problems with trying to recreate the correct anatomy of the proximal humerus, in particular with the orientation of the humeral head component relative to the metaphysis. Numerous innovative designs were devised to try to deal with this problem, with variable geometry of both the proximal portion of the humeral prosthesis and the humeral head. Reproduction with a prosthesis of the correct proximal humeral anatomy when gross deformity is present, in particular malunion following fracture, is often insurmountable with a long stem prosthesis. There was then the introduction of the surface replacement prosthesis, of which the Copeland prosthesis was probably the best known. [2] The technique of reaming of the humeral head for the insertion with a surface replacement tended to overstuff the shoulder joint. As the humeral head was not removed with this surface replacement technique, access for carrying out a glenoid replacement, particularly in a stiff shoulder, was often quite difficult. An alternative to a long stem and a resurfacing replacement is a prosthesis with a short stem which does not extend down the medulla. This has been termed either a stemless or short stem prosthesis. The position of the humeral prosthesis short stem and consequently the humeral head prosthesis is, therefore, not related in any way to the anatomy of the humeral medullary canal. Theoretically, therefore, the humeral head can always be placed exactly in the correct anatomical position for the proximal humeral bone, and in particular for the rotator cuff insertion. This enables a ceramic humeral head to be utilized, as the cone recess of the head is always central.
A short stem humeral shoulder prosthesis system was introduced in 2009 by the Mathys Company (Mathys AG, Bettlach, Switzerland) [Figure 1]. An Australian study was established to prospectively analyze the results with this prosthesis, together with a ceramic head and a cemented double peg biconcave polyethylene glenoid prosthesis.
 Materials and methods Materials and methods | |  |
Ethics approval was given by Monash University and registered with the clinical trials registry ACTRN12613001183774.
A group of five orthopedic surgeons were involved in the prospective study. Patients entered in the study had advanced primary osteoarthritis of the glenohumeral joint and an intact rotator cuff. Exclusion criteria were age over 80 years, inability to replace the glenoid, severe osteoporosis, rotator cuff tear, postfracture/traumatic osteoarthritis or proximal humeral deformity, abnormal neurology, and inability to comply with the study requirements. All data were collected by a dedicated research institute. All patients preoperatively had the American shoulder and elbow surgeons (ASES), Constant, shoulder pain and disability index (SPADI), and disability of the arm, shoulder and hand (DASH) scores, recorded. The SPADI numerical rating scale version) is a self-completed questionnaire which measures current shoulder pain and disability. The lower the score, the better the outcome. The DASH outcome measure is a self-completed questionnaire designed to measure physical function and symptoms in people with any of several musculoskeletal disorders of the upper limb. We scored the disability/symptom 30 point section (scored 1 no difficulty-5 unable to perform the action). The lower the score, the better the outcome.
The patients were clinically reviewed at the 2 weeks, 8 weeks, 1 year, and 2 years mark with completion of a previously devised data form. Radiological evaluation was carried out 1 day following surgery, at 8 weeks postsurgery, and at the 1 year and 2 years follow-up. These radiographs were assessed by an independent orthopaedic surgeon. The humeral head radiographs were classified by a standard technique devised for this prosthesis with the assessment of five zones [Figure 2]. Any radiolucent lines (RLLs) around the glenoid prosthesis cement bone interface were classified according to the Lazarus score. [3] At the 8 weeks review, the level of pain was documented. At the 1 and 2 years follow-up the range of passive and active motion, Constant, ASES, SPADI, DASH, and pain results were recorded. The answers to additional questions relating to satisfaction with operation, improvement in movement for daily activities, and achievement of patient expectations were documented.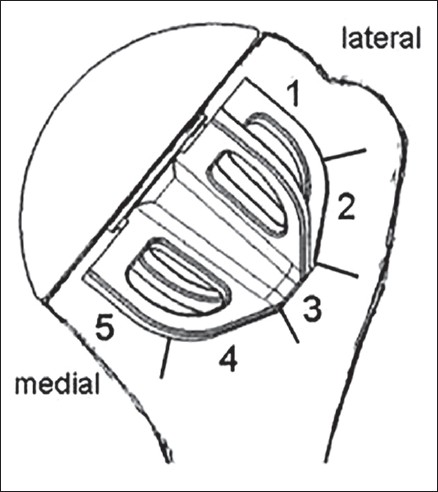 | Figure 2: The five zones assessed for radiolucent lines around the short stem
Click here to view |
Technique of insertion
Operations in all cases were performed through a delto-pectoral approach with tenodesis of the biceps tendon and mobilization of the subscapularis with either a tenotomy or a lesser tuberosity osteotomy. Standard jigs were utilized for the removal of the humeral head. The anatomical margin of the head was defined with a diathermy, and then the cutting jig aligned to remove as close as possible the humeral head at the anatomical neck. The centre of the cut humeral surface was then identified and the appropriate size humeral head to fit this surface determined. The appropriate size short stem cutting jig was then impacted into position and a protective base plate attached to it.
The glenoid was then prepared in a standard manner for the Affinis double pegged glenoid prosthesis, which has been described previously. [4] The appropriate size glenoid prosthesis was then cemented into position with pressure injected cement.
The selected size humeral prosthesis was then impacted partially into position. The appropriate size ceramic head was then attached to this and the head and short stem were then impacted down until the head contacted with the cut surface of the proximal humeral bone. The shoulder was reduced, the subscapularis reattached, and the wound closed.
Postoperative rehabilitation
Patients were immobilized in a sling between 3 and 6 weeks and commenced on a physiotherapy program. Resisted subscapularis strengthening was commenced at 3 months from the operation by the specialist shoulder physiotherapist following a predetermined rehabilitation protocol.
 Results Results | |  |
During the study period 97 short stem, ceramic head total shoulder replacements were carried out. During operative insertion of the short stem humeral prosthesis, there were no intra-operative fractures or problems with instability of the prosthesis.
At the time of follow-up 12 were 2 years from the operation, and 38 were 1 year from the operation. Overall, the mean satisfaction rate for the procedure was 98% (80-100) at 2 years, and 96% (0-100) at 1 year. [Table 1] represents the patient demographics, and [Table 2] active elevation, the ASES, Constant, SPADI and DASH scores, pain, satisfaction with the operation, and radiology scores. At the 1 year follow-up there was one patient who was dissatisfied with the result despite having active elevation of 160° and almost normal power. She felt that her shoulder was inadequate for full use with cross country skiing and, therefore, was dissatisfied with the result.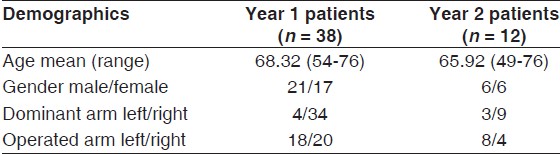 | Table 1: Patient demographics for year 1 follow-up patients and year 2 follow-up patients
Click here to view |
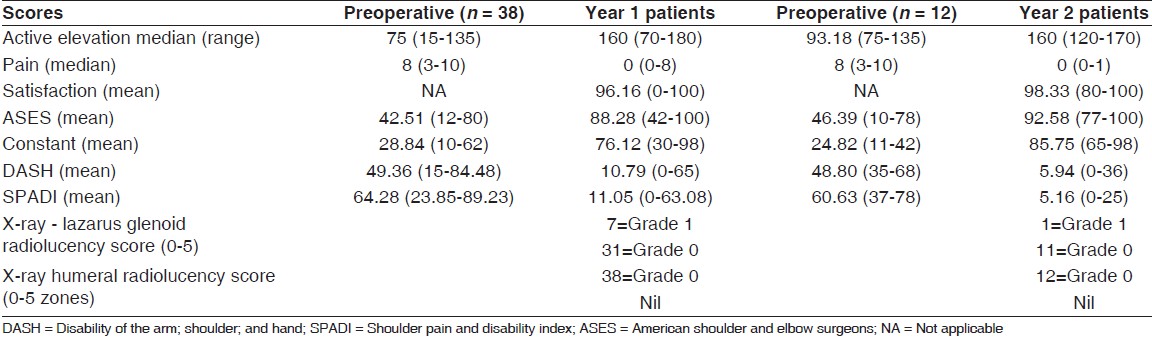 | Table 2: Outcomes for year 1 follow-up patients and year 2 follow-up patients with initial Pre Op scores
Click here to view |
One case required revision. This was the only patient who had previously had a rotator cuff repair. She was 60 years old and clinically had good preoperative supraspinatus power, and at operation an intact tendon. Postoperatively, she had inadequate supraspinatus power and gross fatty atrophy of the supraspinatus muscle on a magnetic resonance imaging. She, therefore, was converted to a reverse prosthesis, which was a relatively easy procedure, and she has a good result at 7 months post revision.
Complications were few, and none related to the prosthesis. There were no infections, fractures, or any instability. Four patients developed acromioclavicular (AC) joint pain months following the replacement. Two of these patients had an AC joint cortisone injection, and finally, the pain resolved in all patients. There were several further problems. There were two transient partial musculocutaneous nerve palsies, one olecranon bursitis, and two skin reactions to the dressings, all of which resolved over time.
Radiological review
The radiographs of the humeral short stem prosthesis demonstrated at the 1 year and 2 years follow-up no sign of any RLL in any area, and there was also no evidence of any migration of any prosthesis [Figure 3]. On the Lazarus scores for the glenoid prosthesis, there were no significant RLLs, and eight patients who had a Lazarus 1 score, which is a partial, RLL around 1 peg.
 Discussion Discussion | |  |
The overall clinical results of this group of patients are good. The constant score of 76 at 1 year and 86 at 2 years compares favorably with the majority of published studies. [5],[6],[7],[8],[9] In a paper reporting the results of the TESS short stem prosthesis, the average constant score was 75. [10] In a paper comparing stemless and stemmed prostheses, the average constant score of the stemless prosthesis was 55, with little difference between the two groups. [11] The ASES score of 93 in our cohort at 2 years is better than most other reports, with Norris reporting an ASES of 86 in 94 total shoulders. [1] The range of motion is also better than most published studies, with average active overhead elevation of 160°. In a paper concerning the Eclipse prosthesis used as a total shoulder arthroplasty and also with the TESS prosthesis, the active elevation was 145° and 142,° respectively. [10],[12] In our cohort, there was a high level of patient satisfaction with the procedure, with at 2 years only three patients with <90% satisfaction with the result. However, these are only short-term results, and longer term follow-up is necessary to, in particular, determine further the incidence of RLLs and polyethylene wear.
There were no problems at all with the use of a short stem prosthesis, in particular there were no problems with insertion, and no intra-operative fractures. At later follow-up there was no evidence of any loosening or migration of the prosthesis, or the development of any RLLs. Only one revision was necessary, which was related to poor supraspinatus muscle function, with no relationship to the prosthesis.
There are a number of advantages of using a short stem humeral prosthesis compared with a long stem, which may account for the good results achieved by the five surgeons in this study. These are two-fold. The use of short stem prosthesis does allow absolute anatomical positioning of the humeral head prosthesis on the proximal humerus, which should give improved functional results. The short-stem prosthesis enables the use of a ceramic humeral head which may provide better wear properties on the glenoid than a metal prosthesis and, therefore, potentially decrease the degree of glenoid loosening in the future. [13] The short stem prosthesis can be used when there is deformity in the proximal humerus, to enable optimal positioning of the anatomical neck humeral cut relative to the rotator cuff insertion without reference to the position of the humeral medulla. Since the head is removed, it does allow adequate access to the glenoid for the proper insertion of a glenoid prosthesis. The short stem diminishes the risk of humeral shaft fracture in subsequent trauma. Should a revision procedure be necessary in the future, in particular conversion to a reverse prosthesis if there is later rotator cuff failure, the humeral side of the revision is much easier than with a well-fixed long humeral stem. There are limitations to the use of this prosthesis in patients with severe osteoporosis, or insufficient bone stock of the proximal humerus for adequate short stem fixation.
Overall, there were no complications at all with the short stem prosthesis in this study. Longer follow-up of these patients will obviously be carried out to assess the effect of the truly anatomical reconstruction, and the ceramic head on the longevity of the prosthesis.
 References References | |  |
| 1. | Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: A multicenter study. J Shoulder Elbow Surg 2002;11:130-5. 
|
| 2. | Levy O, Copeland SA. Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder. J Shoulder Elbow Surg 2004;13:266-71. 
|
| 3. | Lazarus MD, Jensen KL, Southworth C, Matsen FA 3 rd . The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am 2002;84-A:1174-82. 
|
| 4. | Greiner S, Berth A, Kääb M, Irlenbusch U. Glenoid morphology affects the incidence of radiolucent lines around cemented pegged polyethylene glenoid components. Arch Orthop Trauma Surg 2013;133:1331-9. 
|
| 5. | Young A, Walch G, Boileau P, Favard L, Gohlke F, Loew M, et al. A multicentre study of the long-term results of using a flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. J Bone Joint Surg Br 2011;93:210-6. 
|
| 6. | Fucentese SF, Costouros JG, Kühnel SP, Gerber C. Total shoulder arthroplasty with an uncemented soft-metal-backed glenoid component. J Shoulder Elbow Surg 2010;19:624-31. 
|
| 7. | Denard PJ, Raiss P, Sowa B, Walch G. Mid- to long-term follow-up of total shoulder arthroplasty using a keeled glenoid in young adults with primary glenohumeral arthritis. J Shoulder Elbow Surg 2013;22:894-900. 
|
| 8. | Montoya F, Magosch P, Scheiderer B, Lichtenberg S, Melean P, Habermeyer P. Midterm results of a total shoulder prosthesis fixed with a cementless glenoid component. J Shoulder Elbow Surg 2013;22:628-35. 
|
| 9. | Raiss P, Schmitt M, Bruckner T, Kasten P, Pape G, Loew M, et al. Results of cemented total shoulder replacement with a minimum follow-up of ten years. J Bone Joint Surg Am 2012;94:e1711-10. 
|
| 10. | Huguet D, DeClercq G, Rio B, Teissier J, Zipoli B, TESS Group. Results of a new stemless shoulder prosthesis: Radiologic proof of maintained fixation and stability after a minimum of three years′ follow-up. J Shoulder Elbow Surg 2010;19:847-52. 
|
| 11. | Berth A, Pap G. Stemless shoulder prosthesis versus conventional anatomic shoulder prosthesis in patients with osteoarthritis: A comparison of the functional outcome after a minimum of two years follow-up. J Orthop Traumatol 2013;14:31-7. 
|
| 12. | Brunner U, Fruth M, Ruckl K, Magosch M, Tauber M, Resch H, et al. Die schaftfreie Eclipse-prothese-indikation und mittelfristige ergebnisse. Obere Extremitat 2012;7:22-8. 
|
| 13. | Ranawat A, Meftah M, Klingenstein G, Yun RJ, Ranawat C. Long-term survivorship and wear analysis of ceramic and metal on polyethylene in young, active patients: A matched pair analysis. Bone Joint J 2013;95-B Suppl 15:306. 
|
[Figure 1], [Figure 2], [Figure 3]
[Table 1], [Table 2]
|
