| |


 |
| Year : 2014 | Volume
: 8
| Issue : 3 | Page : 81-85 |
|
|
|
|
|
ORIGINAL ARTICLE Comparison of the cheese-wiring effects among three sutures used in rotator cuff repair
Mark Lambrechts1, Behrooz Nazari2, Arash Dini3, Michael J O'Brien3, Wendell M. R. Heard3, Felix H Savoie3, Zongbing You4
1 Department of Orthopaedic Surgery and Tulane Institute of Sports Medicine; Department of Structural and Cellular Biology, Tulane University School of Medicine, New Orleans, LA 70112, USA
2 Department of Orthopaedics, Tabriz Emam Reza Hospital, Tabriz, Iran
3 Department of Orthopaedic Surgery and Tulane Institute of Sports Medicine, Tulane University, School of Medicine, New Orleans, LA 70112, USA
4 Department of Orthopaedic Surgery and Tulane Institute of Sports Medicine; Department of Structural and Cellular Biology; Tulane Cancer Center, Louisiana Cancer Research Consortium, Tulane Center for Aging, Tulane Center for Stem Cell Research and Regenerative Medicine, Tulane University School of Medicine, New Orleans, LA 70112, USA
Correspondence Address:
Zongbing You
1430 Tulane Ave SL 49, New Orleans, LA 70112
USA
 Source of Support: This work was partially supported by a grant provided by DePuy Mitek, Inc., to Tulane University (No. 551206, to Z.Y., F.H.S., and M.J.O.). F.H.S. is an unpaid consultant of DePuy Mitek, Inc., Smith & Nephew plc, and Rotation Medical and Biomet Sports Medicine, as well as a board member of the rthroscopy Association of North America Education Foundation and of the Trustees for Arthroscopy., Conflict of Interest: None
DOI: 10.4103/0973-6042.140115
 |
|
|
|
| Date of Web Publication | 4-Sep-2014 |
 Abstract Abstract | | |
Purpose: The goal of this study was to compare the cheese-wiring effects of three sutures with different coefficients of friction.
Materials and methods: Sixteen human cadaveric shoulders were dissected to expose the distal supraspinatus and infraspinatus muscle tendons. Three sutures were stitched through the tendons: #2 Orthocord™ suture (reference #223114, DePuy Mitek, Inc., Raynham, MA), #2 ETHIBOND* EXCEL Suture, and #2 FiberWire® suture (FiberWire® , Arthrex, Naples, FL). The sutures were pulled by cyclic axial forces from 10 to 70 N at 1 Hz for 1000 cycles through a MTS machine. The cut-through distance on the tendon was measured with a digital caliper.
Results: The cut-through distance in the supraspinatus tendons (mean ± standard deviation, n = 12) were 2.9 ± 0.6 mm for #2 Orthocord™ suture, 3.2 ± 1.2 mm for #2 ETHIBOND* suture, and 4.2 ± 1.7 mm for #2 FiberWire® suture. The differences were statistically significant analyzing with analysis of variance (P = 0.047) and two-tailed Student's t-test, which showed significance between Orthocord™ and FiberWire® sutures (P = 0.026), but not significant between Orthocord™ and ETHIBOND* sutures (P = 0.607) or between ETHIBOND* and FiberWire® sutures (P = 0.103).
Conclusion: The cheese-wiring effect is less in the Orthocord™ suture than in the FiberWire® suture in human cadaveric supraspinatus tendons.
Clinical Relevance: Identification of sutures that cause high levels of tendon cheese-wiring after rotator cuff repair can lead to better suture selection.
Keywords: Biomechanics, cadaver study, cheese-wiring, supraspinatus tendon, suture
How to cite this article:
Lambrechts M, Nazari B, Dini A, O'Brien MJ, Heard WM, Savoie FH, You Z. Comparison of the cheese-wiring effects among three sutures used in rotator cuff repair. Int J Shoulder Surg 2014;8:81-5 |
 Introduction Introduction | |  |
Rotator cuff tear is one of the most common injuries involving the shoulder. The tear most often involves the supraspinatus tendon. Without prompt treatment, the altered joint biomechanics can extend the tear to involve the infraspinatus tendon. [1],[2] Repair of these injuries is based on individual patients with few protocols established to determine whether the patient best fits for steroid injection, physical therapy, or surgical intervention. However, surgery is generally recommended for all symptomatic patients younger than 60 with a full-thickness rotator cuff tear. [3] The expected outcome of surgery is a high fixation strength, but many variables can affect the success of surgery including the patient's age, tendon health, smoking, time from tear to surgery, arthroscopic technique, suture location, and suture selection. [4],[5],[6],[7]
The choice of sutures has not been well studied. It has been reported that the suture location is a key factor in causing damage to the repaired tendons. Wieser et al. [8] found the ideal placement to be located in the center of the tendon just medial to the rotator cable. This finding is in contrast to Wang et al. [9] who found an ideal location of suture placement more medially at the muscle-tendon junction. Clearly, location of the placed sutures is important in minimizing postsurgical tendon damage, but the properties of the sutures should also be a consideration. Unfortunately, it is not easy to evaluate different sutures because different types of repair define surgical success differently. For example, rotator cuff repair requires suture stability under high load requirements, while flexor tendon repair requires minimal friction. Nevertheless, there are several well-recognized suture properties including the tensile strength, knot security, stiffness, and resistance to fraying. [10],[11],[12],[13],[14],[15]
Coefficient of friction is an inherent property of the suture, which has not been well investigated. Silva et al. [16] found that #3-0 FiberWire® sutures (FiberWire® , Arthrex, Naples, FL) had a lower coefficient of friction (0.054) than #3-0 ETHIBOND* sutures (with a coefficient of friction of 0.076) (ETHIBOND* EXCEL, Ethicon, Somerville, NJ). We speculate that coefficient of friction may be an important factor in determining how easy the suture cuts through the tendon, that is, the cheese-wiring effect. Our hypothesis is that the sutures with lower coefficient of friction may be easier to cut-through the tendon than the sutures with higher coefficient of friction. The present study was conducted to test this hypothesis.
 Materials and methods Materials and methods | |  |
This study was conducted using human cadaveric supraspinatus and infraspinatus muscle tendons. Eight pairs of unembalmed human shoulders (n = 16) were obtained from donors through the Bureau of Anatomical Services, Louisiana State Department of Health and Hospitals. The average age of the donors was 77.1 ± 9.8 years of age. The use of these deidentified specimens was determined as "not human subjects study" by Tulane University Institutional Review Board (Project no. 206610-1). The specimens were stored at −20°C and thawed at room temperature prior to use. Only grossly intact tendons without obvious damage were used for the study. Twelve supraspinatus tendons (n = 12) were dissected out and detached distally from the greater tubercle of the humerus. The supraspinatus muscles remained attached to the scapula and the subscapularis and infraspinatus muscles remained undisturbed during testing of the supraspinatus tendons. After testing on the supraspinatus tendons, the infraspinatus tendons were dissected out and detached distally, while the infraspinatus muscle remained attached to the scapula. Only 5 infraspinatus tendons (n = 5) were not damaged and were used for testing. The three types of sutures used in this study were #2 FiberWire® suture (reference #AR-7200, Arthrex, Inc., Naples, FL), #2 ETHIBOND* EXCEL suture (reference #X519, Ethicon, Inc., Somerville, NJ), and #2 Orthocord™ suture (reference #223114, DePuy Mitek, Inc., Raynham, MA). FiberWire® suture is constructed of a multi-strand, long chain ultra-high molecular weight polyethylene (UHMWPE) core with a braided jacket of polyester and UHMWPE. ETHIBOND* suture is composed of a braided polyester core coated with polybutilate. Orthocord™ suture is made with a braided polyethylene core coated with a copolymer of caprolactone and glycolide.
Biomechanical testing
We used a Bionix Servohydraulic Test System (MTS Systems Corporation, Eden Prairie, MN) for the mechanic tests. The scapula with the proximal attachment of supraspinatus (or infraspinatus) muscle was fixed to the sensor stage using a custom-made frame [Figure 1]a. A single pass-through suture loop was placed through the supraspinatus (or infraspinatus) tendon approximately 5 mm distal to the muscle-tendon junction [Figure 1]b. The other end of the suture loop was attached to the actuator [Figure 1]a. The specimen was kept moist at all times by spraying of phosphate buffered saline.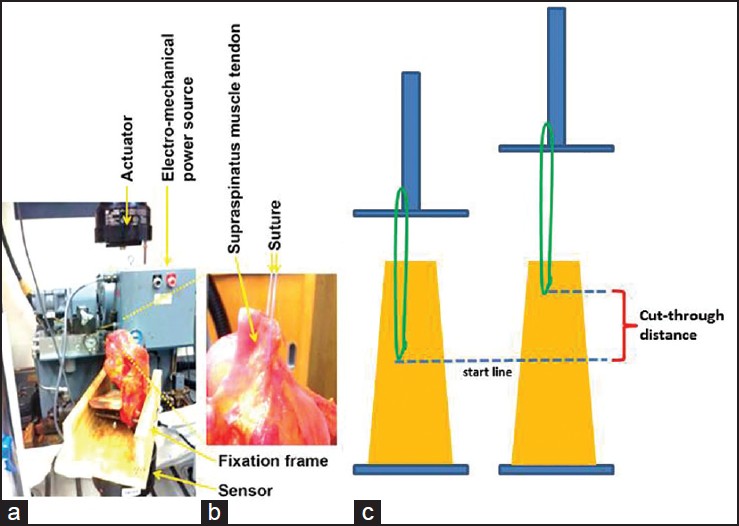 | Figure 1: Illustration of how the mechanic testing was performed. (a) The specimen was fi xed to the sensor of an MTS machine by a fi xation frame; the suture was stitched through the supraspinatus muscle-tendon and connected to the actuator; and a computer (not shown) controlled the electro-mechanical power source to drive the actuator to provide uniaxial tensile force loading on the suture, and recorded the load and displacement through the testing time period.
(b) A representative close-up picture is showing the tendon and suture. (c) An illustration of how the cut-through in the tendon was recorded
Click here to view |
In our pilot study, two shoulders were used to determine the testing conditions. A force of 10 N was applied to preload the tendon and the suture for 1 min. No cutting through of the tendon was observed by any of the three sutures at 10 N loading. A mark line (start line) was made on the tendon with a marker pen. Then, a 10-50 N at 1 Hz for 1000 cycles of cyclic pulling load was applied to the suture. At the end of 1000 cycles, any cut-through of the tendon by the suture was recorded manually with a digital caliper [Figure 1]c. Then, the load was returned to 10 N for 1 min. Next, this step was repeated at 10-70 N at 1 Hz for 1000 cycles. Again, the cut-through distance was recorded. Finally, this step was repeated at 10-100 N at 1 Hz for 1000 cycles. However, at this load, all three sutures completely cut-through the tendon when the load was approximately 80-85 N. Therefore, we decided to test each suture by applying 10-70 N at 1 Hz for 1000 cycles.
Twelve supraspinatus muscle tendons were tested first, followed by testing five infraspinatus muscle tendons. The three sutures were tested on each tendon side-by-side, with approximately 5 mm inter-stitch distance. Each of the three sutures was stitched in an alternated order, so that the location of stitch and order of testing were equally assigned to each suture. For example, on tendon #1, Orthocord™ suture was tested first, followed by ETHIBOND* suture and then FiberWire® suture. On tendon #2, the order of testing was ETHIBOND*, FiberWire® , and Orthocord™ . On tendon #3, the order of testing was FiberWire® , Orthocord™ , and ETHIBOND*. On tendons #4-12, the alternating order was repeated. The three investigators (M.L., B.N., and A.D.) who performed the tests were blinded to the sources of the sutures during testing.
Measurement of the cut-through distance
After 1000 cycles of 10-70 N loading at 1 Hz were completed, the force was returned to 10 N. The cut-through distance [Figure 1]c was measured manually with a digital caliper. This cut-through distance is called displacement, which represents the cheese-wiring effect of the suture. The MTS machine also continuously recorded the axial displacement during the 1000 cycles, which was the change of distance between the sensor and actuator, including the cut-through distance and stretching of the muscle, tendon, and suture.
Statistical analysis
The displacement and axial displacement were shown as means and standard deviations. The data was analyzed with analysis of variance (ANOVA) software provided by GraphPad Prism (GraphPad Software, Inc., La Jolla, CA) and using two-tailed Student's t-test. The significance was set at P < 0.05.
 Results Results | |  |
We found that the axial displacement, as recorded by the MTS machine, was proportional to the cyclic load applied to each suture [Figure 2]a-f. In the tests of 12 supraspinatus tendons, the displacements (i.e., the cut-through distances on the tendons), as manually recorded with a digital caliper at the end of 1000 cycles of loading, were 2.9 ± 0.6 mm for #2 Orthocord™ suture, 3.2 ± 1.2 mm for #2 ETHIBOND* suture, and 4.2 ± 1.7 mm for #2 FiberWire® suture. Statistical significance existed using ANOVA (P = 0.047) and comparing Orthocord™ to FiberWire® sutures (P = 0.026), however, the difference was not statistically significant between ETHIBOND* and FiberWire® sutures (P = 0.103) or between Orthocord™ and ETHIBOND* sutures (P = 0.607) [Figure 3]a. The axial displacements, as recorded by the MTS machine from cycle 1 to 1000, were not statistically different among the three sutures [P > 0.05, [Figure 3]b]. However, the axial displacement from cycle 100 to 1000, while not significant with ANOVA, was clearly longer in FiberWire® suture than in Orthocord™ or ETHIBOND* sutures [Figure 3]c. The difference was statistically significant between Orthocord™ and FiberWire® sutures (P = 0.022) and between ETHIBOND* and FiberWire® sutures (P = 0.011), but there was no statistical significance between Orthocord™ and ETHIBOND* sutures (P = 0.510) [Figure 3]d. | Figure 2: Representative recordings of uniaxial cyclic loading force over time (a-c) and axial displacement over time (d-f)
Click here to view |
 | Figure 3: The displacements of sutures in the supraspinatus tendons recorded manually and automatically by the MTS machine. (a) The displacement (cut-through distance) of sutures measured manually with a digital caliper at the end of 1000 cycles of 10-70 N loading. (b) The overall axial displacements of sutures recorded by the MTS machine at the end of 1000 cycles of 10-70 N loading, which included the cut-through distance and the stretching of the muscle, tendon, and suture. (c) The axial displacements of sutures recorded by the MTS machine from 100 to 1000 cycles of 10-70 N loading. (d) The axial displacements of sutures at the end of 1000 cycles, recorded by the MTS machine from 100 to 1000 cycles of 10-70 N loading. The data represent means ± standard deviations (error bars, n = 12)
Click here to view |
In the tests of 5 infraspinatus tendons, the displacements (i.e., the cut-through distances on the tendons), as manually recorded with a digital caliper at the end of 1000 cycles of loading, were 6.7 ± 2.0 mm for #2 Orthocord™ suture and 6.1 ± 0.6 mm for #2 ETHIBOND* suture, which was not statistically significant [P = 0.612, [Figure 4]a]. In contrast, #2 FiberWire® suture completely cut-through the infraspinatus tendon, which was >15 mm from start line to the distal end of the tendon. The axial displacements, as recorded by the MTS machine from cycle 1 to 1000, were not statistically different between Orthocord™ and ETHIBOND* sutures [P > 0.05, [Figure 4]b-c. | Figure 4: The displacements of sutures in the infraspinatus tendons recorded manually and automatically by the MTS machine. (a) The displacement (cut-through distance) of sutures measured manually with a digital caliper at the end of 1000 cycles of 10-70 N loading. (b) The overall axial displacements of sutures recorded by the MTS machine at the end of 1000 cycles of 10-70 N loading, which included the cut-through distance and the stretching of the muscle, tendon, and suture. (c) The axial displacements of sutures at the end of 1000 cycles, recorded by the MTS machine from 100 to 1000 cycles of 10-70 N loading. Of note, FiberWire® suture completely cut-through the infraspinatus tendons for a distance >15 mm. The data represent means ± standard deviations (error bars, n = 5)
Click here to view |
 Discussion Discussion | |  |
This study found that #2 FiberWire® suture cuts through the supraspinatus tendon easier than #2 Orthocord™ suture under 1000 cycles of 10-70 N loading conditions. This finding was further supported by the tests with infraspinatus tendons, as #2 FiberWire® suture completely cut-through the tendon (>15 mm) whereas #2 Orthocord™ suture only cut-through <7 mm. Similarly, #2 ETHIBOND* suture only cut-through the infraspinatus tendons for approximately 6 mm. These findings suggest the #2 FiberWire® is more likely to cut-through the tendons than #2 Orthocord™ or ETHIBOND* suture. Although the difference is about 1 mm after 1000 cycles of loading at up to 70 N, the difference may be bigger at higher loads and/or more cycles.
It is worth pointing out that the overall axial displacements caused by the three sutures were of no difference [Figure 3]b, which is contradictory to our manual measurement [Figure 3]a. We consider that this axial displacement, as recorded by the MTS machine, was the change of distance between the actuator and the sensor, including the cut-through by the suture and the stretched length of the muscle, tendon and suture. Thus, this axial displacement does not accurately reflect the cut-through by the suture at the beginning of the cyclic loading when the loading mainly stretched the muscle and tendon. This explanation is supported by our finding that the axial displacements from cycles 100 to 1000 [Figure 3]c-d were consistent to our manual measurement [Figure 3]a, because at this late stage the axial displacement mainly reflects the cut-through after the muscle and tendon had already been stretched by the initial pulling loads.
We speculate that the observed differences in the cut-through (or cheese-wiring effect) are due to the different coefficients of friction of sutures. It has been reported that #3-0 FiberWire® suture had a lower coefficient of friction than #3-0 ETHIBOND* suture. [16] This difference in friction may be caused by differences in material properties and the way how the strands are braided. FiberWire® suture is constructed of a multi-strand, long chain UHMWPE core with a braided jacket of polyester and UHMWPE. ETHIBOND* suture is composed of a braided polyester core coated with polybutilate. Orthocord™ suture is made with a braided polyethylene core coated with a copolymer of caprolactone and glycolide. Other physical properties of the sutures may also play a role. For example, it has been found that ETHIBOND* suture is considerably less stiff (13 ± 2 N/m) than FiberWire® suture (35 ± 6 N/m). [12] This indicates that the stiffer FiberWire® suture may be more likely to cut-through the tendons.
This study has some limitations since it was a laboratory study using human cadaveric tendons. First, no healing occurred in the cadaveric specimens. In live patients, healing may occur between the physical loads, so as to mitigate the cheese-wiring effect. Second, only a single pass-through stitch was tested. This could be meaningful in clinical situations where this type of suture method is used to restore the continuity of broken tendons. However, this finding may not be applicable to other suture methods such as mattress or figure of eight sutures. Finally, only 10-70 N cyclic loading was tested. This was due to a limitation caused by the cadaveric tendon quality where a load of 80-85 N led to complete cut-through of the tendons. It is possible that higher loads may be applied to fresh (or live) tendons.
 Conclusion Conclusion | |  |
We found that #2 Orthocord™ and ETHIBOND* sutures cause less cheese-wiring effects than #2 FiberWire® suture in human cadaveric supraspinatus and infraspinatus tendons under 1000 cycles of 10-70 N cyclic pulling loads.
 Acknowledgments Acknowledgments | |  |
The authors thank Eric Morales and Dr. Erich Richter (Department of Neurosurgery, Louisiana State University-New Orleans) and Rita Richardson and Donna Watkins (Department of Orthopaedic Surgery, Tulane University) for their laboratory assistance. Z. You was partially supported by two grants from the National Institute of General Medical Sciences (P20GM103518) and the National Cancer Institute (R01CA174714) of the National Institutes of Health, three grants from Department of Defense Health Program through the Prostate Cancer Research Program (W81XWH-14-1-0050, W81XWH-14-1-0149, and PC130118; the U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office), the Developmental Fund of Tulane Cancer Center (TCC), and Louisiana Cancer Research Consortium (LCRC) Fund. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Defense.
 References References | |  |
| 1. | Jerosch J, Müller T, Castro WH. The incidence of rotator cuff rupture. An anatomic study. Acta Orthop Belg 1991;57:124-9. 
|
| 2. | Lee TQ. Current biomechanical concepts for rotator cuff repair. Clin Orthop Surg 2013;5:89-97. 
|
| 3. | Williams GR Jr, Rockwood CA Jr, Bigliani LU, Iannotti JP, Stanwood W. Rotator cuff tears: Why do we repair them? J Bone Joint Surg Am 2004;86-A:2764-76. 
|
| 4. | Chung SW, Kim JY, Kim MH, Kim SH, Oh JH. Arthroscopic repair of massive rotator cuff tears: Outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med 2013;41:1674-83. 
|
| 5. | Favard L, Bacle G, Berhouet J. Rotator cuff repair. Joint Bone Spine 2007;74:551-7. 
|
| 6. | Kukkonen J, Kauko T, Virolainen P, Äärimaa V. Smoking and operative treatment of rotator cuff tear. Scand J Med Sci Sports 2014;24:400-3. 
|
| 7. | Mukovozov I, Byun S, Farrokhyar F, Wong I. Time to surgery in acute rotator cufftear: A systematic review. Bone Joint Res 2013;2:122-8. 
|
| 8. | Wieser K, Rahm S, Farshad M, Ek ET, Gerber C, Meyer DC. Stitch positioning influences the suture hold in supraspinatus tendon repair. Knee Surg Sports Traumatol Arthrosc 2013;21:1587-92. 
|
| 9. | Wang VM, Wang FC, McNickle AG, Friel NA, Yanke AB, Chubinskaya S, et al. Medial versus lateral supraspinatus tendon properties: Implications for double-row rotator cuff repair. Am J Sports Med 2010;38:2456-63. 
|
| 10. | Ilahi OA, Younas SA, Ho DM, Noble PC. Security of knots tied with ethibond, fiberwire, orthocord, or ultrabraid. Am J Sports Med 2008;36:2407-14. 
|
| 11. | Mahar AT, Moezzi DM, Serra-Hsu F, Pedowitz RA. Comparison and performance characteristics of 3 different knots when tied with 2 suture materials used for shoulder arthroscopy. Arthroscopy 2006;22:614.e1-2. 
|
| 12. | Najibi S, Banglmeier R, Matta J, Tannast M. Material properties of common suture materials in orthopaedic surgery. Iowa Orthop J 2010;30:84-8. 
|
| 13. | Swan KG Jr, Baldini T, McCarty EC. Arthroscopic suture material and knot type: An updated biomechanical analysis. Am J Sports Med 2009;37:1578-85. 
|
| 14. | Wright PB, Budoff JE, Yeh ML, Kelm ZS, Luo ZP. Strength of damaged suture: An in vitro study. Arthroscopy 2006;22:1270-1275.e3. 
|
| 15. | Wüst DM, Meyer DC, Favre P, Gerber C. Mechanical and handling properties of braided polyblend polyethylene sutures in comparison to braided polyester and monofilament polydioxanone sutures. Arthroscopy 2006;22:1146-53. 
|
| 16. | Silva JM, Zhao C, An KN, Zobitz ME, Amadio PC. Gliding resistance and strength of composite sutures in human flexor digitorum profundus tendon repair: An in vitro biomechanical study. J Hand Surg Am 2009;34:87-92. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|
