| |


 |
| Year : 2014 | Volume
: 8
| Issue : 3 | Page : 86-89 |
|
|
|
|
|
SURGICAL TECHNIQUE Noncomminuted lateral end clavicle fractures associated with coracoclavicular ligament disruption: Technical considerations for optimal anatomic fixation and stability
Richard S Page1, Deepak N Bhatia2
1 St. John of God Hospital, Geelong, Victoria 3220, Australia
2 Department of Orthopaedic Surgery, Seth GS Medical College, King Edward VII Memorial Hospital, Parel, Mumbai, Maharashtra, India
Correspondence Address:
Deepak N Bhatia
Department of Orthopaedic Surgery, Seth GS Medical College, King Edward VII Memorial Hospital, Parel, Mumbai - 400 012, Maharashtra
India
 Source of Support: None, Conflict of Interest: None  | 2 |
DOI: 10.4103/0973-6042.140116

|
|
|
|
| Date of Web Publication | 4-Sep-2014 |
 Abstract Abstract | | |
Distal clavicle fractures associated with coracoclavicular ligament disruption are potentially unstable and necessitate surgical treatment. Current fixation techniques are nonanatomic and do not address relevant aspects of the pathoanatomy. We have developed a technique that uses a unique combination of implants; this permits minimally invasive fixation and stable reduction with a lateral fragment size as small as 5 mm. The surgical technique consists of (1) neutralization of muscular forces on the proximal fragment using a minimally invasive ligament repair device (TightRope™, Arthrex, FL, USA) and (2) internal fixation using a contour-matched locking plate (2.4 mm LCP® Distal radius plates, Synthes, USA). Technical tips to optimize this new procedure are discussed. The technique can be extended to an "arthroscopic-assisted" method involving arthroscopic coracoclavicular fixation followed by a mini-open plate fixation of the clavicular fragments.
Keywords: Clavicle fracture, coracoclavicular ligaments, coracoid process, locking plate, shoulder
How to cite this article:
Page RS, Bhatia DN. Noncomminuted lateral end clavicle fractures associated with coracoclavicular ligament disruption: Technical considerations for optimal anatomic fixation and stability. Int J Shoulder Surg 2014;8:86-9 |
How to cite this URL:
Page RS, Bhatia DN. Noncomminuted lateral end clavicle fractures associated with coracoclavicular ligament disruption: Technical considerations for optimal anatomic fixation and stability. Int J Shoulder Surg [serial online] 2014 [cited 2016 May 30];8:86-9. Available from: http://www.internationalshoulderjournal.org/text.asp?2014/8/3/86/140116 |
 Introduction Introduction | |  |
Fractures of the lateral clavicle with associated coracoclavicular ligament disruption (Neer type 2) are potentially unstable and are associated with a high rate of nonunion when treated conservatively. [1] Internal fixation of these fractures is often difficult due to two anatomical factors:
- Inadequate distal fragment size and
- displacement and instability consequent to ligament disruption.
Several techniques, both open and arthroscopic, have been described to overcome these anatomical difficulties, however, none of these techniques effectively address the pathoanatomy. [2],[3],[4],[5],[6],[7],[8],[9],[10],[11],[12],[13] We present a technique that permits minimally invasive apposition of bone fragments and neutralization of displacement forces; a combination of implants described here enables the surgeon to achieve stable reduction with a lateral fragment size as small as 5 mm [14],[15] [Figure 1].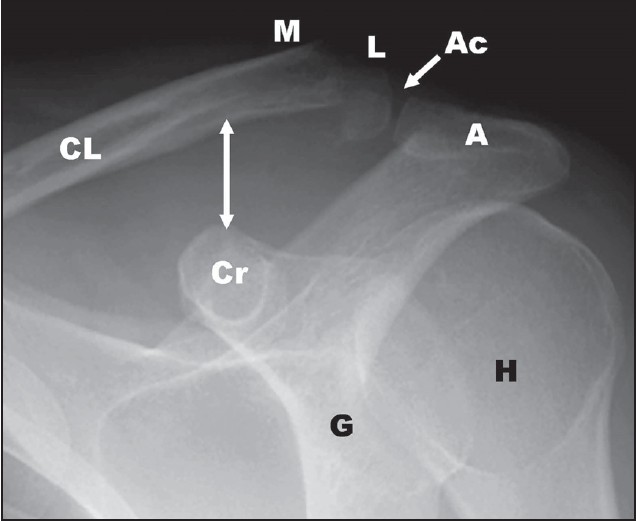 | Figure 1: A 15° cephalad tilt radiograph of the glenohumeral joint shows a noncomminuted lateral clavicle fracture. Increased coracoclavicular distance (arrows) suggests disruption of the coracoclavicular ligaments. (Ac: acromioclavicular joint, A: acromion, CL: clavicle, M: medial fragment, L: lateral clavicle fragment, Cr: coracoid, G: glenoid, H: humeral head)
Click here to view |
 Indications and contraindications Indications and contraindications | |  |
Neer type 2 fractures of the lateral end of the clavicle can be further subclassified into four fracture patterns as described by Bhatia and Page. [14] The technique described here is indicated for type 1 and type 2 fracture patterns. Types 3 and 4 involve extension of fracture lines into the distal fragment, and the technique is contraindicated in these types.
 Surgical technique Surgical technique | |  |
Under general anesthesia, the patient is placed in the beach-chair position with the back tilted 40° to 60° to the horizontal. The entire upper extremity and the shoulder are prepared and draped up to the medial border of the scapula and the lower pectoral region. A 5 cm linear incision is made over the fracture site; this extends from 1 cm lateral to the acromioclavicular joint and extends linearly along the lateral clavicle to approximately 1 cm medial to the clavicular region overlying the palpable coracoid process tip. The skin and subcutaneous tissues are undermined, and the underlying deltoid is visualized. In acute cases, the medial and lateral clavicular fragments are found to be "stripped" of soft-tissue attachments; the stripped deltoid-trapezius fascia is meticulously dissected and stay sutures are passed for subsequent repair. The probe is inserted through the interval between the separated deltoid fascial origin; this is used to assess the integrity of the coracoclavicular ligaments, and also to ascertain the angle of approach to the coracoid process for coracoclavicular fixation [Figure 2]. Next, the medial and lateral clavicular fragments are exposed; in the presence of segmental comminution of the lateral clavicle, periosteal stripping is avoided to prevent devascularization of the comminuted fragments. The acromioclavicular joint is located by inserting a 22-guage hypodermic needle into it and the acomioclavicular ligaments spanning the joint are exposed. It is not necessary to expose the acromioclavicular facets, and care is taken to preserve the spanning ligaments. The distance between this needle and the medial end of the lateral clavicular fragment is measured. In the absence of sufficient bone stock in the lateral fragment (minimum 5 mm), alternate procedures may be necessary.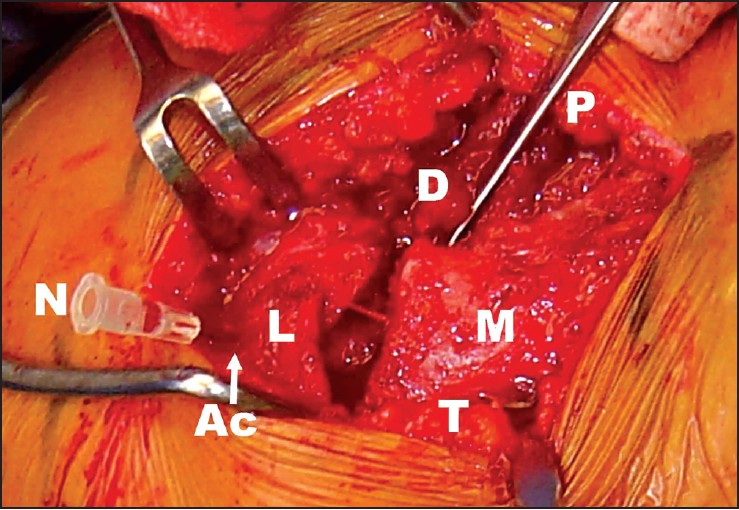 | Figure 2: Intraoperative demonstration of the pathoanatomy of lateral clavicle fractures. A needle (N) marks the position of the acromioclavicular joint (Ac). The torn deltoid (D) and trapezius (T) attachments and the lateral (L) and medial (M) clavicular fragments are seen. A probe (P) is used to palpate the coracoid process
Click here to view |
Coracoclavicular ligament reconstruction and augmentation are performed using a minimally invasive ligament repair device (TightRope™, Arthrex, FL, USA). Several techniques exist for passage of this device, and the steps are only briefly mentioned here. [6],[7],[8],[10],[12] First, the "junctional surface area" of the coracoid is located using a probe; this area has been described by Bhatia et al. as the geometric attachment site of the coracoclavicular ligaments. [16] Once this is located, the mid-point of the superior clavicle surface overlying this region is marked, and a 4 mm hole is drilled through the clavicle. Next, a drill-guide is passed anterior to the clavicle; this is positioned on the superior coracoid pillar and a 4 mm hole is drilled through this region. Alternately, an aiming jig may be used as described by some authors. [7] A nitinol wire is passed, first through the clavicular hole, and then through the coracoid hole, and is retrieved from the lateral aspect of the coracoid using a curved artery forceps. This wire is used to shuttle the ligament repair device, which is then tightened to achieve fracture reduction, and secured to hold the medial clavicular fragment in place.
The adequacy and stability of fracture reduction are assessed, after initial fixation with the ligament repair device, as described below: The arm is gradually left unsupported, and the fracture site is observed for displacement or distraction. In our experience, in most case, a distraction of the fracture site is observed and is an indication for additional fixation [Figure 3]. This is achieved using a five-hole distal radial locking plate (2.4 mm LCP® Distal radius plates, Synthes, USA). The plate is contoured intra-operatively to convert the volar angulation into a neutral position, and the locking holes at either end of the horizontal limb of the "T" are bent inward by about 20°. Reduction is optimized by supporting the arm, thereby reducing the distraction and achieving contact between the fragments. The horizontal limb is aligned with the lateral clavicle fragment, and the vertical limb of the plate is secured to the medial clavicle fragment with screws. Finally, the lateral fragment is secured by placing locking screws through the horizontal distal limb of the plate. Adequacy of reduction is assessed once again by gradually reducing arm support; stable fixation prevents any distraction at the fracture site [Figure 4] and [Figure 5]. The deltoid-trapezius fascia is meticulously reattached with sutures to cover the low-profile plate; failure to do so can cause the prominence of the plate and necessitate early implant removal.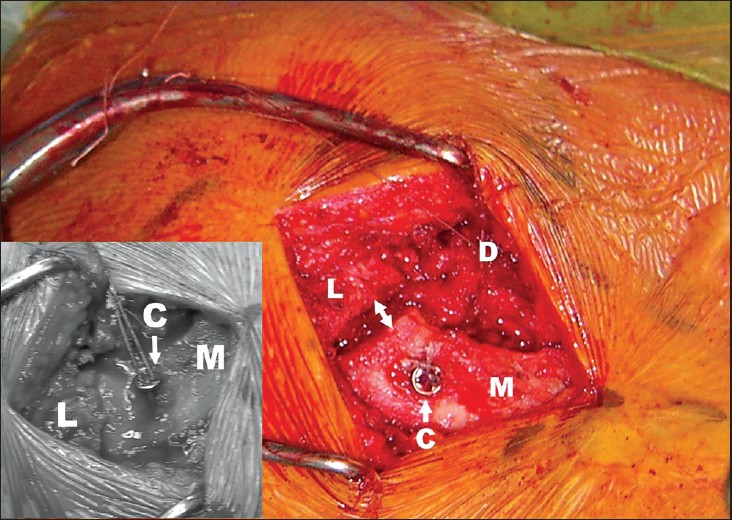 | Figure 3: The coracoclavicular ligament repair device (C) reduces the medial fragment (M) to the level of the lateral fragment (L). Distraction of the fracture site (arrows) is seen when the arm is left unsupported. Inset: With the arm supported, the lateral and medial fragments are in apposition
Click here to view |
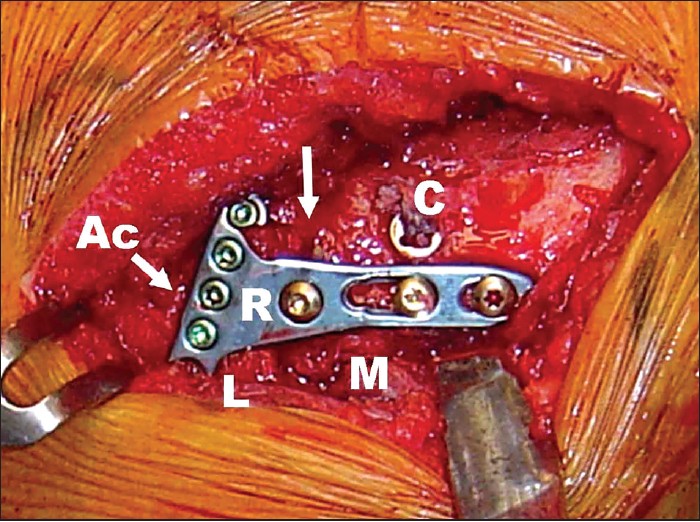 | Figure 4: A five-hole locking radius plate (R) and the coracoclavicular fixation device (C) achieve adequate fixation of the fracture fragments (M and L) and apposition across the fracture site (Top arrow). (Ac: acromioclavicular joint)
Click here to view |
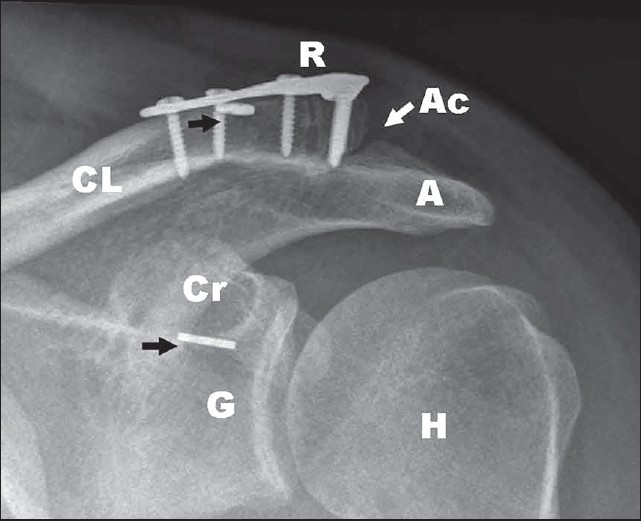 | Figure 5: Follow-up radiograph shows signs of union across the fracture site (R: radius locking plate, Ac: acromioclavicular joint, A: acromion, CL: clavicle, Cr: coracoid, G: glenoid, H: humeral head, black arrows: coracoclavicular fixation device buttons)
Click here to view |
The technique can be extended to an "arthroscopic-assisted" method, developed by one of the authors (DNB); this involves arthroscopic coracoclavicular cerclage or endobutton fixation, followed by a mini-open plate fixation of the clavicular fragments.
In the postoperative period, the upper limb is supported in a sling for 2-3 weeks, to permit soft-tissue healing. During this period, passive range of motion exercises is performed. After the first 3 weeks, the sling is discarded, active-assisted, and active range of motion exercises is begun. Muscle strengthening exercises are added after 6 weeks.
 Discussion Discussion | |  |
Open surgical techniques for internal fixation of Neer type 2 lateral end clavicle fractures usually involve acromioclavicular joint spanning implants, either transacromial kirschner wires or hook plates. [2],[3] Others have described the use of coracoclavicular screws and tension band wires for a fragment reduction. [4],[5] On the other hand, arthroscopic techniques focus solely upon coracoclavicular ligament reconstruction to neutralize displacement forces between fracture fragments; these arthroscopic techniques may not result in adequate apposition in all fracture patterns, and there may exist residual instability between fracture fragments [Figure 3]. [6],[7],[8]
The use of distal radius locking plates for lateral clavicle fracture fixation has been recently described with excellent early results by Kalamaras et al.; additional sutures looped around the coracoid and clavicle were used in 6 of the 9 patients reported. [10] Our technique utilizes a combination of a locking T-plate with a minimally invasive coracoclavicular ligament augmentation device; we have used this technique and its variations for lateral end clavicle fractures associated with coracoclavicular ligament insufficiency. The Tightrope™ device (TightRope™, Arthrex, FL, USA). Is commercially available and can be implanted in a minimally invasive method. In addition, it is sufficiently strong to oppose the displacement forces, thereby decreasing the load on the locking plate. This permits secure fixation of fragments as small as 5 mm without excess stress on the distal screws.
The technique presented here adequately addresses the pathoanatomy of unstable lateral clavicle fractures. First, the displacement secondary to coracoclavicular ligament disruption is neutralized using a ligament augmentation/repair device. Second, the displaced fracture fragments are stabilized using a low-profile contoured locking plate without having to span the acromioclavicular joint. Third, repair of the deltoid-trapezius fascia adds to the stability by further neutralizing displacement forces. Fourth, bone grafting can be performed in nonunions of lateral clavicle fractures.
The technique has limitations; small size and comminution of the distal fragment can prevent adequate purchase of distal locking screws and are contraindications to plate fixation. A minimum of 5 mm of circumferential cortical integrity is necessary for screw purchase in the distal fragment. Radiographic types 1 and 2 fracture patterns described by Bhatia and Page are ideal indications. [14]
 Conclusion Conclusion | |  |
A combination of coracoclavicular ligament augmentation device and low profile distal radius locking T-plate permits minimally invasive fixation of unstable lateral clavicle fractures. The technique can be extended to an "arthroscopic-assisted" method involving arthroscopic coracoclavicular fixation followed by a mini-open plate fixation of the clavicular fragments.
 References References | |  |
| 1. | Neer CS II nd . Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma 1963;3:99-110. 
|
| 2. | Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res 2006;447:158-64. 
|
| 3. | Kao FC, Chao EK, Chen CH, Yu SW, Chen CY, Yen CY. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma 2001;51:522-5. 
|
| 4. | Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br 1991;73:291-4. 
|
| 5. | Levy O. Simple, minimally invasive surgical technique for treatment of type 2 fractures of the distal clavicle. J Shoulder Elbow Surg 2003;12:24-8. 
|
| 6. | Nourissat G, Kakuda C, Dumontier C, Sautet A, Doursounian L. Arthroscopic stabilization of Neer type 2 fracture of the distal part of the clavicle. Arthroscopy 2007;23:674.e1-4. 
|
| 7. | Pujol N, Philippeau JM, Richou J, Lespagnol F, Graveleau N, Hardy P. Arthroscopic treatment of distal clavicle fractures: A technical note. Knee Surg Sports Traumatol Arthrosc 2008;16:884-6. 
|
| 8. | Checchia SL, Doneux PS, Miyazaki AN, Fregoneze M, Silva LA. Treatment of distal clavicle fractures using an arthroscopic technique. J Shoulder Elbow Surg 2008;17:395-8. 
|
| 9. | Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: Early observations using a new technique. J Shoulder Elbow Surg 2008;17:60-2. 
|
| 10. | Richards A, Tennent D. Arthroscopic stabilisation of acute distal clavicle fractures and dislocations using the TightRope syndesmosis repair system. Presented at the 10 th International Congress of Shoulder and Elbow Surgery, La Bahia, Brazil; 2007. 
|
| 11. | Shyamalan G, Tennent D. The TightRope system. Arthroscopy 2008;24:494. 
|
| 12. | Wellmann M, Zantop T, Petersen W. Minimally invasive coracoclavicular ligament augmentation with a flip button/polydioxanone repair for treatment of total acromioclavicular joint dislocation. Arthroscopy 2007;23:1132.e1-5. 
|
| 13. | Jackson WF, Bayne G, Gregg-Smith SJ. Fractures of the lateral third of the clavicle: An anatomic approach to treatment. J Trauma 2006;61:222-5. 
|
| 14. | Bhatia DN, Page RS. Surgical treatment of lateral clavicle fractures associated with complete coracoclavicular ligament disruption: Clinico-radiological outcomes of acromioclavicular joint sparing and spanning implants. Int J Shoulder Surg 2012;4:116-20. 
|
| 15. | Page RS, Bhatia DN. Non-comminuted lateral clavicle fractures associated with coracoclavicular ligament disruption: A new anatomical technique for superior fixation and stability. J Bone Joint Surg Br 2010;92B Suppl I:214. 
|
| 16. | Bhatia DN, de Beer JF, du Toit DF. Coracoid process anatomy: Implications in radiographic imaging and surgery. Clin Anat 2007;20:774-84. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|
