| |


 |
| Year : 2014 | Volume
: 8
| Issue : 4 | Page : 122-126 |
|
|
|
|
|
REVIEW ARTICLE Association between screw prominence and vascular complications after clavicle fixation
Harry D. S. Clitherow1, Gregory I Bain2
1 Department of Orthopaedics, Monash Medical Centre, Moorabbin; Melbourne Shoulder & Elbow Centre, Brighton; Department of Orthopaedic Surgery, Monash University, Melbourne, Victoria, Australia
2 Department of Orthopaedics and Trauma, Flinders Medical Centre; Department of Orthopaedic Surgery, Flinders University, Adelaide, SA, Australia
Correspondence Address:
Harry D. S. Clitherow
196 Melbourne Street, North Adelaide, 5006, South Australia
Australia
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.145261

|
|
|
|
| Date of Web Publication | 21-Nov-2014 |
 Abstract Abstract | | |
Context: Fixation of clavicle fractures has become more common to prevent symptomatic malunion and nonunion. The subclavian and axillary vessels are in close proximity to the medial two-thirds of the clavicle, placing them at risk from prominent metalware. Injury to these major vessels has the potential to be life or limb-threatening. Despite this anatomical risk, iatrogenic vascular injury associated with clavicle fixation is rare.
Aims: The aim of this study was to identify risk factors associated with modern fixation techniques in reported cases of vascular injury after clavicle fixation.
Materials and Methods : A literature search was performed, and all identified cases of iatrogenic vascular injury associated with prominent clavicle fixation were analyzed. Clinical details, the total length of the prominent screws and the distance that they protruded from the far cortex were recorded.
Results: Five cases were identified; there were four pseudoaneurysms and one arteriovenous fistula. The total length of the offending screw was identifiable in two cases, measuring 26 and 30 mm. The length of screw prominence was identifiable in 3 cases (8, 10 and 10 mm). The pseudoaneurysms presented at 2-10 years following clavicle fixation. Three of these cases developed limb-threatening ischemia.
Conclusions: Vascular complications associated with clavicle fixation are uncommon but potentially limb-threatening. Several associated factors are identified. The authors provide a number of detailed recommendations aimed at preventing these complications.
Keywords: Arteriovenous fistula, axillary artery, clavicle fracture, complication, internal fixation, risk factor, subclavian artery
How to cite this article:
Clitherow HD, Bain GI. Association between screw prominence and vascular complications after clavicle fixation. Int J Shoulder Surg 2014;8:122-6 |
 Introduction Introduction | |  |
Clavicle fixation
Fixation of clavicle fractures has become more common since the recognition of symptomatic malunion and nonunion as an important complication of non-operative management. [1],[2],[3] These are typically young, active patients who are involved in sports or have manual occupations. [4],[5] Fixation is generally performed with plate and screw or intramedullary constructs. The use of Kirschner wire constructs around the shoulder is associated with wire migration to the major vessels and spinal cord. [6]
Anatomy
The subclavian vessels ascend from the thoracic cavity. In the thoracic outlet, they are separated by scalenus anterior, with the artery running posterior to the muscle and the vein anterior. Lateral to scalenus anterior, the vessels pass over the first rib, at which point they are named the axillary vessels. These vessels are at risk of injury as they run past the clavicle toward the axilla.
Previous anatomical studies have demonstrated the relationship of the vessels to the medial two-thirds of the clavicle in detail. All measurements have been rounded down to the nearest millimeter.
Clavicle thickness
The maximum superior to inferior diameter (thickness) of dry bone clavicles has been reported to be 17 mm, and 15 mm at the site where the axillary artery crosses under the clavicle. [7] The mean maximal thickness of the clavicle, in any direction, has been reported to be 24 mm (range: 13-34) in the medial third and 15 mm (range: 11-28) in the middle third. [8]
Distance from clavicle to vessels
The distance from the superior surface of the clavicle to the superior surface of the subclavian artery in cadavers has been reported as 22-34 mm. [7] A magnetic resonance imaging (MRI) study reported the distance from the anterior surface of the clavicle to the sheath of the neurovascular bundle as 11-22 mm in the medial third and 16-64 mm in the middle third. [9]
The reported mean distance from the subclavian and axillary vessels to the nearest surface of the clavicle ranges from 17 to 26 mm for the arteries and 5 to 12 mm for the veins. However, the artery can be as close as 5 mm, and the vein may be directly apposed to the clavicle [8] [Table 1].
Orientation of vessels to the clavicle
Computed tomography and MRI studies have reported that the vessels are directly posterior to the medial third of the clavicle and are posteroinferior to the middle third. [8],[9] The recommended safe trajectory for screws in the medial third of the clavicle is from superior to inferior, and in the middle third, it is from anterior to posterior. [8]
Screw protrusion and vascular injury
Screws that protrude from the posterior and posteroinferior aspects of the clavicle are at risk of injuring these vascular structures. Despite this, vascular injuries have, fortunately, been rare, and several large series of clavicle fixation cases have reported no vascular complications. [10] The length that a screw can safely protrude from the far cortex of the clavicle has not been reported.
Aim
The aim of this study was to identify risk factors associated with modern fixation techniques in reported cases of vascular injury after clavicle fixation.
 Materials and methods Materials and methods | |  |
Articles reporting vascular injury associated with clavicular fixation were reviewed. A search of the PubMed and EMBASE databases was performed of English language journals using the search terms "clavicle," "internal fixation" "arterial" "venous," "vascular" and "complication."
The inclusion criteria were: Vascular injury associated with prominent internal fixation of the clavicle. Exclusion criteria were: Vascular injury presenting prior to internal fixation, thoracic outlet syndrome with no evidence of vessel wall injury, deep vein thrombosis with no evidence of external injury to the vessel wall, and fixation using Kirschner wire constructs.
Abstracts were screened, and all potentially suitable articles were reviewed in full. Reference lists from these articles were also reviewed to identify further suitable articles.
The clinical details of each case were recorded, and particular attention paid to identify the length of the offending screw and the distance it protruded from the far cortex. If the actual screw length was reported, this was recorded. Attempts were made to contact the authors of all the case reports to verify the length of the screws and their protrusion.
Radiological and clinical images of the protruding screws were measured for screw length and protrusion from the cortex using Pixelstick 2.5 software (PlumAmazing, Princeville, Hawaii, USA). This tool expresses measurements as numbers of pixels, which can be extrapolated to millimeters by comparing them to objects of a known length in the same image (the diameter 3.5 mm diameter of a screw and if known, the total length of the screw). All measurements were rounded down to the nearest millimeter.
 Results Results | |  |
Complications
Ten papers met the inclusion criteria. No randomized trials or case series regarding this subject were found. Of these 10 papers, five were excluded: Two involved migration of Kirschner wires and two involved a compressive thoracic outlet syndrome with no injury to the vessel wall. The fifth paper involved a deep vein thrombosis of the subclavian and axillary veins but no external injury the great veins.
The five studies that were included were all case reports. There were four cases of arterial pseudoaneurysm [11],[12],[13],[14] and one case of subclavian arteriovenous (AV) fistula. [15] All were associated with prominent screws. There were no reported fatalities from arterial injury due to clavicle fixation.
The indication for fixation, location of the initial fracture, delay between fixation and presentation, and the length and position of the offending screw are presented in [Table 2].
In all cases, the indication for the index surgery was related to a fracture in the middle third of the clavicle. The delay between the fracture and surgery varied with the indication for fixation, ranging from acute fracture [12],[15] to nonunion of up to 2 years duration. [11],[13],[14]
All cases had been treated with a clavicular plate. There was no supplemental fixation such as an independent interfragmentary screw or cerclage wires. All cases implicated the tip of a prominent screw as the cause of vascular injury and all but one of the offending screws was medial to the fracture site. No cases implicated a displaced bone spike. No cases reported significant intraoperative bleeding during the initial fixation.
All of the pseudoaneurysms presented as intermittent claudication symptoms in the ipsilateral upper limb. There was a prolonged delay of 2-10 years between clavicle fixation and presentation. In three of the four cases, there was a subsequent acute deterioration into limb-threatening ischemia, due to emboli in the upper limb. [11],[12],[14]
The AV fistula presented 4 months after clavicle fixation as a pulsatile supraclavicular mass with associated ipsilateral arm weakness.
All five cases required a vascular procedure (stent or graft).
Screw lengths
Two authors [11],[14] replied to our requests for further information.
The total length of the protruding screw was identifiable in two cases as 26 and 30 mm. The screw protrusion length could be identified in three of the five cases as 8, 10, and 10 mm [Table 2].
In one case, [11] the screw protrusion could be measured from a radiograph [Figure 1] and in another [14] it could be measured from a clinical photograph [Figure 2]. In both cases, the offending screw was markedly longer than the screws either side of it.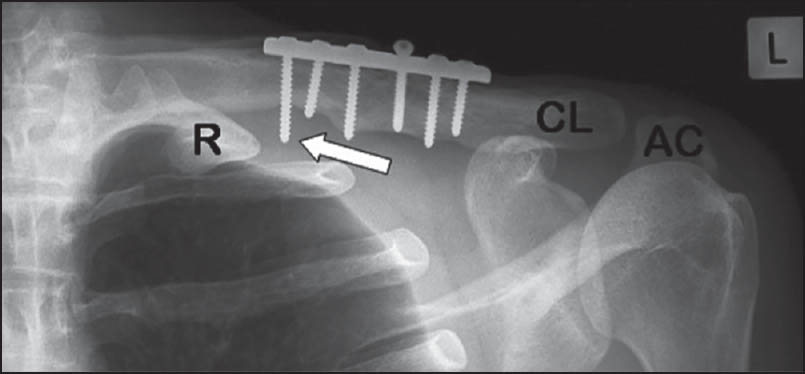 | Figure 1: Plain radiograph of 3.5 mm dynamic compression plate with prominent medial screw (white arrow). Note the offending screw is markedly longer than the adjacent screws. R = First rib; CL = Clavicle; AC = Acromion. (Bain GI, Galley IJ, Keogh AR, Durrant AW. Axillary artery pseudoaneurysm after plate osteosynthesis for a clavicle nonunion: A case report and literature review. Int J Shoulder Surg 2010;4:79-82. Reproduced with permission)
Click here to view |
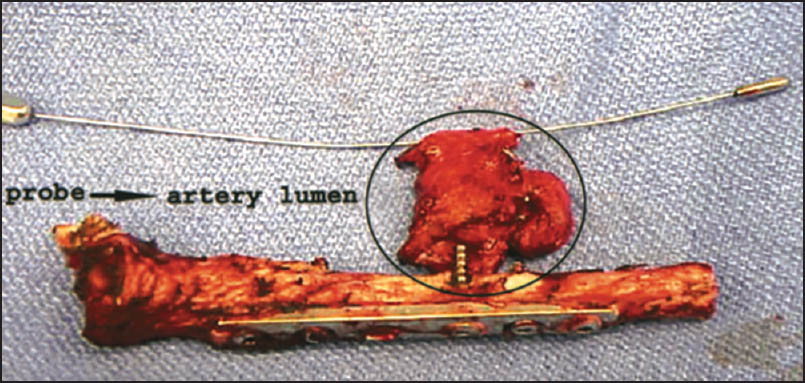 | Figure 2: Excised clavicle with 3.5 mm plate and screws and associated pseudoaneurysm around the tip of the prominent screw. A dilator has been placed through the true lumen of the excised segment of the subclavian artery. This image depicts several identifi ed risk factors. The offending screw is markedly longer than the adjacent screws and protrudes from the posteroinferior surface of the middle clavicle third. The screw passage is eccentric, such that the surgeon may only have encountered one cortex when drilling the hole. (Shackford SR, Connolly JF. Taming of the screw: a case report and literature review of limb-threatening complications after plate osteosynthesis of a clavicular nonunion. J Trauma 2003;55:840-3. Reproduced with permission)
Click here to view |
In two of the cases, the only image available was of angiogram with an oblique view of the clavicle. A reliable measurement could not be determined.
 Discussion Discussion | |  |
While iatrogenic vascular injury following clavicle fixation is rare; it is a clinically significant, potentially limb-threatening and ultimately preventable complication. A number of factors could potentially be associated with this complication.
The initial injury was a diaphyseal clavicle fracture in all cases. This is not surprising, given that approximately 80% of all clavicle fractures occur in this region. [1] The indications for the index procedure varied widely from acute fracture to nonunion of 2 years duration.
There were no reported fatalities resulting from arterial injury associated with prominent metalware. In addition, the authors could find no reports of fatalities arising from arterial injury that was identified intraoperatively.
There were no medial or lateral fractures among the reported cases, but the results are still of relevance in the management of these injuries: The most medial holes of a lateral fracture plate will encroach upon the middle third of the clavicle, and all screws will be at risk during fixation of medial fractures.
All cases were associated with prominent screws, and the offending screw was medial to the fracture in all but one case, where it was immediately lateral to the fracture. This is consistent with the described anatomy, where the vascular structures are most at risk in the medial two-thirds of the clavicle.
The sharpness of the protruding screw tip could be expected to affect the likelihood of developing a vascular injury. Unfortunately, it was not possible to identify the type of screw tips used in the studies that were reviewed.
The total length of the offending screws ranged from 26 to 30 mm, which is within the range of reported clavicle diameters. Maximum clavicle diameter is not a reliable indicator that a chosen screw length will be safe. If the screw is aimed off center, it is possible that it will protrude markedly from the far cortex as demonstrated by the prominent screw in [Figure 2].
The minimum screw prominence resulting in a vascular injury was 8 mm. It is alarming that this length is less than the reported mean distances between the clavicle and the arteries (17-26 mm). [8],[9] It has been proposed that the injury occurs when the vessels are brought closer to the metalware during arm movement. [12] The authors feel that this highlights the need for a low margin of tolerance for screw prominence in this procedure. To prevent injury to the artery, it must be less than the reported minimum distance from the vessel to the bone (5 mm).
The use of an all unicortical locking screw construct avoids screw prominence, but this removes the ability to apply compression across the fracture using the plate. In some fracture configurations, this may be overcome by using an independent interfragmentary compression screw. However, the direction of this screw required to achieve maximal compression may not be along a safe trajectory. This screw will be at risk of prominence and must be placed with caution.
Only one case in our study recorded the region of the protrusion, [12] in that instance the screw was medial to the fracture site and protruded from the posterior cortex.
Limitations
There are important limitations to this study. The sample size is very small due to the rarity of these complications, and the published articles are all case reports. Readers may believe that arterial injury may be anecdotally more common than the findings of this report. However, the authors can only interpret the literature that is published.
There is a potential error in the calculation of screw length due to differences in the orientation of the published images.
Recommendations
Based on the findings of this study and a review of the literature, the authors make the following recommendations:
1. Dissection
Subperiosteal dissection should be performed around the medial two-thirds of the clavicle to avoid inadvertent injury to an adherent major vessel. The authors note that other authors have recommended extra-periosteal dissection due to concerns regarding impairment of blood supply. [16] However, the authors of the current study believe that the potential morbidity arising from major vessel injury greatly outweighs that of impaired blood supply to the medial two-thirds of the clavicle.
2. Screw direction
As recommended by Sinha et al., [8] drills and screws should be aimed superior to inferior in the medial third and anterior to posterior in the middle third of the clavicle.
3. Screw length
Caution must be employed if the measured screw length is >16 mm. This is derived from the narrowest reported clavicle thickness (11 mm) and the closest reported distance of the vessels to the middle third of the clavicle (5 mm). If the screw is longer than this, or is markedly longer than the adjacent screws, the surgeon must pay close attention to the trajectory of the screw and the degree of prominence to ensure they are within the safe range.
4. Screw prominence
The maximum allowable is 4 mm, based on the closest reported distance of the vessels to the middle third of the clavicle (5 mm).
If there is any doubt about the degree of screw prominence, an intraoperative assessment must be performed. Subperiosteal dissection can be used to identify the screw tips. Intraoperative fluoroscopy could also be used in this situation but may be unreliable if the imaging plane is not perpendicular to the screws.
5. Follow-up
Patients who present with a peri-clavicular mass or ischemic episodes in the ipsilateral upper limb require an urgent vascular imaging and assessment by a vascular surgeon.
Patients who present with prominent medial screws should be considered for an angiogram and plate removal, irrespective of whether they have current vascular symptoms or not. This recommendation holds even if there has been a delay of several years since the initial fixation was performed.
 Acknowledgment Acknowledgment | |  |
The authors wish to thank Dr. Steven Shackford for providing further information regarding his previously published case.
 References References | |  |
| 1. | Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am 2007;89:1-10.  |
| 2. | Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537-9.  |
| 3. | McKee MD, Pedersen EM, Jones C, Stephen DJ, Kreder HJ, Schemitsch EH, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am 2006;88:35-40.  |
| 4. | Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res 1994:127-32.  |
| 5. | Robinson CM, Goudie EB, Murray IR, Jenkins PJ, Ahktar MA, Read EO, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: A multicenter, randomized, controlled trial. J Bone Joint Surg Am 2013;95:1576-84.  |
| 6. | Lyons FA, Rockwood CA Jr. Migration of pins used in operations on the shoulder. J Bone Joint Surg Am 1990;72:1262-7.  |
| 7. | Galley IJ, Watts AC, Bain GI. The anatomic relationship of the axillary artery and vein to the clavicle: A cadaveric study. J Shoulder Elbow Surg 2009;18:e21-5.  |
| 8. | Sinha A, Edwin J, Sreeharsha B, Bhalaik V, Brownson P. A radiological study to define safe zones for drilling during plating of clavicle fractures. J Bone Joint Surg Br 2011;93:1247-52.  |
| 9. | Qin D, Zhang Q, Zhang YZ, Pan JS, Chen W. Safe drilling angles and depths for plate-screw fixation of the clavicle: Avoidance of inadvertent iatrogenic subclavian neurovascular bundle injury. J Trauma 2010;69:162-8.  |
| 10. | Wijdicks FJ, Van der Meijden OA, Millett PJ, Verleisdonk EJ, Houwert RM. Systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg 2012;132:617-25.  |
| 11. | Bain GI, Galley IJ, Keogh AR, Durrant AW. Axillary artery pseudoaneurysm after plate osteosynthesis for a clavicle nonunion: A case report and literature review. Int J Shoulder Surg 2010;4:79-82.  [ PUBMED]  |
| 12. | Johnson B, Thursby P. Subclavian artery injury caused by a screw in a clavicular compression plate. Cardiovasc Surg 1996;4:414-5.  |
| 13. | Casselman F, Vanslembroek K, Verougstraete L. An unusual cause of thoracic outlet syndrome. J Trauma 1997;43:142-3.  |
| 14. | Shackford SR, Connolly JF. Taming of the screw: A case report and literature review of limb-threatening complications after plate osteosynthesis of a clavicular nonunion. J Trauma 2003;55:840-3.  |
| 15. | Ding M, Hu J, Ni J, Lv H, Song D, Shu C. Iatrogenic subclavian arteriovenous fistula: Rare complication of plate osteosynthesis of clavicle fracture. Orthopedics 2012;35:e287-9.  |
| 16. | Altamimi SA, McKee MD, Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am 2008;90 Suppl 2:1-8.  |
[Figure 1], [Figure 2]
[Table 1], [Table 2]
|
