| |


 |
| Year : 2015 | Volume
: 9
| Issue : 1 | Page : 20-23 |
|
|
|
|
|
SURGICAL TECHNIQUE Pectoralis major transosseous equivalent repair with knotless anchors: Technical note and literature review
Gonzalo S Samitier, Alejandro I Marcano, Kevin W Farmer
Department of Orthopaedics and Rehabilitation, University of Florida, Gainesville, FL, USA
Correspondence Address:
Kevin W Farmer
Orthopaedics and Sports Medicine Institute, 3450 Hull Road, University of Florida, Gainesville, FL 32607
USA
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.150219
 |
|
|
|
| Date of Web Publication | 28-Jan-2015 |
 Abstract Abstract | | |
Introduction: Rupture of the pectoralis major (PM) tendon was initially described almost 2 centuries ago, but most of the reported injuries have occurred within the last 30 years. Options for repair have varied widely. The most common methods for repair depend on either transosseous sutures or suture anchors for fixation. Transosseous suture repair allows for docking the tendon into a trough at its anatomic insertion, but risks cortical breakage during suture passing. Our experience has confirmed the value and potential advantages of anchors for a secure fixation.
Aims: To describe a variation of repair using knotless suture anchors and a burred trough to dock the tendon into its anatomic insertion.
Conclusion: We describe a technique of a transosseous equivalent PM repair technique. To our knowledge, this is the first paper describing such a repair technique for PM rupture.
Keywords: knotless suture anchors, pectoralis major repair, pectoralis major rupture, suture anchors, transosseous repair
How to cite this article:
Samitier GS, Marcano AI, Farmer KW. Pectoralis major transosseous equivalent repair with knotless anchors: Technical note and literature review. Int J Shoulder Surg 2015;9:20-3 |
 Introduction Introduction | |  |
Pectoralis major (PM) ruptures were initially described by Patissier in 1822. The majority of the reported injuries have been within the last 30 years, likely due to the increasing volume of athletes in sporting activities. [1] The PM participates in adduction, internal rotation, and flexion of the humerus. The anatomy is well-defined, with the origins from the sternum, the medial clavicle, the aponeurosis of the external oblique muscle and the first six ribs. The PM tendon has a peculiar humeral insertion, turning 90° on itself, and inserting laterally to the biceps tendon. The portion that originated from the clavicular and upper sternum attach distally (clavicular head), while the lower sternal and abdominal fibers cross above and insert superiorly on the humerus (sternal head), covering a combined area of 5 cm. [2],[3] The fibers of the sternal head are maximally elongated during activities involving abduction, external rotation, and extension of the humerus, such as during bench press, thus putting the inferior tendon insertion at the highest risk of injury early on. [4] Although many cases are partial ruptures, complete tears also commonly occur, predominantly in the area of the distal musculotendinous junction or tendon insertion. [5]
Pectoralis major ruptures typically occur when the shoulder is in full extension and externally rotated, while trying to resist a sudden forceful load directed in an anterior to posterior direction. Injury can occur during either the concentric or eccentric aspects of the activity. Furthermore, it appears that a correlation exists between the mechanism of injury and rupture site. Tears of the muscle belly are more common due to direct trauma, whereas indirect trauma or overload often leads to avulsion of the humeral insertion or injury at the musculotendinous junction. This rupture is commonly associated with bench pressing, rugby, and American style football. Anabolic steroids have also been linked to an injury. [5] PM ruptures remain a predominantly male injury, even though women are increasingly getting involved in activities such as power lifting and bodybuilding.
The classic clinical presentation for this injury is a sudden, severe pain in the shoulder or axilla, with or without an audible "snap," ecchymosis, swelling, and weakness. Physical examination shows an asymmetry of the axillary fold, often with an area of depression at the deltopectoral groove. Asymmetric bulging at the origin of the pectoralis on the chest occurs with contraction of the pectoralis. Muscle strength examination demonstrates weakness in arm adduction and internal rotation.
Radiographs usually do not show abnormalities except in bony avulsion cases; absence of the pectoral shadow has been described as a consistent finding for clinical diagnosis. [6] Ultrasound has been used as a powerful tool to visualize tears; however, magnetic resonance imaging (MRI) is considered as the gold standard imaging modality. [7]
The most commonly used classification for this rupture was suggested by Tietjen [8] and modified by Berson: [9]
- Contusion or sprain
- Partial tear
- Complete tear
- Muscle origin
- Muscle belly
- Musculotendinous junction
- Muscle tendon itself
- Bony flake avulsion of the tendon
- Intratendinous ruptures.
Treatment depends on the location of the tear and the level of physical activity of the patient, as well as comorbidities. Intramuscular tears are often treated nonoperatively, typically with rehabilitation. For physically demanding patients, surgical repair provides optimal outcomes in regard to strength, cosmetics, and earlier return to competitive sports without limitations. Early repair is superior to delayed repair. [5]
Options for repair have varied widely. The most commonly used methods for fixation are transosseous sutures and suture anchors. [10] However, other techniques have been, such as suturing the tendon to the periosteum or the clavipectoral fascia, [11] the use of screws with spiked plastic washers and even barbed staples. [6]
Our experience and opinions are similar to those stated in the biomechanical article published by Hart et al., [12] which emphasizes the potential advantages of anchors comparing to the classic transosseous fixation. We introduce here, a variation using knotless suture anchors and a burred trough to dock the tendon into its anatomic insertion. To our knowledge, this is the first paper describing this transosseous equivalent repair for PM rupture.
 Surgical Technique Surgical Technique | |  |
Our approach to this type of injuries is through a careful physical exam and medical history. Conventional X-rays are used to rule out other injuries and/or recognize humeral bony avulsions. MRIs are routinely obtained. Although the diagnosis is normally confirmed after the physical exam, MRI usually provides the necessary information such as the rupture location and its characteristics (partial, full thickness, muscle belly, muscle-tendon junction, humeral avulsion).
Once the patient is identified in the preoperative holding area, the appropriate extremity is anesthetized through a supraclavicular brachial plexus block. The patient is positioned supine on the operating table in a modified beach chair position. Preoperative antibiotics are utilized.
A modified and inferiorly positioned deltopectoral incision about 4 cm in length is done. The cephalic vein is displaced laterally, and dissection is carried until the conjoined tendon is identified. With blunt dissection medially, the torn tendon is identified. Often, a large seroma is encountered around the tendon. The tendon is usually retracted medially. Occasionally, a thin veil of tissue/fascia still attached to the humeral insertion. We first bluntly dissect superficially as well as posteriorly to the ruptured heads until a 360° release is obtained. Two, number 2 ultra-resistant Fiber wire (Arthrex, Inc., Naples, FL, USA) locked sutures are placed within the bulk of the muscle tendon unit in a Krackow fashion to be able to bring this back to the insertion point without undue tension. A cortical trough is created just lateral to the biceps tendon using a small round burr. The trough is created approximated 2 cm in length, and to a depth where the cancellous bone just becomes apparent. After creating the trough, pilot holes are punched and tapped for two Peek Swivelock 5.5-mm anchors (Arthrex, Inc., Naples, FL, USA) [Figure 1]. One anchor is placed in the superior portion of the trough, and one is placed in the inferior portion of the trough. The previously placed sutures are passed into the corresponding anchor (superior sutures in the superior anchor, inferior sutures in the inferior anchor) [Figure 2]. The eyelets are passed into the pilot holes, with tension on the sutures. As the eyelets are placed into the humerus, the edge of the tendon is effectively docked in the trough. The PEEK anchors are screwed into lock the eyelets and sutures.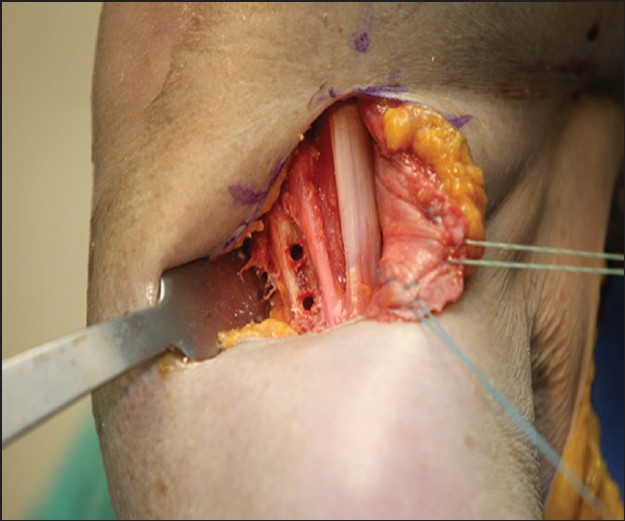 | Figure 1: Pectoralis major tendon held with two #2 Fiber wire© (Arthrex, Inc., Naples, FL, USA) locked sutures in a Krackow fashion. The humeral insertion site was properly prepared, creating a trough with a rounded burr at the anatomic insertion site, lateral to the biceps tendon
Click here to view |
 | Figure 2: Insertion of one of the knotless Swivelock© 5.5 anchor previously loaded with one of the #2 fiber wire© (Arthrex, Inc. Naples, FL, USA) sutures from the pectoralis major tendon
Click here to view |
Each suture from the tendon is tied to the corresponding eyelet suture in the anchor. The sutures from the superior anchor can then be tied to the sutures from the inferior anchor creating a fixed unit and increasing the pull-out strength [Figure 3]. At this point, it is advisable to test the external rotation and stability of the construct. Finally, the deltopectoral interval is closed with absorbable sutures and nonabsorbable subcuticular sutures are used for the skin. | Figure 3: Final result of the pectoralis major repair. The anatomic insertion site was recreated, lateral to the bicipital groove which is shown in the picture
Click here to view |
 Discussion Discussion | |  |
The first reported PM tear occurred in 1822; by 1980, approximately 100 cases had been reported. [8] The most recent systematic review included 67 articles reporting 365 cases of PM injuries. [13] Only 86 cases (24%) had appeared in publications before 1990, the remaining 279 cases (76%) had been reported in the last 20 years. Most of these reports are small series or case reports. Unfortunately, the meta-analysis of 112 PM injuries published by Bak et al.[5] in 2000 incorporated duplicate cases, which reduced the value of their data.
A systematic review by ElMaraghy and Devereaux of 365 cases provides useful information. They found tears of the PM were more common in active males 20-40 years of age (mean of 31 ± 9.9 years, ranges: 14-91). Only 11 PM ruptures were reported in women (mean of 85.4 ± 6.9 years, ranges: 73-97), 10 of whom were living in nursing homes. These ruptures likely occurred during assisted transfers or dressing, and were managed conservatively. [13]
The authors found that the indirect trauma was the reported mechanism in 83% of PM ruptures. Concentric muscle contraction with gymnastics, wrestling or jujitsu was reported in a small number of injuries. [13] The most common mechanism of injury was a maximal force applied in an eccentrically contracted PM muscle in abduction and external rotation of the shoulder. In 48% of the tears, the injury occurred during the bench press. Anabolic steroid use was mentioned in 11% and did not appear to be a major factor. [13] Sixty-two percent of injuries were reported as acute and 38% as chronic. ElMaraghy and Devereaux's analysis and determined that complete tears or avulsions made up 56% (206/365) of the injuries. In 67% of the cases, the rupture was intratendinous or at the tendon insertion. [13]
In the past, repair of the PM rupture has been a controversial issue. When the patient groups are corrected to include "delayed surgery" cases as patients for whom conservative treatment failed, the difference in outcomes between surgical and conservative management becomes even more favorable for surgical treatment. [5] McEntire et al. reported good to excellent results in up to 90% of patients treated with acute surgical repair. Results were judged good to excellent in only 70% of the patients treated nonoperatively. [11] Scott et al. used dynamometry to assess the muscle strength of four patients with PM rupture and demonstrated a significant loss of torque with conservative treatment. [14] For sedentary people or the elderly, conservative treatment might be satisfactory in many cases. [2] For complete tears, most surgeons now recommend surgery, especially in athletic individuals. [15],[16],[17]
When considering the appropriate timing for repair, Aδrimaa et al., [18] in a meta-analysis published in 2004 with 73 patients, confirmed that repairs within 8 weeks of injury resulted in significantly better outcomes than delayed surgery or conservative treatment. Age and type of rupture did not affect the final outcomes of the repair. Data analysis of previously published articles showed significant statistical differences in the outcome of the three different treatment groups: Conservative, acute operative, and delayed operative treatment (P < 0.001). In the acute operation group, 18 of 33 patients reported excellent results. Excellent results were reported by only 8 of 19 in the delayed operative group and 1 of 22 in the conservative treatment group. [18]
From a retrospective study of 17 patients, Schepsis et al.[10] concluded that all patients treated surgically fared significantly better, regarding pain and strength, than those treated nonoperatively. Delayed repair did not significantly compromise outcomes in this sample.
Multiple methods of repair have been described. Transosseous suturing of the tendon into a trough lateral to the bicipital groove is the most common. [10],[15] Other methods proven effective are barbed staples, [19] screw and washer fixation, [20] and more recently, suture anchors. [21] A case report by Miller et al. told of successful treatment using three Mitek suture anchors to repair a PM rupture. [21] Aδrimaa et al.[18] in 2004, reported on 33 cases of surgically treated tears and found outcomes were not significantly different when suture anchors were compared to transosseous sutures.
In 2011, Hart et al.[12] conducted a biomechanical study evaluating different repair techniques. They did not find significant differences between results of transosseous reinsertion technique and suture anchors repair, concluding that each had its advantages and disadvantages. The transosseous technique demonstrated good long-term clinical outcomes and still is considered the "Gold Standard." The main disadvantage in this technique is that sutures are tied over two bone bridges, lateral to the pectoralis insertion. With these techniques, there is a risk of fracture of the bony bridge with possible fixation failure. In the biomechanical study by Hart et al., [12] none of the suture anchors pulled loose from the bone, but half of the repairs failed at the bone bridge.
The PM footprint has thick cortical bone, ideal for placement of the anchors. However, suture anchor repairs are more expensive, and there is less contact between suture area and tendon to bone contact. In addition, local host reaction to metal or biodegradable anchors can occur, and metal anchors can interfere with imaging. [12] On the other hand, use of knotless suture anchors in our technique allows the tendon end to be brought into the trough, similar to the transosseous technique, yet has the strength inherent to the suture anchor technique.
 Conclusion Conclusion | |  |
This surgical technique allows the free tendon edge to be docked into a trough similar to the standard transosseous technique, minimizing the potential disadvantage of bony-bridge fracture while keeping the strength of the suture anchor repair. By tying the preloaded sutures to themselves as well as the sutures in the tendon, we enhance the strength of the construct. We believe this will lead to improved long-term outcomes. Surgeons may want to add this technique to their repertoire.
 References References | |  |
| 1. | Petilon J, Carr DR, Sekiya JK, Unger DV. Pectoralis major muscle injuries: Evaluation and management. J Am Acad Orthop Surg 2005;13:59-68.  |
| 2. | Wolfe SW, Wickiewicz TL, Cavanaugh JT. Ruptures of the pectoralis major muscle. An anatomic and clinical analysis. Am J Sports Med 1992;20:587-93.  |
| 3. | Fung L, Wong B, Ravichandiran K, Agur A, Rindlisbacher T, Elmaraghy A. Three-dimensional study of pectoralis major muscle and tendon architecture. Clin Anat 2009;22:500-8.  |
| 4. | Travis RD, Doane R, Burkhead WZ Jr. Tendon ruptures about the shoulder. Orthop Clin North Am 2000;31:313-30.  |
| 5. | Bak K, Cameron EA, Henderson IJ. Rupture of the pectoralis major: A meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc 2000;8:113-9.  |
| 6. | Quinlan JF, Molloy M, Hurson BJ. Pectoralis major tendon ruptures: When to operate. Br J Sports Med 2002;36:226-8.  |
| 7. | Lee J, Brookenthal KR, Ramsey ML, Kneeland JB, Herzog R. MR imaging assessment of the pectoralis major myotendinous unit: An MR imaging-anatomic correlative study with surgical correlation. AJR Am J Roentgenol 2000;174:1371-5.  |
| 8. | Tietjen R. Closed injuries of the pectoralis major muscle. J Trauma 1980;20:262-4.  [ PUBMED] |
| 9. | Kakwani RG, Matthews JJ, Kumar KM, Pimpalnerkar A, Mohtadi N. Rupture of the pectoralis major muscle: Surgical treatment in athletes. Int Orthop 2007;31:159-63.  |
| 10. | Schepsis AA, Grafe MW, Jones HP, Lemos MJ. Rupture of the pectoralis major muscle. Outcome after repair of acute and chronic injuries. Am J Sports Med 2000;28:9-15.  |
| 11. | McEntire JE, Hess WE, Coleman SS. Rupture of the pectoralis major muscle. A report of eleven injuries and review of fifty-six. J Bone Joint Surg Am 1972;54:1040-6.  [ PUBMED] |
| 12. | Hart ND, Lindsey DP, McAdams TR. Pectoralis major tendon rupture: A biomechanical analysis of repair techniques. J Orthop Res 2011;29:1783-7.  |
| 13. | ElMaraghy AW, Devereaux MW. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg 2012;21:412-22.  |
| 14. | Scott BW, Wallace WA, Barton MA. Diagnosis and assessment of pectoralis major rupture by dynamometry. J Bone Joint Surg Br 1992;74:111-3.  |
| 15. | Kretzler HH Jr, Richardson AB. Rupture of the pectoralis major muscle. Am J Sports Med 1989;17:453-8.  [ PUBMED] |
| 16. | Liu J, Wu JJ, Chang CY, Chou YH, Lo WH. Avulsion of the pectoralis major tendon. Am J Sports Med 1992;20:366-8.  |
| 17. | Pavlik A, Csépai D, Berkes I. Surgical treatment of pectoralis major rupture in athletes. Knee Surg Sports Traumatol Arthrosc 1998;6:129-33.  |
| 18. | Aärimaa V, Rantanen J, Heikkilä J, Helttula I, Orava S. Rupture of the pectoralis major muscle. Am J Sports Med 2004;32:1256-62.  |
| 19. | Egan TM, Hall H. Avulsion of the pectoralis major tendon in a weight lifter: Repair using a barbed staple. Can J Surg 1987;30:434-5.  |
| 20. | Kehl T, Holzach P, Matter P. Rupture of the pectoralis major muscle. Unfallchirurg 1987;90:363-6.  [ PUBMED] |
| 21. | Miller MD, Johnson DL, Fu FH, Thaete FL, Blanc RO. Rupture of the pectoralis major muscle in a collegiate football player. Use of magnetic resonance imaging in early diagnosis. Am J Sports Med 1993;21:475-7.  |
[Figure 1], [Figure 2], [Figure 3]
|
