| |


 |
| Year : 2015 | Volume
: 9
| Issue : 2 | Page : 47-51 |
|
|
|
|
|
ORIGINAL ARTICLE Performance of antegrade suture passers according to tendon thickness
Myung-Sun Kim1, Dong Whan Kim2, Young Eun Choi2, Larry Bachman Jr3, Sae Hoon Kim2
1 Department of Orthopedic Surgery, Chonnam National University College of Medicine, Chonnam National University Hospital, Gwangju, Korea
2 Department of Orthopedic Surgery, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea
3 Department of Bioengineering, University of California, San Diego, USA
Correspondence Address:
Sae Hoon Kim
Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul
Korea
 Source of Support: This work was funded by donation grant-aid-program in the institution: SNUH no. 3020130210 (2013-2705), Conflict of Interest: None
DOI: 10.4103/0973-6042.154760
 |
|
|
|
| Date of Web Publication | 8-Apr-2015 |
 Abstract Abstract | | |
Purpose: To determine the effect of tendon thickness on the needle penetration ability of four different designs of antegrade suture passers.
Materials and Methods: Four antegrade suture passers were tested: (a) ExpresSew II (Depuy Mitek Inc., Raynham, MA), (b) Arthrex Scorpion (Arthrex, Naples, FL), (c) Concept (Linvatec Corp, Largo, FL), and (d) ElitePass (Smith and Nephew Endoscopy, Andover, MA). Bovine tendons were divided into five thickness groups: 3, 5, 7, 9 and 11 mm. At each tendon thickness, we performed 15 trials with the suture loaded and 15 unloaded per device. Successful needle penetration was recorded, and in case of success, the exit point of the needle was noted in relation to the superior arm of the grasping component.
Results: All tested suture passing devices successfully penetrated tendon thicknesses of 3 and 5 mm. With the suture loaded, one device (Concept) only successfully penetrated 7 mm group tendons in 3/15 (20%) trials. Success rates at 9 mm with the suture loaded were 40% in ExpresSew II, 53% in Arthrex Scorpion, 0% in Concept and 53% in ElitePass. Among successful passages with a loaded suture in the 7 and 9 mm-groups, about 20-50% of passages were oblique, and the needle came out distal to the superior arm of grasping the component. No trial with any device succeeded with 11 mm tendons in the suture loading condition.
Conclusion: Using an antegrade suture passer during arthroscopic rotator cuff repair should be carefully considered when the torn end of the tendon is thicker than about 7-9 mm due to potential failure of needle penetration and/or too oblique a suture passage.
Level of Evidence: Controlled laboratory study.
Keywords: Antegrade suture passer, needle passage, rotator cuff repair, tendon thickness
How to cite this article:
Kim MS, Kim DW, Choi YE, Jr LB, Kim SH. Performance of antegrade suture passers according to tendon thickness. Int J Shoulder Surg 2015;9:47-51 |
 Introduction Introduction | |  |
Antegrade suture passers are one of the most widely used devices in arthroscopic rotator cuff repair. These devices combine tendon grasping, suture passage, and suture retrieval in one convenient step. They also use flexible, small-caliber needles that help to minimize damage to the tendon during surgery. This is important because the tendon-suture interface is the weakest point and accounts for the highest rates of fixation failure. [1],[2],[3],[4],[5],[6],[7] While different shapes and sizes of suture passing devices affect the tensile strength of repair, superior biomechanics are achieved when the caliber of tendon penetration is small, making antegrade suture passage an effective and convenient method. [7],[8]
An antegrade suture passer can be used without complication in the majority of cases. However, in our clinical experience, difficulties have been observed such as oblique passage of the needle, failure of the needle to completely penetrate the tendon, and needlepoint breakage. This is particularly evident when attempting to pass through the thick torn end of the rotator cuff in bursal side partial tears and acute tears.
There is not much information on how the thickness of the tendon affects antegrade suture passer performance, or at what thickness limit these devices no longer reliably succeed. There is also not much information on tendon thickness of the rotator cuff during surgery. In anatomical studies of the supraspinatus, the medial to the lateral width at the mid-point measures from 9.6 mm to 16 mm. [9],[10],[11],[12] Tendon thickness itself is probably smaller, nevertheless, in clinical experience the tendon can be up to approximately 10 mm thick.
The purpose of this study was to determine the effect of tendon thickness on the needle penetration ability of four different designs of commonly used antegrade suture passers. We hypothesized that the needle passage success rate of each device diminishes as tendon thickness is increased. Furthermore, based on these observations, we consider and discuss how device design may play a role in suture passage performance.
 Materials and methods Materials and methods | |  |
Fresh bovine forelimb tendons were acquired at the slaughterhouse, 150 tendons were measured with digital Vernier calipers (MAX-CAL, Japan Micrometer MFG Co., Osaka, Japan), and put into five groups according to thickness: 3 mm, 5 mm, 7 mm, 9 mm, and 11 mm. We used four commercially available antegrade suture passers [Figure 1] and [Figure 2]:
- ExpresSew II (Depuy Mitek Inc., Raynham, MA),
- Arthrex Scorpion (Arthrex, Naples, FL),
- Concept (Linvatec Corp, Largo, FL), and
- ElitePass (Smith and Nephew Endoscopy, Andover, MA).
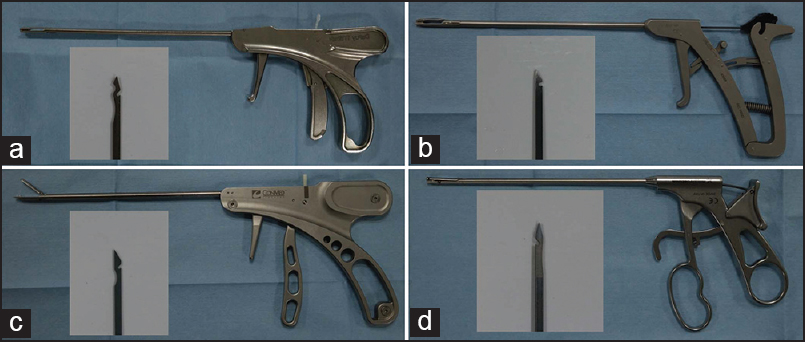 | Figure 1: Antegrade suture passers used in this study: (a) ExpresSew II, (b) Arthrex Scorpion, (c) Concept, and (d) ElitePass. Each small box shows an enlarged image of the flexible needle used in each device. All needles had a side opening that captured and delivered the suture through the tendon. Note that the superior grasping arm of device C did not have a locking mechanism and is therefore shown open in this image
Click here to view |
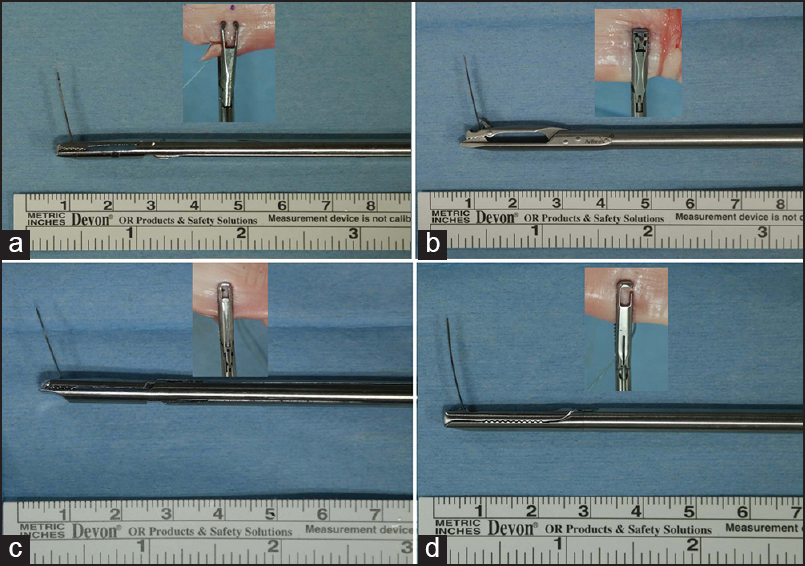 | Figure 2: Images show the tip of each suture passer with needle, and the small images show a superior view of the tip's grasping arm during needle penetration of a tendon: (a) ExpresSew II, (b) Arthrex Scorpion, (c) Concept, and (d) ElitePass. The superior grasping arms of devices A and B were offset to the shaft (hump back design), although device B had a much larger offset. Device A also had an opening at the front of the superior arm of the grasping component (small fi gure). Also note that the angle the needle projects relative to the shaft of the device is the least perpendicular in device C
Click here to view |
Each device incorporated a disposable flexible needle with a side hole [Figure 1] for delivering the suture strand upon penetrating the tendon. At each tendon thickness, we performed 15 trials with no suture (unloaded) and 15 with the suture (Hi-Fi® , Linvatec Corp, Largo, FL) loaded per device. A success was recorded if the needle penetrated the full thickness of the tendon. Furthermore, in case of success, the exit point of the needle was noted in relation to the window of the grasping component on the superior arm of the device [Figure 2]. The same author conducted all suture passing procedures.
Statistical analyses
All statistical analyses were performed using the SPSS software package (version 21.0, IBM SPSS Statistics, Chicago, IL). Success rate of each device at a certain thickness group was compared with Chi-square test. Statistical significance was set at a P < 0.05.
 Results Results | |  |
All tested suture passing devices successfully penetrated tendon thicknesses of 3 mm (3.01 ± 0.15 mm) and 5 mm (5.06 ± 0.19 mm) with and without suture loading, as well as at 7 mm (7.05 ± 0.14 mm) without suture [Table 1]. With the suture loaded, one device (Concept) only successfully penetrated the 7 mm group tendons in 3/15 (20%) trials. Failures occurred in all devices with the 9 mm (9.04 ± 0.21 mm) group. Success rates at 9 mm with the suture loaded were 40% in ExpresSew II, 53% in Arthrex Scorpion, 0% in Concept and 53% in ElitePass. Furthermore, among successful passages with a loaded suture in the 7 mm and 9 mm-groups, some passages were oblique and the needle came out distal to the superior arm of grasping component [Figure 3] and [Table 2]. The Concept device performed more poorly than the other three devices at 7 mm and 9 mm with suture loading, and at 9 mm without suture loading (P < 0.05). No trial with any device succeeded with 11 mm (11.12 ± 0.15 mm) tendons in the suture loading condition.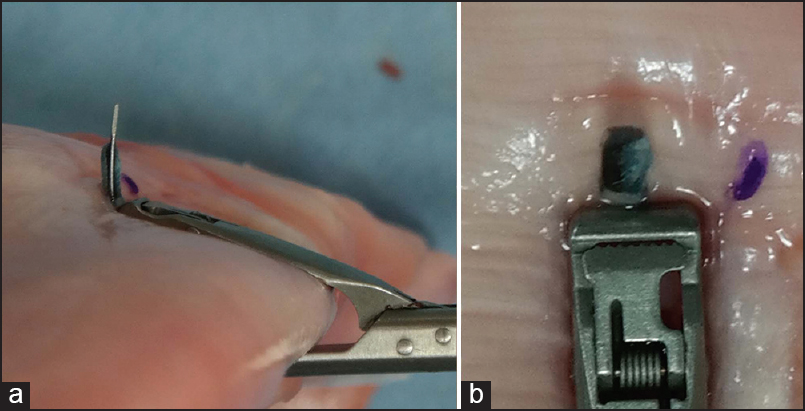 | Figure 3: A needle passage with suture is depicted using the Arthrex Scorpion, however, the needle passed in front of the superior arm of the grasping component. (a) Lateral view; (b) superior view
Click here to view |
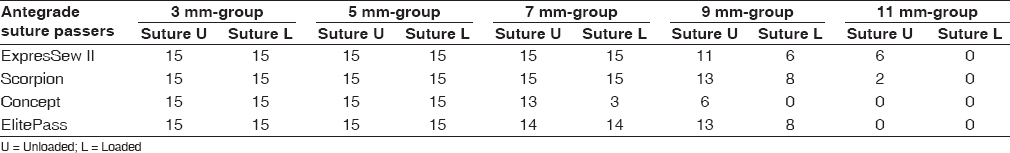 | Table 1: Number of successful passages in each device (out of 15 trials)
Click here to view |
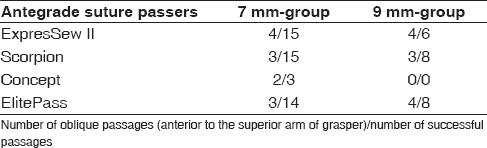 | Table 2: Number of oblique passages among successful passages in suture loading condition
Click here to view |
 Discussion Discussion | |  |
The results of this study show that the performance of antegrade suture passing devices begins to suffer from tendon thicknesses at 7 mm, fails approximately 50% or more of the time at 9 mm, and fails completely at 11 mm. Moreover, even if tendon penetration is successful, oblique passage occurs in 20% or more cases at 7 mm and about 50% of cases at 9 mm. When the needle exits distal to the superior grasping arm, the suture retrieving mechanism is rendered ineffective as demonstrated in [Figure 4] by one of our clinical observations. A suture passage, that is too oblique, may also affect repair biomechanics. Therefore, using an antegrade suture passer during rotator cuff repair should be carefully considered when the torn end of the tendon is thicker than about 7-9 mm.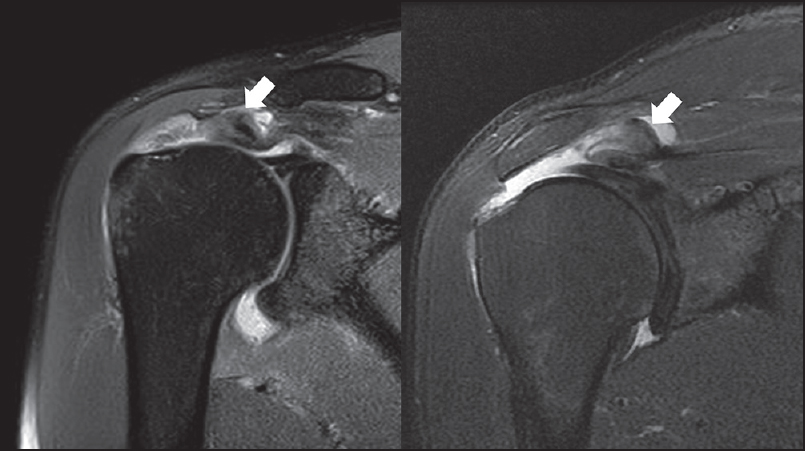 | Figure 4: Two magnetic resonance imaging scans of rotator cuff tears with a delaminated torn end of the tendon thicker than 10 mm (measured with imaging software)
Click here to view |
Our clinical arthroscopic repair data from December 2012 to November 2013 record 29 high-grade bursal side tears and 113 full-thickness rotator cuff tears. Preoperative magnetic resonance imaging measurements reveal that 41 cases (36.3%) of full-thickness tears and 14 cases (48.3%) of bursal side tears were >7 mm thick, and 9 cases (8.0%) of full-thickness tears and 4 cases (13.8%) of bursal side tears were >9 mm thick [Figure 4]. There is no appropriate method to measure tendon thickness intra-operatively, however, when it is measured roughly with probe sometimes the thickness is up to 10 mm [Figure 5]. In some of these cases, we had to convert to another type of suture passing method due to failure of antegrade suture passage [Figure 6] and [Figure 7].
We suggest further improvements to antegrade suture passer designs based on our observations. First, the superior grasping arm should be offset to the shaft. Then, the inferior arm of the grasper lies more horizontal to the tendon axis, allowing needle penetration more perpendicular to the tendon [Figure 8]. One design (device B) has this offset design [Figure 2]. However, more pronounced offset prevents tendon slippage in tendon bite. In medial row stitch of a double row repair, more tissue bite is needed. However, an additional offset is limited by the diameter of the portal or cannula in the antegrade suture passer. Second, the projection angle of the flexible needle should be more perpendicular to the handle/shaft of the device to limit oblique suture passage. Even if the needle projection were perpendicular, oblique passage would still occur because the tendon always has a certain thickness [Figure 9]. This could be minimized by using an offset as mentioned previously, or even by slightly angling the needle from perpendicular back toward the handle. Finally, the open front window on the grasping arm of one device in this study (ExpresSew II) helps prevents needle point jams [Figure 2] and [Figure 10], which we commonly experience at the front bar of the window when using closed-type devices.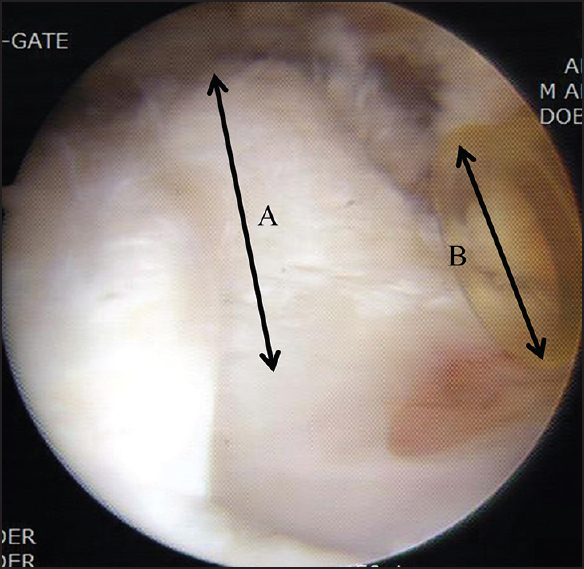 | Figure 5: Arthroscopic view of a high-grade bursal side rotator cuff tear showing that the torn end of the tendon (a) was thicker than the 8 mm diameter cannula (b)
Click here to view |
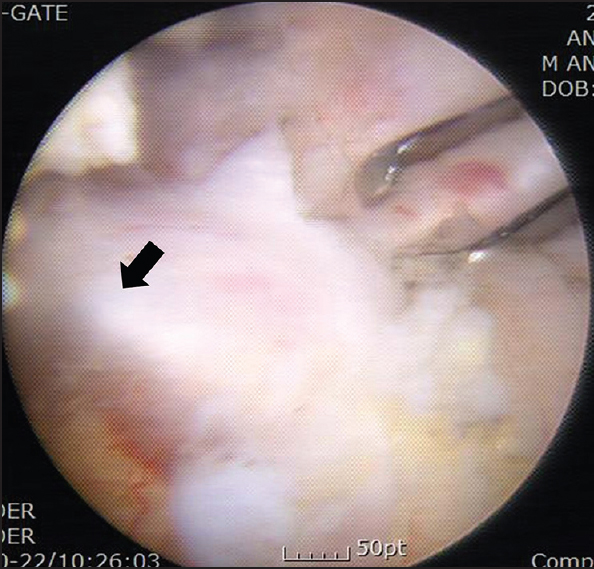 | Figure 6: Arthroscopic view of a rotator cuff tendon repair showing an unsuccessful antegrade needle passage. In this case, the tendon was thick and the needle penetrated at an acute angle such that the needle point slid far in front of the superior grasping window without emerging from the tendon (arrow)
Click here to view |
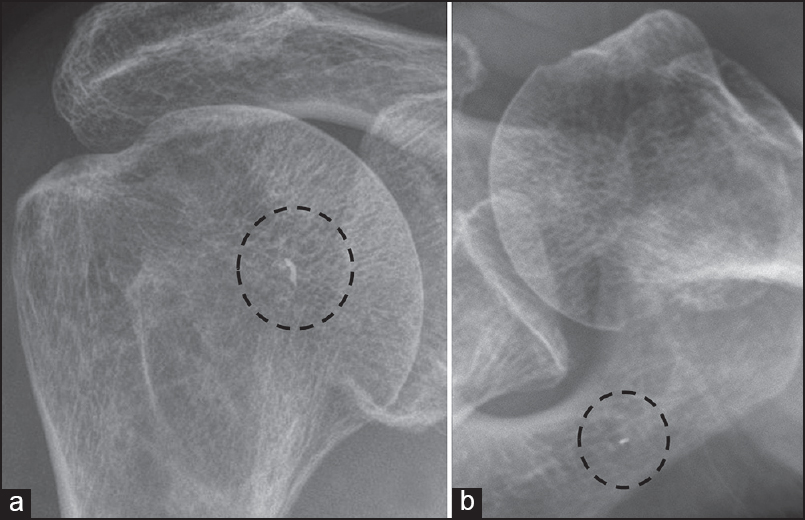 | Figure 7: (a) Anterior-posterior and (b) axillary lateral radiographs showing a broken needle tip (inside dotted circle) that could not be removed from the rotator cuff tendon
Click here to view |
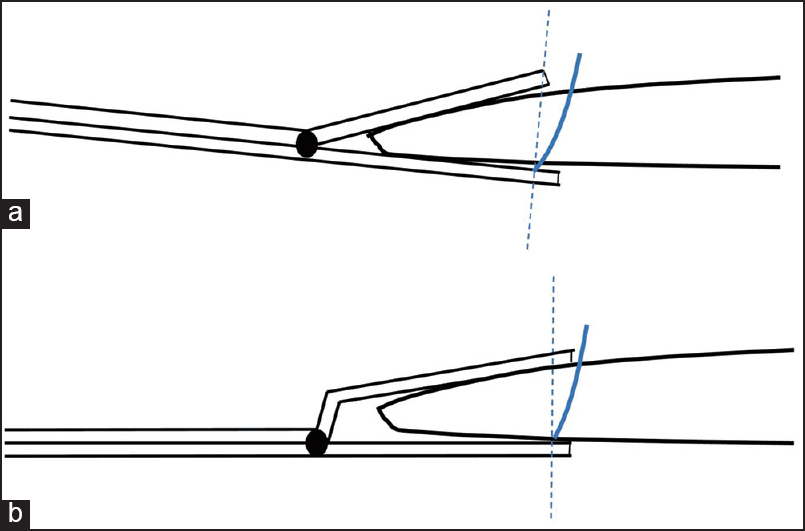 | Figure 8: A side-view diagram of the grasping components of two antegrade suture passing devices: (a) Without offset, and (b) with offset. The dotted line shows a desired needle projection perpendicular to the inferior arm and shaft of the device. However, we commonly observed the needle penetrate the tendon distal to the grasping window, as represented by thesolid line. In a thick tendon as illustrated in this diagram, even when the needle penetrates perpendicular to the device it travels obliquely through the tendon and exits distal to the superior arm of the grasper. This effect is less when using devices with offset grasping arms (B)
Click here to view |
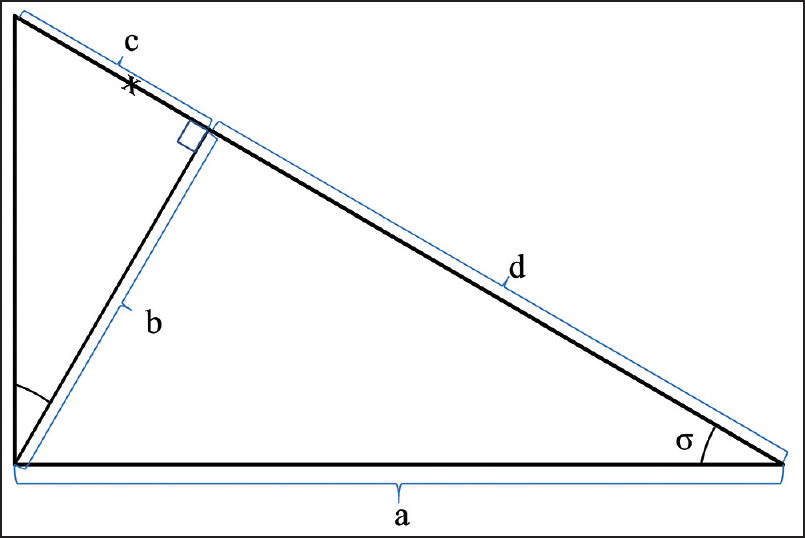 | Figure 9: Schematic drawing of the grasping arms of a suture device without offset (large triangle sides a and d) open at a 30°angle (σ) around a 10 mm thick tendon (b). If the distance between the device hinge and needle (vertical unlabeled line) is 2 cm (a), then the desired needle exit point is 2 cm along sides (d) and (c) at position (x). If the needle penetrates perpendicular to the lower limb of the grasper (side a), it will exit at the top corner of the triangle in the diagram. This point is 2.31 cm from the hinge (d = 1.73 cm + c = 0.58 cm), or 0.31 cm distal to the desired needle exit point (x)
Click here to view |
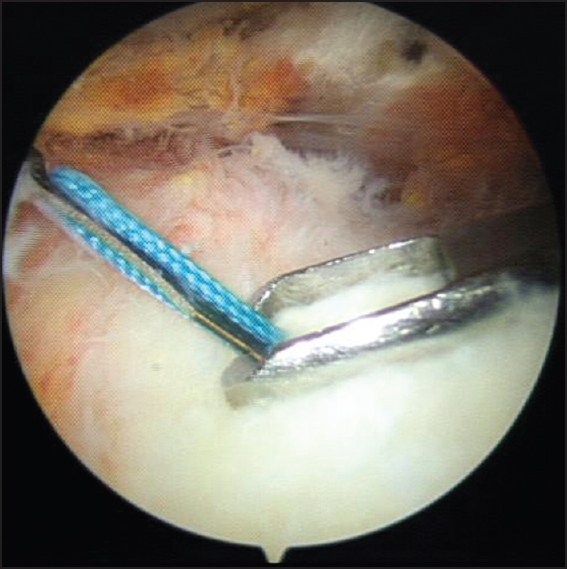 | Figure 10: Arthroscopic view of an antegrade suture passage through the rotator cuff tendon demonstrating an oblique penetration of the needle. Note that the device (ExpresSew II) had an open-type window on the superior arm of the grasping component. In closed-window devices the needle occasionally jammed on the front bar of the window during rotator cuff repair and during trials in this study
Click here to view |
Limitation of this study is that human rotator cuff tendons could have various characteristics not reflected by studying bovine tendons. However, the rotator cuff tendons in human cadaveric specimens are typically not torn and do not offer variable thickness to evaluate threshold of suture passer's performance. Additionally, we tested one device of each model, but two devices of the same model may produce different results. Lastly, device performance may have been more favorable with our experimental design compared to during a surgical arthroscopic procedure.
In summary, performance of antegrade suture passer is not reliable past a tendon thickness of 9 mm. This is most evident in the suture-loading condition, and when using the device with the least perpendicular needle projection angle.
 Conclusions Conclusions | |  |
Using an antegrade suture passer during rotator cuff repair should be carefully considered when the torn end of the tendon is thicker than about 7-9 mm due to an increased risk of needle penetration failure and/or too oblique a suture passage.
 Acknowledgment Acknowledgment | |  |
This work was done by donation grant-aid-program in the institution: SNUH no. 3020130210 (2013-2705).
 References References | |  |
| 1. | Schneeberger AG, von Roll A, Kalberer F, Jacob HA, Gerber C. Mechanical strength of arthroscopic rotator cuff repair techniques: An in vitro study. J Bone Joint Surg Am 2002; 84-A:2152-60.  |
| 2. | Bisson LJ, Manohar LM. A biomechanical comparison of the pullout strength of No 2 FiberWire suture and 2-mm FiberWire tape in bovine rotator cuff tendons. Arthroscopy 2010;26:1463-8.  |
| 3. | Burkhart SS, Diaz Pagàn JL, Wirth MA, Athanasiou KA. Cyclic loading of anchor-based rotator cuff repairs: Confirmation of the tension overload phenomenon and comparison of suture anchor fixation with transosseous fixation. Arthroscopy 1997;13:720-4.  |
| 4. | Burkhart SS, Fischer SP, Nottage WM, Esch JC, Barber FA, Doctor D, et al. Tissue fixation security in transosseous rotator cuff repairs: A mechanical comparison of simple versus mattress sutures. Arthroscopy 1996;12:704-8.  |
| 5. | Denard PJ, Burkhart SS. Techniques for managing poor quality tissue and bone during arthroscopic rotator cuff repair. Arthroscopy 2011;27:1409-21.  |
| 6. | Gerber C, Schneeberger AG, Beck M, Schlegel U. Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg Br 1994;76:371-80.  |
| 7. | Ponce BA, Hosemann CD, Raghava P, Tate JP, Sheppard ED, Eberhardt AW. A biomechanical analysis of controllable intraoperative variables affecting the strength of rotator cuff repairs at the suture-tendon interface. Am J Sports Med 2013;41:2256-61.  |
| 8. | Chokshi BV, Kubiak EN, Jazrawi LM, Ticker JB, Zheng N, Kummer FJ, et al. The effect of arthroscopic suture passing instruments on rotator cuff damage and repair strength. Bull Hosp Jt Dis 2006;63:123-5.  |
| 9. | Dugas JR, Campbell DA, Warren RF, Robie BH, Millett PJ. Anatomy and dimensions of rotator cuff insertions. J Shoulder Elbow Surg 2002;11:498-503.  |
| 10. | Curtis AS, Burbank KM, Tierney JJ, Scheller AD, Curran AR. The insertional footprint of the rotator cuff: An anatomic study. Arthroscopy 2006;22:609.e1.  |
| 11. | Ide J, Maeda S, Takagi K. Arthroscopic transtendon repair of partial-thickness articular-side tears of the rotator cuff: Anatomical and clinical study. Am J Sports Med 2005;33:1672-9.  |
| 12. | Ruotolo C, Fow JE, Nottage WM. The supraspinatus footprint: An anatomic study of the supraspinatus insertion. Arthroscopy 2004;20:246-9.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10]
[Table 1], [Table 2]
|
