| |


 |
| Year : 2015 | Volume
: 9
| Issue : 2 | Page : 60-67 |
|
|
|
|
|
REVIEW ARTICLE Reverse shoulder arthroplasty. Part 2: Systematic review of reoperations, revisions, problems, and complications
Eduard Alentorn-Geli1, Gonzalo Samitier2, Carlos Torrens1, Thomas W Wright2
1 Department of Orthopaedic Surgery and Traumatology, Parc de Salut Mar - Hospital del Mar & Hospital de l'Esperança, Universitat Autonoma de Barcelona (UAB), Barcelona, Spain
2 Orthopaedics and Sports Medicine Institute, Department of Orthopaedics and Rehabilitation, University of Florida, Gainesville, Florida, USA
Correspondence Address:
Thomas W Wright
Orthopaedics and Sports Medicine Institute, Department of Orthopaedics and Rehabilitation, University of Florida, 3450 Hull Road, Gainesville, Florida, 32611
USA
 Source of Support: None, Conflict of Interest: None  | 4 |
DOI: 10.4103/0973-6042.154771
 |
|
|
|
| Date of Web Publication | 8-Apr-2015 |
 Abstract Abstract | | |
Purpose: Many factors influence the reoperations, revisions, problems, and complications of reverse shoulder arthroplasty (RSA). The purpose of this study was to compare those depending on the surgical approach, type of prosthesis, and indication for surgery through a comprehensive, systematic review.
Materials and Methods: A literature search was conducted (1985 to June 2012) using PubMed, CINAHL, EBSCO-SPORTDiscus, and Cochrane Central Register of Controlled Trials. Levels I-IV evidence, in-vivo human studies (written in English with minimum of 2 years of follow-up and sample size of 10 patients) reporting reoperations, revisions, problems, and complications after RSA were included. The data obtained were analyzed depending on the surgical approach, type of prosthesis (with medialized or lateralized center of rotation), or indication for surgery.
Results: About 37 studies were included involving 3150 patients (mean [SD] percentage of females, age, and follow-up of 72% [13], 71.6 years [3.8], and 45 months [20], respectively). Use of deltopectoral approach and lateralized prostheses had significantly higher risk of need for revision surgery (P = 0.008) and glenoid loosening (P = 0.01), but lower risk of scapular notch (P < 0.001), compared with medialized prostheses with same approach. RSA for revision of anatomic prosthesis demonstrated higher risk of reoperation (P < 0.001), revision (P < 0.001), hematoma (P = 0.001), instability (P < 0.001), and infection (P = 0.02) compared with most of the other indications.
Conclusions: Lateralized prostheses had significantly higher glenoid loosening and need for revision surgery, but a significantly lower rate of scapular notching compared to medialized prostheses. The risk of reoperations, revisions, problems, and complications after RSA was increased in revision cases compared with other indications.
Level of Evidence: Level IV.
Keywords: Complications, reoperations, reverse shoulder arthroplasty, revisions, systematic review
How to cite this article:
Alentorn-Geli E, Samitier G, Torrens C, Wright TW. Reverse shoulder arthroplasty. Part 2: Systematic review of reoperations, revisions, problems, and complications. Int J Shoulder Surg 2015;9:60-7 |
 Introduction Introduction | |  |
Reverse shoulder arthroplasty (RSA) is a common surgery for degenerative joint disease with deficient rotator cuff. [1],[2],[3] Theoretical advantages of RSA are increased lever arm of the deltoid muscle through a medialized center of rotation of the prosthesis (increasing deltoid efficiency), increased prosthetic stabilization through humeral lengthening (increasing deltoid tension), and decreased mechanical torque at the glenoid component (decreasing glenoid loosening). [4],[5] RSA is indicated for cuff tear arthropathy, [1],[2],[3],[6],[7],[8],[9] although indications have extended to fracture sequelae, rheumatoid arthritis (RA), acute fractures, tumors, massive cuff tears, or as a revision procedure for failed anatomic or reverse prostheses. [5],[10],[11] Zumstein et al. conducted a systematic review in which they found the type of approach and the indication for RSA influenced the incidence of reoperation, revision surgery, problems, and complications. [5] However, the influence of the type of prosthesis (either with medialized or lateralized center of rotation) associated with the type of approach was not reported. The term of medialized or lateralized design for RSA can be confusing, as all the designs for RSA medialize the center of rotation in order to optimize the deltoid function. There are designs where this characteristic is more pronounced than others, and theoretically a more medialized or more lateralized RSA design could have functional and clinical implications. It has been shown that the location of the center of rotation may be associated with the occurrence of problems and complications, [4],[12] and thus may influence the reoperation and revision-surgery rates. In addition, the study by Zumstein et al. included studies up until 2008, and there have been many publications in the last 4 years regarding RSA.
The principal purpose of this systematic review was to compare the reoperations, revisions, problems, and complications depending on the type of prosthesis, type of approach, and indication for surgery. It was hypothesized that reoperations, revisions, problems, and complications are modified by these factors.
 Materials and Methods Materials and Methods | |  |
The methodology of this study was reported following the PRISMA Statement for systematic review and meta-analysis. [13] All human studies reporting reoperations, revisions, problems, and complications in patients treated with primary or revision RSA were assessed for eligibility. Both print text and electronic manuscripts were eligible for inclusion. Studies were included if they had a level of evidence between I and IV, were written in English, had a minimum of 2 years of follow-up and had a minimum sample size of 10 patients. Studies only reporting clinical outcomes, nonoriginal articles, or studies with insufficient data were excluded. The literature-search strategy has been previously reported. [14]
The reoperations, revisions, problems, and complications rates were extracted from all studies systematically using a table template. The data extraction methodology has been reported in a previous publication. [14] The definition of problems and complications was based on the Zumstein et al. article. [5] The percentage of patients needing reoperation or revision surgery was collected. The definition of reoperation and revision surgery was based on the Zumstein et al. article. [5] The percentage of patients developing each problem was collected and included the following: glenoid radiolucency, humeral radiolucency, scapular notch, hematoma, heterotopic calcification, osteophytes, and others. The percentage of patients developing each complication was also collected, and included the following: glenoid loosening, humeral loosening, component dissociation, scapular fracture, spine fracture, acromial fracture, coracoid fracture, glenoid fracture, humeral fracture, hardware failure, instability, infection, nerve injury, thrombosis, and others. A 0% of a problem or complication was considered whenever the authors stated that none of their patients had that problem or complication, whereas the value was left as unreported whenever the authors did not mention the problem or complication. Fracture-related complications were considered for both intraoperative and postoperative periods. Nerve injury was considered either a transient neuroapraxia or definitive nerve damage with sequelae. Relevant information regarding level of evidence, type of prosthesis (either with medialized or lateralized center of rotation), type of approach (either deltopectoral or superolateral), indication for RSA, sample size, percentage of females in the sample, follow-up, and age of patients was extracted from all studies.
Descriptive statistics was used to summarize all collected information. Data were presented using comparative tables according to the type of surgical approach (deltopectoral or superolateral), type of prosthesis employed (either with medialized or lateralized center of rotation), and type of indication for RSA. An indirect between-studies comparison was conducted. For the comparison of reoperations, revisions, problems, and complications depending on the type of approach and type of prosthesis, a risk analysis adjusted by length of follow-up and provided with the odds ratio (with 95% confidence interval) was conducted. For the comparison depending on each indication for RSA (reported as the number of patients with the percentage with respect to the specific subgroup), a Chi-square or Fisher exact test was employed as needed. The alpha level was set at 0.05. Statistical analyses were performed using SPSS v21 (SPSS Inc., Chicago, IL, USA).
 Results Results | |  |
The PubMed search yielded 329 citations, of which 174 were clinical studies in humans. About 34 met inclusion criteria, and additional database searches and review of the reference list of included articles yielded a final number of 37 articles included in the analysis of reoperations, revisions, problems, and complications [Figure 1]. [6],[7],[8],[9],[10],[15],[16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41],[42],[43],[44],[45],[46] From all 174 articles assessed for eligibility, the senior author had to review three of them because of disagreement between the two authors conducting the systematic review. These two authors had no disagreement on data extraction for the 37 included studies.
The 37 studies were grouped depending on the approach and type of prosthesis: deltopectoral approach associated with a prosthesis with a medialized center of rotation (DM group; n = 19 studies), deltopectoral approach associated with a prosthesis with a lateralized center of rotation (DL group; n = 7 studies), and a combination of approaches associated with a prosthesis with a medialized center of rotation (CM group; n = 11 studies). The latter group was created because the authors employed different approaches, but reoperations, revisions, problems or complications were not specified depending on the type of approach (all these studies employed a prosthesis with a medialized center of rotation). A unique group with the superolateral approach was not created because only one study exclusively employed this approach. [12] The studies included a total sample of 3150 patients with a mean percentage of females, age, and follow-up of 72% (13), 71.6 years (3.8), and 45 months (20), respectively. The DM group involved a total of 1188 patients with a mean (SD) percentage of females, age, and follow-up of 71.4% (12.9), 71.4 years (4.1), and 40.3 months (13.5), respectively. The DL group involved a total of 219 patients with a mean (SD) percentage of females, age, and follow-up of 66.1% (19), 69.9 years (2.3), and 38.6 months (7), respectively. The CM group involved a total of 1721 patients with a mean (SD) percentage of females, age, and follow-up of 76.8% (8.1), 73.2 years (3.7), and 57.7 months (29.9), respectively. There were no significant differences in percentage of females and age of patients among the three groups, but the CM group had a follow-up significantly longer than the other two (P < 0.05). The intergroup comparative analysis of reoperations, revisions, problems, and complications was possible for only those parameters most commonly reported in the reviewed studies, which included the following: reoperations, revision surgery, scapular notch, hematoma, glenoid loosening, humeral loosening, acromial fracture, instability, infection, and nerve injury. The percentage of reoperations, revisions, problems, and complications for the DM, DL, and CM groups were the following: reoperation 4.8%, 7.8%, and 3.7%, respectively; revision surgery 5.6%, 10.5%, and 3.8%, respectively; scapular notch 43.8%, 4.6%, and 50.8%, respectively; hematoma 1.3%, 1.4%, and 1.3%, respectively; glenoid loosening 1.8%, 4.6%, and 3.4%, respectively; humeral loosening 1%, 0.9%, and 2.1%, respectively; acromial fracture 1.2%, 2.3%, and 0.6%, respectively; instability 4.4%, 3.2%, and 2.8%, respectively; infection 2.8%, 3.7%, and 3.4%, respectively; and nerve injury 2.9%, 0.5%, and 0.6%, respectively. [Table 1] shows risk analysis (adjusted for length of follow-up) depending on the approach and type of prosthesis.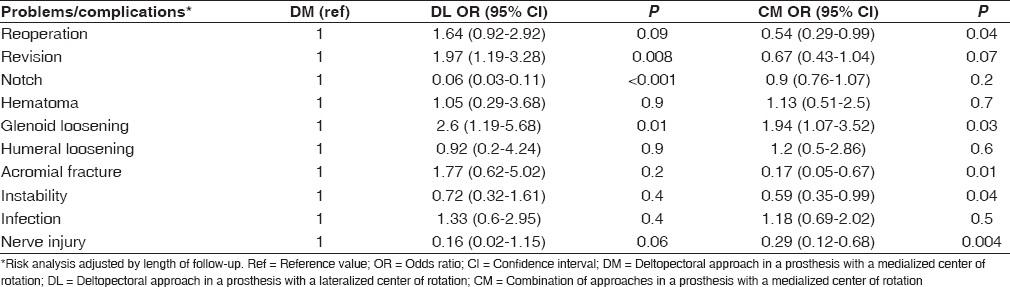 | Table 1: Risk of problems and complications of reverse shoulder arthroplasty depending on the type of approach and implant employed
Click here to view |
For the analysis of reoperations, revisions, problems, and complications depending on the indication for RSA, not all 37 studies were included because results were not always specified by indication. Thus, the number of studies included (total subjects involved) by indications for RSA were the following: cuff tear arthropathy 10 (1016), failed rotator cuff repair 3 (91), fracture sequelae 4 (83), RA 4 (60), revision of anatomic prosthesis 8 (222), and revision of reverse prosthesis 1 (14). Mean (SD) for percentage of females, age, and follow-up depending on indications were the following: cuff tear arthropathy 74.9% (10.6), 72 years (3.6), and 48 months (29.7), respectively; failed rotator cuff repair 69% (19.8), 68 years (2.8), and 46 months (5.7), respectively; fracture sequelae 70% (9.3), 73.2 years (6.2), and 37.7 months (10), respectively; RA 87.7% (12), 68.2 years (3.6), and 56 months (27.2), respectively; and revision of anatomic prosthesis 66.5% (11.7), 68.5 years (2.9), and 40 months (5), respectively. For revision of reverse prosthesis, only one study reported reoperations, revisions, problems, and complications data, with a percentage of females, and intrastudy mean (SD) of age and follow-up of 28%, 70.6 years (8.7), and 33 months (11.2), respectively. [Table 2] compares the reoperations, revisions, problems, and complications depending on the indications for RSA in the included studies.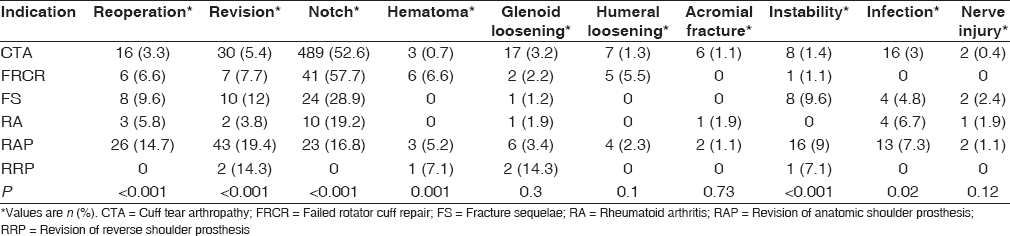 | Table 2: Problems and complications of reverse total shoulder arthroplasty depending on indications
Click here to view |
 Discussion Discussion | |  |
The purpose of this study was to compare the reoperations, revisions, problems, and complications of RSA depending on the type of prosthesis (with either more medialized or lateralized center of rotation), type of approach, and indication for surgery. The principal finding was that prostheses with a lateralized center of rotation had a significantly higher glenoid loosening and the need for revision surgery, but significantly lower rates of scapular notching, compared to medialized prostheses. In addition, indications for surgery influenced the rate of reoperations, revisions, problems, and complications in the following ways: reoperations were higher in revision of anatomic prosthesis and revision of reverse prosthesis; revisions were higher in revision of anatomic prosthesis and fracture sequelae; scapular notch was higher in cuff tear arthropathy and failed rotator cuff repair; hematoma was higher in failed rotator cuff repair, revision of anatomic prosthesis, and revision of reverse prosthesis; instability was higher in revision of anatomic prosthesis and failed rotator cuff repair; and infection was higher in revision of anatomic prosthesis, RA, and fracture sequelae.
Patients with degenerative shoulder disease in whom an RSA is planned are complex cases or revisions of a previous surgery or prosthesis. Although the classical indication for RSA is cuff tear arthropathy, indications are now extended to primary osteoarthritis with degenerative cuff tear, massive cuff tear, failed rotator cuff repair, RA, fracture sequelae, posttraumatic osteoarthritis, revision from anatomic or reverse prosthesis, avascular necrosis, tumors, or fractures as a primary treatment. [5],[41] The surgical procedure is highly complex, and in many cases there are no good alternatives. Although one may argue that RSA has a high risk of problems and complications, potential benefits and lack of reliable surgical alternatives makes RSA a relevant option in certain shoulder disorders compared to anatomic arthroplasties. [11] Both types of RSA prostheses (with medialized and lateralized center of rotation) employed for many indications have demonstrated excellent clinical and functional outcomes. [6],[7],[9],[10],[24],[41].[42].[43],[45],[47] The investigation of reoperations, revisions, problems, and complications is very relevant to adequately understanding potential ways to prevent complications and improve outcomes of RSA.
To our knowledge, this is the first attempted "meta-analysis" aimed to compare reoperations, revisions, problems, and complications depending on the type of prosthesis, type of approach, and an indication for surgery. One of the main contributions of this study is that it provides a statistical comparison between two different types of prosthesis controlled by age, gender, approach, and length of follow-up. The study published by Zumstein et al. was descriptive in nature with few comparisons made through inferential statistics. It also included studies up until 2008, which excludes recent, evolving improvements in prostheses' design and surgeons' experience. Our investigation is an up-to-date systematic review of the literature and attempted "meta-analysis."
This study's results are in agreement with previous literature. [5] However, there are some limitations that must be identified. First, the attempted meta-analysis was indirect in nature. Given that almost all included studies were therapeutic case series, this study corresponds to an indirect level-IV comparison. The potential influence of the interstudy heterogeneity and noncontrolled factors influencing the rate of reoperations, revisions, problems, and complications are thus not negligible. Second, most of the studies did not disclose the reoperations, revisions, problems, and complications rate depending on the indications for surgery, so the meta-analysis of indications had to be considered separately to avoid a significant decrease in the number of studies included in the comparison. Thus, only the type of prosthesis and type of approach could be meta-analyzed altogether. Third, it must be noted that not all studies used the same definitions for reoperations, revisions, problems, and complications that were employed in this study. Events considered problems in this study were simply classified as complications in others. [6],[9],[10],[21],[30],[32],[33],[36],[43] Similarly, some authors used "reoperation" and "revision" interchangeably. [9],[20],[24],[25],[30],[31],[33] This may decrease the accuracy of the comparison between the results of this study and those from existing literature. This concern does not affect the accuracy of the analysis in this study, as special attention was paid when collecting data from all included studies to adequately classify reoperations, revisions, problems, and complications according to Zumstein et al.'s [5] definitions and provide adequate homogenization.
In this study, the influence of the type of approach on the reoperations, revisions, problems, and complications of RSA could not be well-determined. Some studies used a combination of approaches and the reoperations, revisions, problems, and complications were not specified depending on whether the approach was deltopectoral, superolateral, transacromial or through a clavicle osteotomy. Therefore, some studies were grouped as CM to refer to studies using a combination of approaches (and a medialized prosthesis). In some ways, differences between groups' DM (deltopectoral approach and medialized prosthesis) and CM may be explained by differences in the type of approach, as the prostheses in both groups had a medialized center of rotation. However, considering the CM has a combination of approaches rather than a unique superolateral approach, no clear conclusions can be drawn regarding its influence on the reoperations, revisions, problems, and complications of RSA. It seems the rate of problems and complications of the clavicle osteotomy and the transacromial approach is high. [2],[5],[8],[48],[49],[50] Regarding deltopectoral and superolateral approaches, Zumstein et al. found that the former had higher rates of reoperations, revisions, problems, and complications compared to the latter. [5] For specific complications, these authors found that the deltopectoral approach had the highest rate of instability (97.3% of shoulders with this complication were operated through this approach). [5] However, a direct causal-effect relationship between the deltopectoral approach and instability cannot be established, as the version of humeral and glenoid components and the status of the subscapularis (preoperative degenerative rupture of fatty infiltration) may be influencing factors. Nevertheless, the subscapularis release and repair may be a major factor related to instability in the deltopectoral approach; several authors have recommended adequate intraoperative protection or repair before skin closure. [6],[9],[42] Regarding scapular notch, Zumstein et al. found that the rate in the superolateral approach was higher compared to the deltopectoral approach (77% and 49%, respectively, with no P value provided). [5] This higher risk in the superolateral approach has been reported by others. [15],[28],[34] The risk was especially increased if the notch extended to or beyond the inferior screw. [15],[34] Some authors speculate that in the superolateral approach, the baseplate tends to be placed higher on the glenoid and with superior tilt, [5],[51] thus potentially explaining the higher risk compared with the deltopectoral approach. The superolateral approach has also been related to an increased risk of inferior scapular spurs. [34] This is related to a more difficult release of the triceps from the inferior glenoid that would make the subject prone to a traction osteophyte in this area. [39] No clear conclusions can be elaborated because the approach could not be isolated in the intergroup comparison. More research on the surgical approach's influence on reoperations, revisions, problems, and complications are necessary.
The influence of the type of prosthesis on problems and complications has only been studied in a systematic review by Zumstein et al. [5] The authors found that medialized prostheses had more scapular notching (no P value provided) but less glenoid radiolucency lines (no P value provided) and aseptic glenoid loosening (P = 0.025) than lateralized prostheses. [5] These results are consistent with those obtained in the statistical analysis attempted in this investigation, as a statistically significant increased risk of scapular notching (P < 0.001) and decreased risk of glenoid loosening (P = 0.01) in the medialized compared to the lateralized prostheses was found. However, the Zumstein et al. study did not assess the rate of reoperations and revisions depending on the type of prosthesis. The present investigation demonstrated that lateralized prostheses had a higher risk of needing a revision surgery compared to medialized prostheses (P = 0.008). This result might be attributed to the increased torque or shear force applied to the glenosphere-baseplate interface in lateralized prostheses, especially with older designs. [5],[7],[52],[53] Although there has been some concern about the increased risk of glenoid loosening related to scapular notch, [1],[8],[12],[54] this could not be concluded from either the Zumstein et al. [5] study or the present investigation. The absence of a relationship between scapular notch and glenoid loosening has been reported by some original studies. [28],[34],[42] In addition, whereas some studies have observed worse clinical and functional outcomes in patients with scapular notch, [8],[39] more studies have failed to demonstrate this relationship. [6],[9],[15],[35],[40],[41],[46],[51] Several methods have aimed to decrease scapular notch: lowering prosthesis-scapular neck angle and peg-glenoid distance, [39] lowering glenometaphyseal angle, [19] lowering the baseplate to the inferior border of the scapula, [33] and using an eccentric glenosphere. [18] However, it is likely that the use of lateralized prostheses would be more efficient at preventing scapular notch than the glenosphere-baseplate positioning, as Holcomb et al. found that an increased prosthesis-scapular neck angle led to notch in medialized but not lateralized prostheses. [10]
The comparison between types of prostheses in the present investigation was controlled by several factors - age, gender, approach, and follow-up. However, the potential bias for lateralized prostheses must be recognized. Early designs of prostheses with lateralized center of rotation had high rates of glenoid loosening, attributed to increased torque at the bone-implant interface, [7] leading to biomechanical investigations to improve the design. After the inclusion of a 5-mm locking peripheral screw and a 15° inferior tilt of the baseplate (both design and technique modifications), Cuff et al. published a new series of patients treated with new-generation lateralized RSA prostheses and demonstrated that the rate of glenoid loosening and failure was decreased. [17] These were subsequently reproduced by Mulieri et al., who found no cases of baseplate failure in novel designs, but 11.8% in older prostheses, leading to an overall failure rate of 6.7%. [36] Although it seems that complications related to loosening and failure of implants may be increased with respect to medialized prostheses, [5] it might be argued that the differences between both types of prostheses would have been reduced by only including the improved models of the lateralized prostheses. Prostheses with medialized center of rotation have also improved over the years (with inclusion of a Morse taper and a new central screw to improve component fixation), [48] but no studies with older designs of these type of prostheses have been included in the present investigation. Whether new generation lateralized prostheses increase the risk of glenoid loosening compared to medialized prostheses needs further research.
The analysis of reoperations, revisions, problems, and complications depending on indications for surgery did not account for other factors potentially influencing the results (type of prosthesis, type of approach, length of follow-up, among others). Considering these limitations, the present study demonstrated that the type of indication influenced the rate of reoperations, revisions, problems, and complications. Specifically, there was a generally higher rate in revision surgery (changing an anatomic or reverse prosthesis to an RSA) compared to nonrevision procedures. This finding is consistent with previous literature. Werner et al. found that patients undergoing RSA as a revision procedure had a higher rate of complications compared to primary cases or patients undergoing RSA after a failed previous nonprosthetic procedure. [9] However, no P value was provided and the differences were likely nonstatistically significant due to small sample size (low number of complications). Need for reoperation in patients with previous surgery (either prosthetic [38%] or nonprosthetic [40%] procedures) was higher compared to primary RSA (18%; no P value provided). Furthermore, the need for revision surgery was higher in patients with previous surgery compared to primary cases (no P value provided). These results are similar to those obtained by Boileau et al., who found that complications and need for reoperations or revision surgery were higher in patients in the revision group compared with those undergoing RSA for cuff tear arthropathy or fracture sequelae. [6] Interestingly, Wall et al. were able to find a statistically significant difference for this specific comparison: there were 36.7% of complications in the revision compared with 13.3% in the primary procedure group (P < 0.001). [42] The present investigation was able to find significant differences for specific problems and complications. Thus, hematoma was higher in failed rotator cuff repair, revision of anatomic prosthesis, and revision of reverse prosthesis, instability was higher in revision of anatomic prosthesis and failed rotator cuff repair, and infection was higher in revision of anatomic prosthesis, RA, and fracture sequelae. In addition, reoperations were higher in revision of anatomic prosthesis and revision of reverse prosthesis and revisions higher in revision of anatomic prosthesis and fracture sequelae. This study also observed that scapular notch was higher in cuff tear arthropathy and failed rotator cuff repair compared to other indications. This finding is similar to a previous investigation that demonstrated that the incidence of the scapular notch increased in cuff tear arthropathy compared to primary osteoarthritis with degenerative cuff tear. [28] In contrast, other authors have found no differences in scapular notch depending on the type of indication. [35] Without a specific comparison among types of indications, some studies have found that there were no differences in scapular notch between patients with or without previous surgery. [38],[39] The results from the abovementioned studies and those from the present investigation are in agreement with results reported by Zumstein et al. [5] The authors found that problems and complications were, in general, twice as frequent in the revision group compared to other indications. They also observed a tendency to increase the problems and complications in the RA and fracture sequelae groups, but this related to the type of approach. [5] The authors were not able to find differences in scapular notch depending on the type of indications, but they did find that instability and infection were higher in the revision compared to the primary RSA group. Zumstein et al. also found that the rate of revision surgery was higher in the revision compared to primary RSA group, but the rate of reoperations was nearly equal. [5] Although Zumstein et al. did not provide P values for the comparisons of reoperations, revisions, problems, and complications depending on the type of prosthesis, there is a clear message which, in addition, is supported by the present investigation: the risk is increased in patients undergoing RSA for a failed anatomic total shoulder arthroplasty or RSA compared to other indications for surgery.
After a literature review and data analysis performed in the present investigation, two main recommendations can be elaborated. First, further research is clearly needed to investigate the influence of the type of prosthesis, type of approach, and indication for surgery altogether in level-I or II-evidence comparative studies on the rate of reoperations, revisions, problems, and complications, as almost all the evidence is based in level-IV case series without comparison of these important factors. Second, there are a huge number of factors that may influence the rate of reoperations, revisions, problems, and complications that are not well controlled in the existing evidence: length of follow-up, [19],[28],[51] surgeons' experience, [41] different rehabilitation protocols (given the multicentric nature of this study), type of glenosphere (eccentric or concentric), [5],[18],[35] location and orientation of the glenosphere and humeral components (glenometaphyseal angle, prosthesis-scapular neck angle, inferiorly placed glenosphere, anteversion/retroversion of the humeral component), [19],[39],[52],[55] vertical pillar of the scapula, [56] degree of fatty infiltration of the teres minor muscle [6],[28],[39] degree of bone stock and glenoid erosion, [26],[28],[30] use of cement, [34] or previous surgery. [7],[9],[36],[38],[39],[42] Therefore, further studies are also needed to assess the influence of these factors.
 Conclusion Conclusion | |  |
Prostheses with lateralized center of rotation had significantly higher glenoid loosening and the need for revision surgery, but significantly lower rate of scapular notching, compared to medialized prostheses. In addition, the risk of reoperations, revisions, problems, and complications after RSA was increased in revision cases compared to other indications for surgery. The value of this analysis is its ability to educate the surgeon and subsequently the patient on the incidence of complications of RSA surgery, which varies significantly according to the patient's surgical indication.
 Acknowledgment Acknowledgment | |  |
The authors would like to thank Sergi Mojal, PhD, for his methodological and statistical contributions.
 References References | |  |
| 1. | Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics 2002;25:129-33.  |
| 2. | Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 1993;16:65-8.  |
| 3. | Grammont PM, Trouilloud P, Laffay J, Deries X. Study of the performance of a new shoulder prosthesis. Rhumatologie 1987;39:407-18.  |
| 4. | Walker M, Brooks J, Willis M, Frankle M. How reverse shoulder arthroplasty works. Clin Orthop Relat Res 2011;469:2440-51.  [ PUBMED] |
| 5. | Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg 2011;20:146-57.  |
| 6. | Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006;15:527-40.  |
| 7. | Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am 2005;87:1697-705.  |
| 8. | Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 2004;86:388-95.  |
| 9. | Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005;87:1476-86.  |
| 10. | Holcomb JO, Cuff D, Petersen SA, Pupello DR, Frankle MA. Revision reverse shoulder arthroplasty for glenoid baseplate failure after primary reverse shoulder arthroplasty. J Shoulder Elbow Surg 2009;18:717-23.  |
| 11. | Khan WS, Longo UG, Ahrens PM, Denaro V, Maffulli N. A systematic review of the reverse shoulder replacement in rotator cuff arthropathy, rotator cuff tears, and rheumatoid arthritis. Sports Med Arthrosc 2011;19:366-79.  |
| 12. | Vanhove B, Beugnies A. Grammont′s reverse shoulder prosthesis for rotator cuff arthropathy. A retrospective study of 32 cases. Acta Orthop Belg 2004;70:219-25.  |
| 13. | Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med 2009;151:264-9, W64.  |
| 14. | Samitier G, Alentorn-Geli E, Torrens C, Wright TW. Reverse total shoulder arthroplasty. Part 1: Systematic review of clinical and functional outcomes. Int J Shoulder Surg 2015;9:1-8.  |
| 15. | Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 2009;18:600-6.  |
| 16. | Boileau P, Moineau G, Roussanne Y, O′Shea K. Bony increased-offset reversed shoulder arthroplasty: Minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res 2011;469:2558-67.  |
| 17. | Cuff D, Pupello D, Virani N, Levy J, Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am 2008;90:1244-51.  |
| 18. | De Biase CF, Delcogliano M, Borroni M, Castagna A. Reverse total shoulder arthroplasty: Radiological and clinical result using an eccentric glenosphere. Musculoskelet Surg 2012;96 Suppl 1:S27-34.  |
| 19. | Falaise V, Levigne C, Favard L, SOFEC. Scapular notching in reverse shoulder arthroplasties: The influence of glenometaphyseal angle. Orthop Traumatol Surg Res 2011;97:S131-7.  |
| 20. | Favard L, Katz D, Colmar M, Benkalfate T, Thomazeau H, Emily S. Total shoulder arthroplasty - Arthroplasty for glenohumeral arthropathies: Results and complications after a minimum follow-up of 8 years according to the type of arthroplasty and etiology. Orthop Traumatol Surg Res 2012;98:S41-7.  |
| 21. | Favard L, Levigne C, Nerot C, Gerber C, De Wilde L, Mole D. Reverse prostheses in arthropathies with cuff tear: Are survivorship and function maintained over time? Clin Orthop Relat Res 2011;469:2469-75.  |
| 22. | Grassi FA, Murena L, Valli F, Alberio R. Six-year experience with the Delta III reverse shoulder prosthesis. J Orthop Surg (Hong Kong) 2009;17:151-6.  |
| 23. | Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am 2006;88:1742-7.  |
| 24. | Holcomb JO, Hebert DJ, Mighell MA, Dunning PE, Pupello DR, Pliner MD, et al. Reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Shoulder Elbow Surg 2010;19:1076-84.  |
| 25. | Kelly JD 2 nd , Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg 2012;21:1516-25.  |
| 26. | Klein SM, Dunning P, Mulieri P, Pupello D, Downes K, Frankle MA. Effects of acquired glenoid bone defects on surgical technique and clinical outcomes in reverse shoulder arthroplasty. J Bone Joint Surg Am 2010;92:1144-54.  |
| 27. | Leung B, Horodyski M, Struk AM, Wright TW. Functional outcome of hemiarthroplasty compared with reverse total shoulder arthroplasty in the treatment of rotator cuff tear arthropathy. J Shoulder Elbow Surg 2012;21:319-23.  |
| 28. | Lévigne C, Garret J, Boileau P, Alami G, Favard L, Walch G. Scapular notching in reverse shoulder arthroplasty: Is it important to avoid it and how? Clin Orthop Relat Res 2011;469:2512-20.  |
| 29. | Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am 2007;89:292-300.  |
| 30. | Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br 2007;89:189-95.  |
| 31. | Martinez AA, Bejarano C, Carbonel I, Iglesias D, Gil-Alvaroba J, Herrera A. The treatment of proximal humerus nonunions in older patients with the reverse shoulder arthroplasty. Injury 2012;43 (Suppl 2):S3-6.  |
| 32. | Martinez AA, Calvo A, Bejarano C, Carbonel I, Herrera A. The use of the Lima reverse shoulder arthroplasty for the treatment of fracture sequelae of the proximal humerus. J Orthop Sci 2012;17:141-7.  |
| 33. | Melis B, Bonnevialle N, Neyton L, Lévigne C, Favard L, Walch G, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: Is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg 2012;21:342-9.  |
| 34. | Melis B, DeFranco M, Lädermann A, Molé D, Favard L, Nérot C, et al. An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br 2011;93:1240-6.  |
| 35. | Mizuno N, Denard PJ, Raiss P, Walch G. The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop 2012;36:1647-53.  |
| 36. | Mulieri P, Dunning P, Klein S, Pupello D, Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am 2010;92:2544-56.  |
| 37. | Sadoghi P, Leithner A, Vavken P, Hölzer A, Hochreiter J, Weber G, et al. Infraglenoidal scapular notching in reverse total shoulder replacement: a prospective series of 60 cases and systematic review of the literature. BMC Musculoskelet Disord 2011;12:101.  |
| 38. | Sadoghi P, Vavken P, Leithner A, Hochreiter J, Weber G, Pietschmann MF, et al. Impact of previous rotator cuff repair on the outcome of reverse shoulder arthroplasty. J Shoulder Elbow Surg 2011;20:1138-46.  |
| 39. | Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am 2007;89:588-600.  |
| 40. | Valenti P, Sauzières P, Katz D, Kalouche I, Kilinc AS. Do less medialized reverse shoulder prostheses increase motion and reduce notching? Clin Orthop Relat Res 2011;469:2550-7.  |
| 41. | Walch G, Bacle G, Lädermann A, Nové-Josserand L, Smithers CJ. Do the indications, results, and complications of reverse shoulder arthroplasty change with surgeon′s experience? J Shoulder Elbow Surg 2012;21:1470-7.  |
| 42. | Wall B, Nové-Josserand L, O′Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85.  |
| 43. | Willis M, Min W, Brooks JP, Mulieri P, Walker M, Pupello D, et al. Proximal humeral malunion treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg 2012;21:507-13.  |
| 44. | Woodruff MJ, Cohen AP, Bradley JG. Arthroplasty of the shoulder in rheumatoid arthritis with rotator cuff dysfunction. Int Orthop 2003;27:7-10.  |
| 45. | Young AA, Smith MM, Bacle G, Moraga C, Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am 2011;93:1915-23.  |
| 46. | Young SW, Everts NM, Ball CM, Astley TM, Poon PC. The SMR reverse shoulder prosthesis in the treatment of cuff-deficient shoulder conditions. J Shoulder Elbow Surg 2009;18:622-6.  |
| 47. | Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg 2012;21:514-22.  |
| 48. | Baulot E, Chabernaud D, Grammont PM. Results of Grammont′s inverted prosthesis in omarthritis associated with major cuff destruction. Apropos of 16 cases. Acta Orthop Belg 1995;61 Suppl 1:112-9.  |
| 49. | De Wilde L, Mombert M, Van Petegem P, Verdonk R. Revision of shoulder replacement with a reversed shoulder prosthesis (Delta III): Report of five cases. Acta Orthop Belg 2001;67:348-53.  |
| 50. | Rittmeister M, Kerschbaumer F. Grammont reverse total shoulder arthroplasty in patients with rheumatoid arthritis and nonreconstructible rotator cuff lesions. J Shoulder Elbow Surg 2001;10:17-22.  |
| 51. | Lévigne C, Boileau P, Favard L, Garaud P, Molé D, Sirveaux F, et al. Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2008;17:925-35.  |
| 52. | Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse shoulder prosthesis: Design, rationale, and biomechanics. J Shoulder Elbow Surg 2005;14:147S-61.  |
| 53. | Harman M, Frankle M, Vasey M, Banks S. Initial glenoid component fixation in "reverse" total shoulder arthroplasty: A biomechanical evaluation. J Shoulder Elbow Surg 2005;14:162S-7.  |
| 54. | Nyffeler RW, Werner CM, Simmen BR, Gerber C. Analysis of a retrieved delta III total shoulder prosthesis. J Bone Joint Surg Br 2004;86:1187-91.  |
| 55. | Nyffeler RW, Werner CM, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg 2005;14:524-8.  |
| 56. | Gutiérrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE 3 rd . Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg 2007;16:S9-12.  |
[Figure 1]
[Table 1], [Table 2]
|
