| |


 |
| Year : 2015 | Volume
: 9
| Issue : 3 | Page : 69-73 |
|
|
|
|
|
ORIGINAL ARTICLE Difference in clinical outcome between total shoulder arthroplasty and reverse shoulder arthroplasty used in hemiarthroplasty revision surgery
Bas Pieter Hartel1, Tjarco D Alta1, Miguel E Sewnath2, Willem J Willems1
1 Department of Orthopaedic Surgery and Traumatology, Onze Lieve Vrouwe Gasthuis, Amsterdam, Netherlands
2 Department of Orthopaedic Surgery and Traumatology, Vlietland Hospital, Schiedam, Netherlands
Correspondence Address:
Bas Pieter Hartel
Wichersstraat 59, 1051 ML, Amsterdam
Netherlands
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.161426
 |
|
|
|
| Date of Web Publication | 24-Jul-2015 |
 Abstract Abstract | | |
Introduction: The increase of shoulder replacements will lead to a higher revision rate of shoulder arthroplasties. The aim of this study is to evaluate the clinical results of revision surgery performed in our hospital, distinguish the differences in clinical outcome according to revision indication and differences between total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA) in hemiarthroplasty (HA) revision surgery.
Materials and Methods: All patients with an indication for revision of HA were retrospectively included. Clinical evaluation consisted of pre- and post-operative constant scores, disability of arm-shoulder-hand-score (DASH), Dutch translation of the simple shoulder test ((D)SST), Oxford shoulder score test (OSS), short form (SF-36) and the complication rate.
Results: From July 1994 to July 2008, 39 patients (40 shoulders) underwent revision arthroplasty. Of 19 patients (19 shoulders) we obtained a complete follow-up. The mean age at revision surgery 69 ± 10 years (range: 46-83) and the mean follow-up 41 ± 31 months (range: 10-113). In 7 cases TSA was used for revision when the cuff was intact, 12 times RSA was performed. The indications for the revision were glenoid erosion (n = 4), humeral component malposition (n = 2), cuff-pathology (n = 12) and infection (n = 1). Postoperative constant score 51.7 ± 11.4 for TSA and 31.1 ± 18.7 for RSA (P = 0.008). The DASH was 48.3 ± 25.1 and 68.7 ± 17.5, respectively (P = 0.09). DSST showed 6 ± 4 and 4 ± 4 (P = 0.414). OSS 41.3 ± 10.1 and 28.1 ± 10.3 (P = 0.017). SF-36 43.3 ± 22.1 and 24.5 ± 12.8 (P = 0.072). Four shoulders (21%) presented four complications.
Conclusions: In this study, revision surgery showed poor to reasonable postoperative results and better clinical outcome for TSA. When a revision after HA was needed, and the soft-tissue component of the shoulder was intact, a TSA proved to be a preferable solution.
Keywords: Clinical, outcome, reverse shoulder arthroplasty, revision surgery, total shoulder arthroplasty
How to cite this article:
Hartel BP, Alta TD, Sewnath ME, Willems WJ. Difference in clinical outcome between total shoulder arthroplasty and reverse shoulder arthroplasty used in hemiarthroplasty revision surgery. Int J Shoulder Surg 2015;9:69-73 |
How to cite this URL:
Hartel BP, Alta TD, Sewnath ME, Willems WJ. Difference in clinical outcome between total shoulder arthroplasty and reverse shoulder arthroplasty used in hemiarthroplasty revision surgery. Int J Shoulder Surg [serial online] 2015 [cited 2016 Sep 20];9:69-73. Available from: http://www.internationalshoulderjournal.org/text.asp?2015/9/3/69/161426 |
 Introduction Introduction | |  |
At present, hemiarthroplasty (HA) is a widely accepted treatment for different pathologies of the shoulder. It significantly improves function and reduces pain. [1],[2] Survival rates for HA are 82% at 10 years and 75% at 20 years respectively. [3] Within the last decade, there has been an increase in the number of shoulder arthroplasties that might lead to an increase in revision procedures. The indications for revision include osseous deficiencies, component wear or a malposition, infection and soft-tissue deficiencies. [4],[5],[6],[7] The outcome of revision may be predicted by the indication. [8],[9] Dines et al. and Sajadi et al. showed that revision for glenoid erosion or component loosening yields better outcomes compared to revision for infection, the pain of undetermined origin or instability/soft-tissue problems. Soft-tissue problems are mainly related to a deficient or absent rotator cuff. Overall, revision shoulder arthroplasty is not as successful as the primary surgery.
The reversed-geometry design, the basis for the reverse shoulder arthroplasty (RSA), is increasingly used for revision surgery instead of the more common total shoulder arthroplasty (TSA). [10],[11] The possible increase in revision surgery and the choice between two different arthroplasties motivated us to evaluate our revision arthroplasties, and compare the outcomes of different indications and prostheses used.
 Materials and methods Materials and methods | |  |
Between July 1994 and July, 2008 40 revision arthroplasties were performed on 39 patients (30 female and 9 male). Of this group, two patients died, and 18 patients were lost to follow-up. Of 19 remaining patients (18 female and one male), all the pre- and post-operative information were present and were included in this study. Thirteen patients were operated on the right side, six on the left side. In all cases, a deltopectoral approach was used. All 19 patients had a HA before revision surgery. The indication for the primary shoulder surgery was osteoarthritis in three, fracture in nine, rheumatoid arthritis in four, secondary osteoarthritis after instability or trauma in one, infection or failure after osteosynthesis in one and avascular humeral head necrosis in one shoulder. The mean age at revision surgery was 69 ± 10 years (range: 46-83). The mean interval between the primary and revision surgery was 25 ± 15 months (range: 2-59). The mean follow-up after revision surgery was 41 ± 31 months (range: 10-113).
The patients were divided into two groups based on indication for revision surgery, consistent with the dichotomized classification by Sajadi et al. and Dines et al. [8],[9] Group 1 (6 patients) consisted of shoulders with the failure of the prosthesis or glenoid erosion (glenoid erosion in four and humeral component malposition in two). Group 2 (13 patients) consisted of shoulders with soft-tissue failure (cuff-pathology/instability in 12 and infection in one). During the revision procedure, 12 HAs were replaced by a revision RSA and seven by a TSA.
Pre- and post-operatively, the Constant score and relative Constant score were retrieved. [12],[13] Postoperatively the disabilities of the arm, shoulder and hand (DASH), the Dutch translation of the simple shoulder test ((D)SST), the Oxford shoulder score (OSS) and the short form (SF-36) were obtained. [14],[15],[16] The SF-36 was divided into two aggregate summary measures: The physical component summary and the mental component summary. This study only used the physical component.
To meet the objective of this study, we compared pre- and post-operative Constant scores of all shoulders, and we compared the two groups previously mentioned.
Furthermore, we compared the postoperative results of the TSA and RSA used in revision surgery. Finally, complications were noted, and the complication rate was calculated.
Statistical analysis
A statistical analysis was performed using SPSS 17.0 (SPSS Inc. Released 2008. SPSS Statistics for Windows, Version 17.0. Chicago, Illinois, USA: SPSS inc.). A paired t-test was used to analyze the difference between the pre- and post-operative constant scores. The independent t-test was used to evaluate the differences between the two indication groups and the RSA and TSA groups. The significance level was set at P > 0.05.
 Results Results | |  |
The purpose of this case series was to evaluate the clinical outcome after revision surgery of HA and the difference between TSA and RSA revision surgery. There was an overall significant increase in shoulder function measured with the absolute constant score (mean improvement 18.9 points, P < 0.001) and the relative constant score (mean improvement 26.9%, P < 0.001) [Table 1].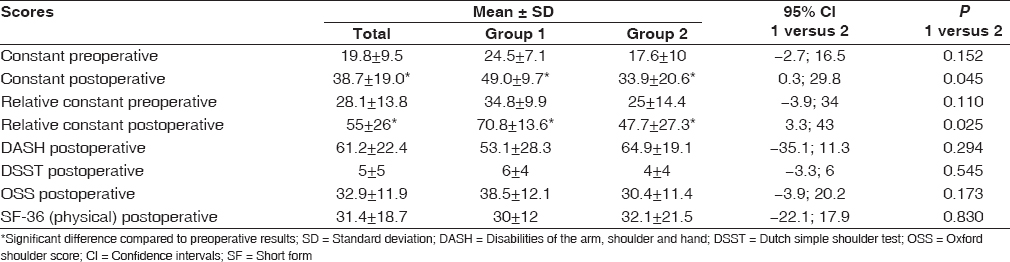 | Table 1: Constant scores, relative Constant score, DASH-scores, DSST, OSS and SF-36 for group 1 and group 2
Click here to view |
Group 1 versus Group 2
Both the constant score and the relative constant score improved significantly in both groups after revision surgery. Group 1 reached a significantly higher postoperative constant score (49.0 ± 9.7) compared to group 2 (33.9 ± 20.6). The same difference was seen in the relative constant score, where the results are 70.8% ± 13.6 and 47.7% ± 27.3 respectively. The other outcomes showed no statistical significant differences between the two groups [Table 1].
Total shoulder arthroplasty versus reverse shoulder arthroplasty
Preoperatively, there was no significant difference in absolute, and relative constant score between the TSA and RSA treated shoulders [Table 2].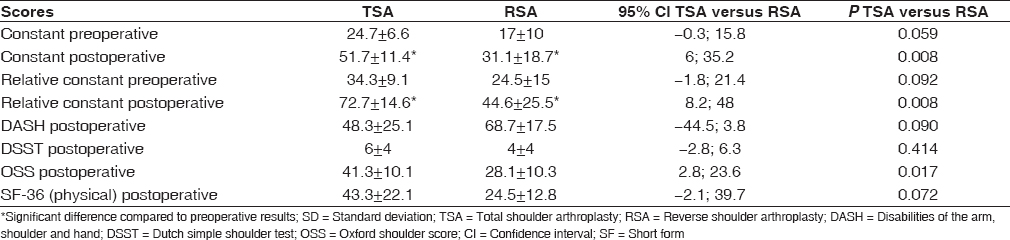 | Table 2: Constant scores, relative constant scores, DASH-scores, DSST, OSS and SF-36 for TSA and RSA
Click here to view |
Postoperatively patients who received a RSA reached a constant score of 31.1 ± 18.7 and a relative constant score of 44.6% ± 25.5. This is significantly less than both scores in patients who received a TSA, 51.7 ± 11.4 and 72.7% ± 14.6 respectively. Moreover, the TSA group achieved a significantly higher OSS score (41.1 ± 9.3 vs. 28.0 ± 9.9) compared with the RSA group [Table 2].
Complications
After revision, 4 out of 19 shoulders (21%) presented with a complication. Two dislocations were seen and two fractures (one postoperative acromion stress fracture and one postoperative humerus fracture). In one dislocation, a liner replacement was needed. The second dislocation could be reduced without surgery. The acromion stress fracture was treated surgically. The humerus fracture was treated with a plate and healed uneventfully. Noteworthy is that three out of the four shoulders with complications received a RSA.
 Discussion Discussion | |  |
At present, HA is a successful surgery with significant improvement in function and pain reduction in most patients. [1],[2] Within the last decade, there has been an increase in the number of shoulder arthroplasties, inevitably leading to a larger number of complications and more revision procedures. Revision surgery performed because of glenoid erosion or component loosening predicts better outcomes than revisions in soft-tissue problems. [9] The introduction of the reversed-geometry design by Grammont et al. has led to an increased use of this prosthetic design in revision shoulder arthroplasty for both soft-tissues and osseous problems. [10],[11]
Along with glenoid erosion in HA, instability is the reason for the majority of the TSA revisions. [17],[18],[19] In the literature, instability was reported by Sajadi et al. (10/35 shoulders), Walker et al. (19/22 shoulders) and Wirth and Rockwood (16/38 shoulders) to be a major indication for revision. [9],[17],[20] Instability usually resulted from rotator cuff deficiencies of various parts of the rotator cuff or malposition of the components. [21] As reported by Dines et al. and Sajadi et al. we defined two groups of patients for different indications. [8],[9] The first group included patients whose shoulder arthroplasties failed due to glenoid erosion or component loosening. The second group included patients with infection, instability or other soft-tissue dysfunction, and pain of undetermined origin. Sajadi et al. noted significantly better results in the first group at forward elevation (106.1° vs. 55.6°), external rotation (ER) (32.8° vs. 11.6°) and the UCLA scores (17.8 vs. 14.1 points). [9] Besides, Dines et al. published significant better results of the first group in the UCLA score (26.1 vs. 12.3 points), L'Insalata score (77.9 vs. 45.3) and satisfaction score (3.45 vs. 1.99). [8] Constant score in our study confirmed these results and was significantly better in the first group.
In the literature, we found results of RSA and TSA in revision surgery, but no clear comparison. Therefore, we were interested in the difference in outcome after revision between the RSA and TSA based on postoperative results. In other studies, the results for TSA outnumbered largely the results for RSA. [7],[8],[9],[20],[21],[22],[23],[24],[25] For instance, Dines et al. reported a total of 39 good to excellent results on the 78 shoulders receiving a revision TSA. [8] The results of 18 revision TSA recorded by Sperling and Cofield showed a decreased pain score (from 4.3 to 2.2 points), an increased in active abduction (from 94° to 124°) and an increased ER (from 32° to 58°). [7] Neer and Kirby reported the results of 36 patients, 30 of whom reported satisfactory pain relief and function for activities of daily living. [26] On the other hand, Walker et al. noted an improvement from one to five points in the simple shoulder test (SST) score and an improvement from 38.5 to 67.5 points in the ASES score in a RSA revision group. [20] Additionally, Levy et al. established results out of 29 patients who received a RSA. [22] The ASES score improved significantly from 22.3 to 52.1 and the SST score improved from 0.9 to 2.6. In the two small series of De Wilde et al. and Delloye et al. (both five shoulders), an improvement in constant score was seen, from 19.4 to 59.9 points and from 32 to 60 points respectively. [27],[28] Finally, Melis et al. conducted a study of 37 patients who underwent a conversion of TSA to RSA and noted an improvement in constant score from 24.3 to 55.2 points at follow-up. [29] In other words, these data are better compared to our results with a constant score of 31.1 points at latest follow-up in the RSA. Although no significant difference was observed, the D(SST) score after revision RSA was lower (four) compared to the score after revision TSA (six). Our remaining results (constant score, DASH, OSS and SF-36) indicate that revision TSA has significantly better results than revision RSA in our study.
Finally, we noted a complication rate of 21% but none of the cases were reoperated. Sperling and Cofield noted a complication rate of 17.6% (3 out of 17), [7] and 12 of the 48 patients (25%) in the series of Antuna et al. required a re-revision. [5] These were studies concerning TSA's. The complication rate seems higher in RSA. [8],[9],[20],[22],[30] Indeed, Boileau et al. described a high reoperation rate (22%) in his study of the Grammont et al. reverse prosthesis. [11],[30] Also, Levy et al. noted eight complications out of 29 shoulders. [22] In his series, three patients had dislocations, two had prosthesis failure, and the last two suffered from an infection and a fracture. In addition, Walker et al. reported an overall complication rate of 22.7% (5 out of 22). [20] Furthermore, De Wilde et al. noted a re-revision rate of 20% and Delloye et al. a rate of 60%. [27],[28] Finally, Melis et al. described an overall 30% complication rate (including glenoid loosening, instability and infection) and a 22% re-revision rate. [29]
 Conclusions Conclusions | |  |
This study suggested that TSA was a reliable and effective option in the revision of HA. When the rotator cuff is intact, an anatomical prosthesis could be considered. In addition, this study suggested that revision for soft-tissue problems provided with inferior results than bone related problems.
 References References | |  |
| 1. | Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am 2005;87:1947-56.  |
| 2. | Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Némoz C, et al. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: Results of a multicenter study. J Shoulder Elbow Surg 2003;12:207-13.  |
| 3. | Sperling JW, Cofield RH, Rowland CM. Minimum fifteen-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elbow Surg 2004;13:604-13.  |
| 4. | Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: Analysis of 2588 shoulders over three decades (1976 to 2008). J Bone Joint Surg Br 2011;93:1513-7.  |
| 5. | Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg 2001;10:217-24.  |
| 6. | Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: Long-term results. J Shoulder Elbow Surg 2004;13:599-603.  |
| 7. | Sperling JW, Cofield RH. Revision total shoulder arthroplasty for the treatment of glenoid arthrosis. J Bone Joint Surg Am 1998;80:860-7.  |
| 8. | Dines JS, Fealy S, Strauss EJ, Allen A, Craig EV, Warren RF, et al. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am 2006;88:1494-500.  |
| 9. | Sajadi KR, Kwon YW, Zuckerman JD. Revision shoulder arthroplasty: An analysis of indications and outcomes. J Shoulder Elbow Surg 2010;19:308-13.  |
| 10. | Gerber C, Pennington SD, Nyffeler RW. Reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2009;17:284-95.  |
| 11. | Grammont P, Trouilloud P, Laffay J, Deries X. Study and realization of a new shoulder prosthesis. (Eture et realisation d′une nouvelle prothese d′epaule). Rhumatologie 1987;39:407-18.  |
| 12. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;214160-4.  |
| 13. | Constant CR, Gerber C, Emery RJ, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg 2008;17:355-61.  |
| 14. | Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996;78:593-600.  |
| 15. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med 1996;29:602-8.  |
| 16. | Kirkley A, Griffin S, Dainty K. Scoring systems for the functional assessment of the shoulder. Arthroscopy 2003;19:1109-20.  |
| 17. | Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am 1996;78:603-16.  |
| 18. | Moeckel BH, Altchek DW, Warren RF, Wickiewicz TL, Dines DM. Instability of the shoulder after arthroplasty. J Bone Joint Surg Am 1993;75:492-7.  |
| 19. | Petersen SA, Hawkins RJ. Revision of failed total shoulder arthroplasty. Orthop Clin North Am 1998;29:519-33.  |
| 20. | Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg 2012;21:514-22.  |
| 21. | Wiesel BB, Williams GR. The reverse prosthesis for failed anatomic shoulder arthroplasty. In: Cofield RH, Sperling JW, editors. Revision and Complex Shoulder Arthroplasty. Philadelphia: Lippincott Williams and Wilkens; 2010. p. 237-49.  |
| 22. | Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am 2007;89:292-300.  |
| 23. | Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 2004;86:388-95.  |
| 24. | Wall B, Nové-Josserand L, O′Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: A review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85.  |
| 25. | Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PA. Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma 2008;22:698-704.  |
| 26. | Neer CS 2 nd , Kirby RM. Revision of humeral head and total shoulder arthroplasties. Clin Orthop Relat Res 1982;170:189-95.  |
| 27. | De Wilde L, Mombert M, Van Petegem P, Verdonk R. Revision of shoulder replacement with a reversed shoulder prosthesis (Delta III): Report of five cases. Acta Orthop Belg 2001;67:348-53.  |
| 28. | Delloye C, Joris D, Colette A, Eudier A, Dubuc JE. Mechanical complications of total shoulder inverted prosthesis. Rev Chir Orthop Reparatrice Appar Mot 2002;88:410-4.  |
| 29. | Melis B, Bonnevialle N, Neyton N, Walch G, Boileau P. Aseptic glenoid loosening or failure in total shoulder arthroplasty: Results of revision with reverse shoulder arthroplasty. In: Walch G, Boileau P, Mole D, Favard L, Levine WN, Sirveaux F, editors. Shoulder Concepts 2010: The Glenoid. Paris: Sauramps Medical; 2010. p. 299-312.  |
| 30. | Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: Design, rationale, and biomechanics. J Shoulder Elbow Surg 2005;14:147S-61.  |
[Table 1], [Table 2]
|
