| |


 |
| Year : 2015 | Volume
: 9
| Issue : 3 | Page : 74-80 |
|
|
|
|
|
ORIGINAL ARTICLE Arthroscopic repair of type II SLAP lesions: Clinical and anatomic follow-up
John N Trantalis1, Stephen Sohmer2, Kristie D More3, Atiba A Nelson3, Ben Wong4, Corinne H Dyke4, Gail M Thornton3, Richard S Boorman3, Ian KY Lo3
1 Department of Orthopaedics, Concord Public Hospital, Concord, NSW 2137, Australia
2 Department of Surgery, Campbell River Hospital, 375 2nd Avenue, Campbell River, BC V9W 3V1, Canada
3 Department of Surgery, Section of Orthopaedic Surgery, McCaig Institute of Bone and Joint Health, University of Calgary, 3330 Hospital Drive NW, Calgary, AB T2N 1N4, Canada
4 Department of Radiology, Foothills Medical Centre, University of Calgary, Calgary, AB T2N 2T9, Canada
Correspondence Address:
Ian KY Lo
Department of Surgery, University of Calgary, 3330 Hospital Drive NW, Calgary, AB T2N 1N4
Canada
 Source of Support: This research was supported by a grant from the Workers’ Compension Board of Alberta., Conflict of Interest: None
DOI: 10.4103/0973-6042.161434
 |
|
|
|
| Date of Web Publication | 24-Jul-2015 |
 Abstract Abstract | | |
Aims: The aim was to evaluate the clinical and anatomic outcome of arthroscopic repair of type II SLAP lesions.
Materials and Methods: The senior author performed isolated repairs of 25 type II SLAP lesions in 25 patients with a mean age of 40.0 ± 12 years. All tears were repaired using standard arthroscopic suture anchor repair to bone. All patients were reviewed using a standardized clinical examination by a blinded, independent observer, and using several shoulder outcome measures. Patients were evaluated by magnetic resonance imaging arthrogram at a minimum of 1-year postoperatively.
Statistical Analysis Used: Two-tailed paired t-test were used to determine significant differences in preoperative and postoperative clinical outcomes scores. In addition, a Fisher's exact test was used.
Results: At a mean follow-up of 54-month, the mean American Shoulder and Elbow Surgeons Shoulder Index (ASES) scores improved from 52.1 preoperatively to 86.1 postoperatively (P < 0.0001) and the Simple Shoulder Test (SST) scores from 7.7 to 10.6 (P < 0.0002). Twenty-two out of the 25 patients (88%) stated that they would have surgery again. Of the 21 patients who had postoperative magnetic resonance imaging arthrographys (MRAs), 9 patients (43%) demonstrated dye tracking between the labrum bone interface suggestive of a recurrent tear and 12 patients (57%) had a completely intact repair. There was no significant difference in ASES, SST, and patient satisfaction scores in patients with recurrent or intact repairs.
Conclusions: Arthroscopic repair of type II SLAP lesions demonstrated improvements in clinical outcomes. However, MRA imaging demonstrated 43% of patients with recurrent tears. MRA results do not necessarily correlate with clinical outcome.
Keywords: Anatomic follow-up, arthroscopic repair, clinical, shoulder, SLAP lesions
How to cite this article:
Trantalis JN, Sohmer S, More KD, Nelson AA, Wong B, Dyke CH, Thornton GM, Boorman RS, Lo IK. Arthroscopic repair of type II SLAP lesions: Clinical and anatomic follow-up. Int J Shoulder Surg 2015;9:74-80 |
 Introduction Introduction | |  |
Lesions of the superior labrum of the shoulder were first described in 1985 by Andrews et al. [1] In 1990, Snyder et al. [2] coined the term SLAP (i.e., superior labrum anterior and posterior) lesions and classified the lesions into four types. A type II SLAP lesion describes a detachment of the superior labrum with resultant instability of the biceps root. Type II SLAP lesions are the most common lesions, representing 55% of all labral tears. [3]
Since its initial description and classification, the volume of literature related to SLAP lesions experienced rapid growth over a relatively short period. While there is a multitude of reports in the literature related to SLAP lesions many controversies remain over its mechanism of injury, examination techniques, diagnostic investigations, arthroscopic diagnosis, and treatment. Notwithstanding these controversies, many authors have reported successful clinical outcomes following arthroscopic repair of type II SLAP lesions. [3],[4],[5],[6],[7],[8],[9],[10],[11],[12],[13],[14]
Despite these reports, there are few studies that specifically investigate the anatomic integrity of the repair. This lack of knowledge precludes correlation of a successful clinical outcome to anatomic healing and limits the utility of postoperative imaging in the painful SLAP repair patient.
The purpose of this study was to evaluate the clinical outcome of patients following type II SLAP repair and to investigate the anatomic outcome using magnetic resonance imaging arthrography (MRA). We hypothesized that patients would have improved outcome following type II SLAP repair and that there would be a correlation between clinical and anatomic outcomes on MRA.
 Materials and methods Materials and methods | |  |
The study was approved by a University Health Research Ethics Board, and all patients consented to participate in the study. Between March 2003 and June 2006, the senior author performed isolated repairs of 25 type II SLAP lesions on a consecutive series of 25 patients (18 male, 7 female) with a mean age of 40 ± 12 years (range: 21-68). The dominant side was affected in 18 of 25 shoulders. Inclusion criteria included age >18 years, type II superior labral anteroposterior (SLAP) lesion confirmed at arthroscopy, and symptomatic for a minimum of 3-month. Exclusion criteria included previous surgery, significant concomitant pathology requiring treatment (e.g., subacromial decompression, distal clavicle excision, rotator cuff repair, biceps tenodesis, biceps tenotomy, Bankart repair, posterior labral repair, osteoarthritis), significant cervical spine pathology (and/or radiculopathy), significant medical issues precluding surgery, secondary gain issues (Workers' Compensation Board claim, litigation), elite athletes, unwillingness to complete study outcomes, and unable to provide informed consent. All patients provided medical history and underwent a physical examination including outcome questionnaires (American Shoulder and Elbow Surgeons Shoulder Index [ASES] and the Simple Shoulder Test [SST]) on initial presentation.
Eighteen out of the 25 patients had a preoperative MRA of which 13 were suspicious for a type II SLAP lesion, and 6 patients had a nonarthrographic magnetic resonance image (MRI) of which 2 were suspicious for a type II SLAP lesion. One patient had a preoperative ultrasound demonstrating no full thickness rotator cuff tear, but the clinical presentation was suspicious for a type II SLAP lesion. All patients had type II SLAP lesions eventually confirmed on arthroscopic evaluation following failure of nonoperative treatment.
A nonoperative treatment was prescribed to each patient at their initial orthopedic consult. The nonoperative treatment program consisted of a supervised physiotherapy program with stretching and strengthening exercises, activity modification, and analgesics. While completing the nonoperative treatment program, patients were seen at 3-month and 6-month. All patients failed the nonoperative treatment program. Failure was defined as patient complaint of persistent pain unaffected by the nonoperative treatment program. A mean duration of symptoms of 30.0 ± 25.8 months prior to surgical intervention.
Surgical technique
The technique of type II SLAP repair has previously been reported. [15] In brief, patients were placed in lateral decubitus position with the arm placed in a pneumatic traction device (Spyder, Tenet Medical, Calgary, Canada). Standard anterior, posterior and anterosuperolateral portals were established. The final diagnosis of a type II SLAP lesion was confirmed at the time of arthroscopy and was based on standardized diagnostic criteria including a bare superior labral footprint, an increased sublabral sulcus with undersurface fraying of the labrum, a displaceable biceps root, a positive peel-back sign, and a positive drive through sign [15],[16] [Figure 1].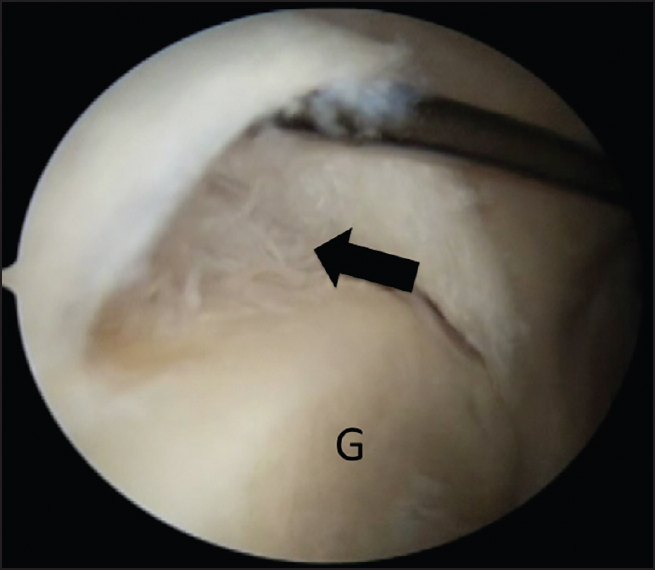 | Figure 1: Arthroscopic view of the right shoulder demonstrating a type II SLAP lesion with an increased sublabral sulcus, a bare sublabral footprint and evidence of fiber failure (arrow). G: Glenoid
Click here to view |
Standard suture anchor based repair was then performed following preparation of the bone bed of the superior glenoid neck. One anchor (3.0 mm Biofastak or BioSuturetak double loaded with #2 Fiberwire, Arthrex, Inc., Naples, FL) was placed underneath the biceps root and sutures were passed anterior and posterior to the biceps tendon. For larger tears extending posteriorly, subsequent anchors were placed through separate percutaneous trans-tendon portals (e.g., Port of Wilmington) into the posterior superior aspect of the glenoid neck. Nine patients had 1 anchor inserted under the biceps anchor, 13 patients had 2 anchors inserted, and 3 patients had 3 anchors inserted. Suture passage was performed using a retrograde (Birdbeak, Arthrex, Inc., Naples, FL) or shuttling technique (Spectrum, Conmed Linvatec, Largo, FL) encircling the labrum in a simple suture fashion [Figure 2]. No patient had a concomitant biceps tenotomy or tenodesis in this study.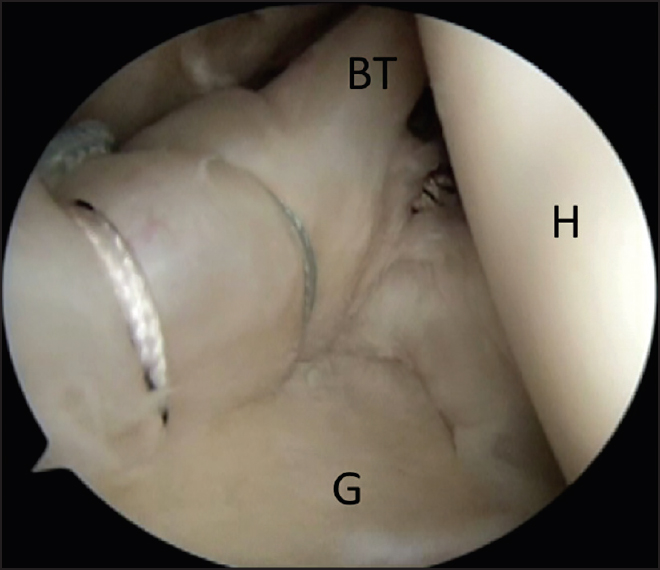 | Figure 2: Arthroscopic view of a right shoulder demonstrating repair of a type II SLAP lesion with one suture anchor placed under the biceps root and a second anchor placed more posteriorly. BT: Biceps tendon, G: Glenoid, H: Humeral head
Click here to view |
Rehabilitation protocol
After completion of the surgery, patients were placed in a supportive sling and commenced a supervised physiotherapy program from day 1 postoperatively. In general, patients were immobilized for 3 weeks but allowed hand, wrist, and elbow range of motion. Passive external rotation was allowed immediately postoperatively as tolerated. At 3 weeks, the sling was discontinued and passive to active range of motion exercises were progressed including overhead elevation and internal rotation. Isotonic strengthening was permitted 6-8 weeks following surgery with progression to return to sport 6-8 months postoperatively.
Clinical evaluation and satisfaction rating
An independent evaluator blinded to the MRA results evaluated patients postoperatively using a standardized protocol including active range of motion and manual muscle testing. Postoperative ASES and SST indices were also completed at their follow-up appointments. Patients were asked to rate their subjective satisfaction on a scale from 0 to 10 (10 being the most satisfied), and whether they would undergo the surgery again.
Magnetic resonance imaging arthrography
In order to determine the anatomic integrity of type II SLAP repairs, 21 out of 25 patients agreed to have their shoulder reimaged at a minimum of 12-month following surgery (mean 25.2-month, range 13-44 months). All patients underwent a standardized MRA protocol and evaluation by two musculoskeletal trained radiologist blinded to the results of clinical outcome. Any disagreement was resolved by consensus. Outcomes were classified according to:
- Recurrent SLAP lesion: Detached superior labrum and dye present between the labrum and superior glenoid at the 12 o'clock position or posteriorly [Figure 3].
- Intact: Minimal to no dye leakage (and/or improvement when compared to the preoperative imaging) under the labrum [Figure 4].
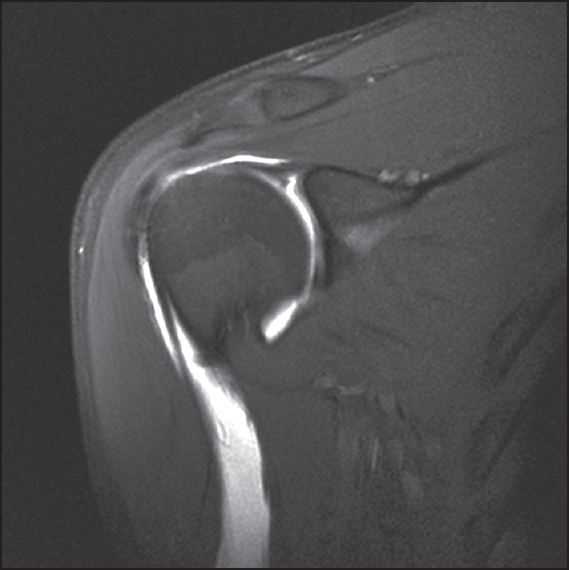 | Figure 3: T1-weighted, fat-suppressed, coronal oblique magnetic resonance imaging arthrography images demonstrating a patient with a recurrent type II SLAP lesions following type II SLAP repair. Note the high signal (gadolinium) present between the superior labrum and glenoid present postoperatively
Click here to view |
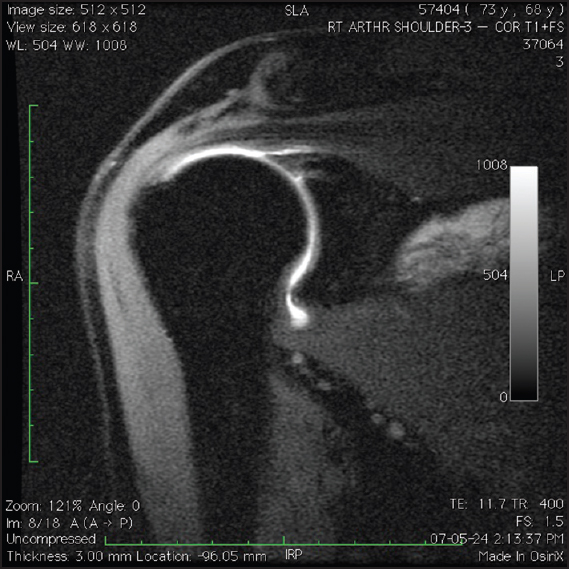 | Figure 4: T1-weighted, fat-suppressed, coronal oblique magnetic resonance imaging arthrography images demonstrating a patient with an intact superior labrum following type II SLAP repair. Note the absence of gadolinium between the superior labrum and glenoid postoperatively
Click here to view |
Statistical analysis
Two-tailed paired t-tests were used to determine significant differences in preoperative and postoperative clinical outcomes scores (ASES and SST), range of motion, and strength. Patients were also categorized according to age (i.e., greater than or less than 40 years old). A P < 0.05 was considered statistically significant.
To analyze whether there was a difference between the MRA appearance (intact versus retorn) of the SLAP repair and ASES, SST or patient satisfaction scores, two-sample t-test with or without Satterthwaite's adjustment for unequal variances were applied. To analyze whether there was an association between the MRA appearance of the SLAP repair and the patients' response to the retrospective question of whether they would have surgery again, a Fisher's exact test was used.
 Results Results | |  |
Twenty-five out of 25 patients were able to present for a follow-up appointment. The mean follow-up was 54-month with a range from 48 to 74 months.
The mean ASES scores improved from 52 ± 18 preoperatively to 86 ± 15 postoperatively (P < 0.0001). The SST scores improved from 7.7 ± 3.0 to 10.6 ± 1.87 (P < 0.0001). The mean subjective patient satisfaction was 8.5 ± 1.5 out of 10. Twenty-two patients (88%) stated that they would have surgery again, and three patients (12%) stated that they would not have surgery again.
There was no statistically significant change in the range of forward flexion (preoperative: 165° ± 11°; postoperative: 172° ± 13°; P = 0.09), or external rotation (preoperative: 56° ± 16°; postoperative: 59° ± 18°; P = 0.34). There were small by significant increases in strength. The forward flexion strength increased from 4.3 ± 0.45 preoperatively to 4.9 ± 0.17 postoperatively (P = 0.000001), external rotation strength increased from 4.3 ± 0.5 preoperatively to 4.9 ± 0.25 postoperatively (P = 0.0001), and internal rotation strength increased from 4.3 ± 0.3 preoperatively to 4.9 ± 0.1 postoperatively (P = 0.00001).
There were 13 patients who were <40 years old and 12 patients who were >40 years old. There was no significant difference between shoulder outcome scores in patients greater than or less than 40 years old [Table 1] (P = 0.39).
Twenty-one out of the 25 patients had a postoperative MRA (1 patient refused, 1 patient had a cardiac stent precluding the use of MRI, 1 patient moved off the continent, 1 patient suffered a separate injury and was unable to attend). Twelve patients had intact type II SLAP repairs on MRA [Figure 4] and nine patients demonstrated leakage of gadolinium insinuating between labum and bone indicating a recurrent (or nonhealing) type II SLAP lesion [Figure 3].
There was no significant difference in ASES, SST, and patient satisfaction scores between patients with recurrent tears or intact repairs [Table 2]. There was no statistically significant association between the MRA appearance of the repair and the patients' response to the question as to whether they would have surgery again (P = 0.74). Of the three patients who would not have surgery again, all had an MRA postoperatively. One had recurrent tear, and two were intact by MRA. The mean age of the patients with recurrent tears (41.2 ± 8.7-year-old) was not significantly different than those with intact repairs (40.9 ± 14.1 years old; P = 0.95).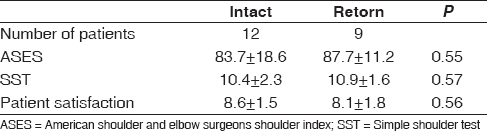 | Table 2: Comparison of intact vs. retorn patients and by outcome measures
Click here to view |
 Discussion Discussion | |  |
The principle result of the study is that arthroscopic repair of type II SLAP lesions demonstrate improvements in clinical outcomes. Although the indications and surgical outcomes following type II SLAP lesion repair continue to evolve, the clinical outcomes in this series of patients were consistent with previous reports [3],[4],[5],[6],[7],[8],[9],[10],[11],[12],[13],[14],[17],[18],[19],[20] with a statistically significant improvement in the both the mean ASES scores and SST scores. Previous studies have suggested that SLAP lesion repair in conjunction with full thickness rotator cuff repair can lead to inferior results. [21],[22],[23] Therefore, we removed any patients with concomitant full thickness rotator cuff tears.
Recently, a number of authors have also questioned the utility of arthroscopic SLAP repair both in the setting of rotator cuff repair and in older patients. In 2009, Boileau et al. [24] reported on the treatment of type II SLAP lesions. He noted superior results in older patients who underwent biceps tenodesis as opposed to arthroscopic SLAP repair. Similarly, Denard et al. [25] reported inferior results in patients over the age of 40 years old following arthroscopic SLAP repair and recommended biceps tenodesis in the older patient.
In the current study, we could not detect a significant difference in clinical outcome in patients greater than or less than 40 years old. Older patients had similarly good outcomes following arthroscopic type II SLAP lesions repair when compared to patients under the age of 40. While this may be related to the relatively low number of patients in this study, other authors have also reported excellent results when performing SLAP repair in older patients. [26],[27],[28] Furthermore, there was no statistical association between healing of the type II SLAP repair and age suggesting that older patients may have a similar healing potential. This is in contrast to reports of repair integrity following rotator cuff repair which a demonstrated an inverse association with increasing age. [29],[30],[31]
The authors believe that with careful clinical indications, good outcomes can be achieved in patients over the age of 40 years old. However, the authors routinely perform alternative procedures in patients with concomitant full thickness rotator cuff tears and patients involved in litigation or workers compensation claims. In the senior author's experience, SLAP repair in these patients has an increased risk of poor outcomes including adhesive capsulitis and on-going pain. Therefore, SLAP repair is generally avoided in these complex populations to avoid these complications. In the senior author's experience, these patients commonly present with inconsistent histories and physical examinations may be better served with biceps tenodesis or debridement. [21],[22],[23],[25]
The authors believe that in patients over the age of 40 with a clear history of injury during overhead athletics, and in particular symptoms predominantly isolated to overhead athletics, arthroscopic SLAP repair may be considered. It should be noted that the 25 patients evaluated in this study were collected over a greater than 3-year period. Since the senior author performs approximately 400-450 shoulder arthroscopies per year, this is a rate of only ~2% of shoulder arthroscopies. This is consistent with reports by Snyder et al. [2],[3] who reported a rate of 3.3-4.7% of surgical cases. In contrast, Weber et al. [32] reported an incidence of SLAP repairs of 9.4% in reported cases to the American Board Of Orthopedic Surgery Part II candidates. These cases also had 4.4% complication rate, with 73.7% of patients complaining of persistent pain and only 13.1% of patients rating their shoulder as normal. These results highlight the importance of careful clinical evaluation and appropriate indications for arthroscopic SLAP repair.
While no clinical evaluation is infallible, in the senior author's experience the patient's history (e.g., athletic profile, prodromal symptoms, difficulty with overhead athletics, dead arm syndrome) is the most important clinical diagnostic tool, followed by supportive physical examination tests. The senior author commonly utilizes the O'Brien's sign and the relocation sign (for pain) as supportive physical examination tests. [4],[15]
The authors believe that strict patient indications, the avoidance of SLAP repair in patients with an "anatomic" SLAP lesion; but without corresponding history, and avoidance of concomitant SLAP repair during the treatment of other significant pathology (e.g., rotator cuff tear), may have contributed to the relatively good outcomes in this review, even in patients over the age of 40.
This study also aimed to specifically investigate the appearance of arthroscopically repaired type II SLAP lesions on MRA. Since MRA has been extensively studied as a tool for investigating the presence of superior labral lesions in primary shoulders, we chose this modality. Bencardino et al. [33] reported that in the diagnosis of a type II SLAP lesion, MRA had a sensitivity of 89%, specificity of 91%, and accuracy of 90% in their study which used arthroscopy as the gold standard. Other studies have reported similar results. [34],[35],[36] However, Vangsness et al. [37] and Reuss et al., [38] both reported lower sensitivity and specificity in the MRA diagnosis of SLAP lesions, and correlated this with the experience of the radiologist. For this reason, in our clinical series, all MRAs were performed and reported by a two radiologists who both specialized in the interpretation of musculoskeletal imaging, and were also blinded to the clinical outcomes.
To our knowledge, MRA has not previously been reported for anatomic imaging following type II SLAP repair. Furthermore, few studies have evaluated the postoperative integrity of type II SLAP repairs using any imaging modality. Yoneda et al. [14] reported on 10 patients after operative repair of superior labral tears associated with spinoglenoid cysts. Follow-up MRIs (without gadolinium enhancement) were performed on 8 patients at a mean of 6-month postoperatively (range: 3-14 months) and demonstrated complete resolution of the cyst and healing of the superior labrum. However, the utility of nonenhanced MRI for the detection of superior labral tears has recently been questioned. [39],[40]
Computed tomography arthrography (CTA) has recently been introduced as a potential modality for imaging of the superior labrum. [41],[42],[43] Oh et al. compared CTA and MRA for the detection of bony lesions (Hill-Sachs lesions), labral lesions (Bankart, SLAP) and rotator cuff tears (full thickness or partial thickness). [41] Although, CTA was as accurate as MRA for the detection of labral tears and full thickness rotator cuff tears, CTA was not as accurate as MRA for the detection of partial-thickness rotator cuff tears.
Oh et al. recently utilized CTA in the detection of healing following arthroscopic type II SLAP repair. [43] In their study of 58 SLAP lesions, 100% demonstrated anatomic healing of the superior labrum to the glenoid. While these results are encouraging both with respect to the utility of the modality and rate of healing, the acceptance of CTA in North America is not as widely acknowledged.
In the current study, we performed MRA on 21 of 25 patients following arthroscopic SLAP repair. All MRA were evaluated by two musculoskeletal-trained radiologists, and any disagreement was resolved by consensus. Despite the overall excellent results, 9 of 21 patients demonstrated some dye leakage between the interface of glenoid and labrum. This is in direct contrast to the study by Oh et al. [43] which demonstrated a 100% healing rate.
Why the anatomic results are so different is unclear. This may be related to differences in patient poluations, surgical technique (e.g., knotless versus knotted; amount of bone bed debridement), and rehabilitation protocols (e.g., period of immobilization). Importantly, however, it may also be related to differences in diagnostic imaging studies (MRA vs. CTA). It should be noted that the accuracy of either study in the postoperative situation is unknown since arthroscopic correlation was not routinely performed.
The results of MRA in this study did not correlate with clinical outcome. Patients with recurrent SLAP lesions overall had comparable results to those with intact repairs questioning the impact of persistent SLAP defects. This is similar to postoperative imaging following rotator repair where persistent rotator cuff defects may be relatively asymptomatic. [44],[45],[46] Furthermore, this is consistent to a recent report by Oh et al. [42] who evaluated the results 61 patients following concomitant rotator cuff and SLAP repair. Using CTA, they demonstrated that unhealed SLAP lesions did not negatively affect the outcome, and there were no significant differences between patients with healed or recurrent SLAP tears.
Importantly, the current results also question the utility of MRA in the investigation of the failed SLAP repair patient. A number of authors have recently published poor results following SLAP repair and the results of revision surgery. [17],[47],[48] While MRA may be utilized in the diagnostic workup of a failed SLAP repair, it should not be the sole investigative tool. Careful clinical workup is obligatory. Furthermore, due to the high incidence of patients with persistent dye leakage between the labrum and glenoid postoperatively, an imaging report of a "recurrent SLAP lesion" should not prematurely terminate methodical clinical investigation. In our study, not only was there a poor correlation between MRA appearance and outcome, but of the three patients with unsatisfactory results two had an intact repair. This further highlights the complexity of postoperative evaluation of the failed SLAP patient where multiple diagnoses may lead to a poor outcome. [47],[49]
Limitations
The weaknesses of this study are that it is a nonrandomized, retrospective study, with a relatively small sample size. Another limitation is that all research activity related to this study was closed in 2012; therefore, further examination of data beyond the initial research question could not be completed. Furthermore, the results of MRA were not confirmed by routine second-look arthroscopy and therefore the accuracy of this imaging modality in the postoperative evaluation is unclear. Despite this, the results in our study are unique in the examination of clinical outcome and MRA outcome following arthroscopic SLAP repair.
 Conclusion Conclusion | |  |
Arthroscopic repair of type II SLAP lesions can lead to significant improvement in clinical outcomes. MRAs performed postoperatively demonstrated an intact repair in 57% of cases, and recurrent tears in 43%. However, there was no significant difference in clinical outcome in patients with intact or recurrent tears.
 References References | |  |
| 1. | Andrews JR, Carson WG Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med 1985;13:337-41.  |
| 2. | Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy 1990;6:274-9.  |
| 3. | Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg 1995;4:243-8.  |
| 4. | Burkhart SS, Morgan C. SLAP lesions in the overhead athlete. Orthop Clin North Am 2001;32:431-41, viii.  |
| 5. | Cohen DB, Coleman S, Drakos MC, Allen AA, O′Brien SJ, Altchek DW, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy 2006;22:136-42.  |
| 6. | Field LD, Savoie FH 3 rd . Arthroscopic suture repair of superior labral detachment lesions of the shoulder. Am J Sports Med 1993;21:783-90.  |
| 7. | Kartus J, Kartus C, Brownlow H, Burrow G, Perko M. Repair of type-2 SLAP lesions using corkscrew anchors. A preliminary report of the clinical results. Knee Surg Sports Traumatol Arthrosc 2004;12:229-34.  |
| 8. | McFarland EG, Park HB, Chronopolous E, Yokota A, Kim TK. Results of repair of SLAP lesion. Orthopade 2003;32:637-41.  |
| 9. | Ozbaydar MU, Tekin C, Kocabas R, Yalaman O. Arthroscopic treatment of type 2 superior labrum anterior posterior lesions. Acta Orthop Traumatol Turc 2006;40:349-55.  |
| 10. | Paxinos A, Walton J, Rütten S, Müller M, Murrell GA. Arthroscopic stabilization of superior labral (SLAP) tears with biodegradable tack: Outcomes to 2 years. Arthroscopy 2006;22:627-34.  |
| 11. | Samani JE, Marston SB, Buss DD. Arthroscopic stabilization of type II SLAP lesions using an absorbable tack. Arthroscopy 2001;17:19-24.  |
| 12. | Segmüller HE, Hayes MG, Saies AD. Arthroscopic repair of glenolabral injuries with an absorbable fixation device. J Shoulder Elbow Surg 1997;6:383-92.  |
| 13. | Warner JJ, Kann S, Marks P. Arthroscopic repair of combined Bankart and superior labral detachment anterior and posterior lesions: Technique and preliminary results. Arthroscopy 1994;10:383-91.  |
| 14. | Yoneda M, Hirooka A, Saito S, Yamamoto T, Ochi T, Shino K. Arthroscopic stapling for detached superior glenoid labrum. J Bone Joint Surg Br 1991;73:746-50.  |
| 15. | Burkhart SS, Lo IK, Brady PC. Burkhart′s View of the Shoulder: The Cowboy′s Guide to Advanced Shoulder Arthroscopy . Philadelphia: Lippincott Williams & Williams; 2006.  |
| 16. | Mileski RA, Snyder SJ. Superior labral lesions in the shoulder: Pathoanatomy and surgical management. J Am Acad Orthop Surg 1998;6:121-31.  |
| 17. | Funk L, Snow M. SLAP tears of the glenoid labrum in contact athletes. Clin J Sport Med 2007;17:1-4.  |
| 18. | Neuman BJ, Boisvert CB, Reiter B, Lawson K, Ciccotti MG, Cohen SB. Results of arthroscopic repair of type II superior labral anterior posterior lesions in overhead athletes: Assessment of return to preinjury playing level and satisfaction. Am J Sports Med 2011;39:1883-8.  |
| 19. | Rhee YG, Lee DH, Lim CT. Unstable isolated SLAP lesion: Clinical presentation and outcome of arthroscopic fixation. Arthroscopy 2005;21:1099.  |
| 20. | Seroyer S, Tejwani SG, Bradley JP. Arthroscopic capsulolabral reconstruction of the type VIII superior labrum anterior posterior lesion: Mean 2-year follow-up on 13 shoulders. Am J Sports Med 2007;35:1477-83.  |
| 21. | Abbot AE, Li X, Busconi BD. Arthroscopic treatment of concomitant superior labral anterior posterior (SLAP) lesions and rotator cuff tears in patients over the age of 45 years. Am J Sports Med 2009;37:1358-62.  |
| 22. | Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. No advantages in repairing a type II superior labrum anterior and posterior (SLAP) lesion when associated with rotator cuff repair in patients over age 50: A randomized controlled trial. Am J Sports Med 2008;36:247-53.  |
| 23. | Kim SJ, Lee IS, Kim SH, Woo CM, Chun YM. Arthroscopic repair of concomitant type II SLAP lesions in large to massive rotator cuff tears: Comparison with biceps tenotomy. Am J Sports Med 2012;40:2786-93.  |
| 24. | Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: Biceps tenodesis as an alternative to reinsertion. Am J Sports Med 2009;37:929-36.  |
| 25. | Denard PJ, Jiwani AZ, Lädermann A, Burkhart SS. Long-term outcome of arthroscopic massive rotator cuff repair: The importance of double-row fixation. Arthroscopy 2012;28:909-15.  |
| 26. | Alpert JM, Wuerz TH, O′Donnell TF, Carroll KM, Brucker NN, Gill TJ. The effect of age on the outcomes of arthroscopic repair of type II superior labral anterior and posterior lesions. Am J Sports Med 2010;38:2299-303.  |
| 27. | Kanatli U, Ozturk BY, Bolukbasi S. Arthroscopic repair of type II superior labrum anterior posterior (SLAP) lesions in patients over the age of 45 years: A prospective study. Arch Orthop Trauma Surg 2011;131:1107-13.  |
| 28. | Schrøder CP, Skare O, Gjengedal E, Uppheim G, Reikerås O, Brox JI. Long-term results after SLAP repair: A 5-year follow-up study of 107 patients with comparison of patients aged over and under 40 years. Arthroscopy 2012;28:1601-7.  |
| 29. | Oh JH, Kim SH, Kang JY, Oh CH, Gong HS. Effect of age on functional and structural outcome after rotator cuff repair. Am J Sports Med 2010;38:672-8.  |
| 30. | Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy 2009;25:30-9.  |
| 31. | Cho NS, Lee BG, Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: Is the repair integrity actually maintained? Am J Sports Med 2011;39:2108-16.  |
| 32. | Weber SC, Martin DF, Seiler JG 3 rd , Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: Incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med 2012;40:1538-43.  |
| 33. | Bencardino JT, Beltran J, Rosenberg ZS, Rokito A, Schmahmann S, Mota J, et al. Superior labrum anterior-posterior lesions: Diagnosis with MR arthrography of the shoulder. Radiology 2000;214:267-71.  |
| 34. | Applegate GR, Hewitt M, Snyder SJ, Watson E, Kwak S, Resnick D. Chronic labral tears: Value of magnetic resonance arthrography in evaluating the glenoid labrum and labral-bicipital complex. Arthroscopy 2004;20:959-63.  |
| 35. | Jee WH, McCauley TR, Katz LD, Matheny JM, Ruwe PA, Daigneault JP. Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: Reliability and accuracy of MR arthrography for diagnosis. Radiology 2001;218:127-32.  |
| 36. | Waldt S, Burkart A, Lange P, Imhoff AB, Rummeny EJ, Woertler K. Diagnostic performance of MR arthrography in the assessment of superior labral anteroposterior lesions of the shoulder. AJR Am J Roentgenol 2004;182:1271-8.  |
| 37. | Vangsness CT Jr, Jorgenson SS, Watson T, Johnson DL. The origin of the long head of the biceps from the scapula and glenoid labrum. An anatomical study of 100 shoulders. J Bone Joint Surg Br 1994;76:951-4.  |
| 38. | Reuss BL, Schwartzberg R, Zlatkin MB, Cooperman A, Dixon JR. Magnetic resonance imaging accuracy for the diagnosis of superior labrum anterior-posterior lesions in the community setting: Eighty-three arthroscopically confirmed cases. J Shoulder Elbow Surg 2006;15:580-5.  |
| 39. | Halma JJ, Eshuis R, Krebbers YM, Weits T, de Gast A. Interdisciplinary inter-observer agreement and accuracy of MR imaging of the shoulder with arthroscopic correlation. Arch Orthop Trauma Surg 2012;132:311-20.  |
| 40. | Phillips JC, Cook C, Beaty S, Kissenberth MJ, Siffri P, Hawkins RJ. Validity of noncontrast magnetic resonance imaging in diagnosing superior labrum anterior-posterior tears. J Shoulder Elbow Surg 2013;22:3-8.  |
| 41. | Oh JH, Kim JY, Choi JA, Kim WS. Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: Comparison with magnetic resonance imaging with arthroscopic correlation. J Shoulder Elbow Surg 2010;19:14-20.  |
| 42. | Oh JH, Kim SH, Kwak SH, Oh CH, Gong HS. Results of concomitant rotator cuff and SLAP repair are not affected by unhealed SLAP lesion. J Shoulder Elbow Surg 2011;20:138-45.  |
| 43. | Oh JH, Kim SH, Lee HK, Jo KH, Bae KJ. Trans-rotator cuff portal is safe for arthroscopic superior labral anterior and posterior lesion repair: Clinical and radiological analysis of 58 SLAP lesions. Am J Sports Med 2008;36:1913-21.  |
| 44. | Dodson CC, Kitay A, Verma NN, Adler RS, Nguyen J, Cordasco FA, et al. The long-term outcome of recurrent defects after rotator cuff repair. Am J Sports Med 2010;38:35-9.  |
| 45. | Spielmann AL, Forster BB, Kokan P, Hawkins RH, Janzen DL. Shoulder after rotator cuff repair: MR imaging findings in asymptomatic individuals - initial experience. Radiology 1999;213:705-8.  |
| 46. | Zanetti M, Jost B, Hodler J, Gerber C. MR imaging after rotator cuff repair: Full-thickness defects and bursitis-like subacromial abnormalities in asymptomatic subjects. Skeletal Radiol 2000;29:314-9.  |
| 47. | Katz LM, Hsu S, Miller SL, Richmond JC, Khetia E, Kohli N, et al. Poor outcomes after SLAP repair: Descriptive analysis and prognosis. Arthroscopy 2009;25:849-55.  |
| 48. | Park S, Glousman RE. Outcomes of revision arthroscopic type II superior labral anterior posterior repairs. Am J Sports Med 2011;39:1290-4.  |
| 49. | Weber SC. Surgical management of the failed SLAP repair. Sports Med Arthrosc 2010;18:162-6.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
[Table 1], [Table 2]
|
