| |


 |
| Year : 2015 | Volume
: 9
| Issue : 4 | Page : 121-127 |
|
|
|
|
|
ORIGINAL ARTICLE Catastrophic failure of a low profile metal-backed glenoid component after total shoulder arthroplasty
Carley B Vuillermin1, Mark E Trump2, Shane A Barwood3, Gregory A Hoy3
1 Melbourne Orthopaedic Group, Windsor 3181, Victoria, Australia
2 Department of Orthopedic Surgery, Los Angeles County and University of Southern California Medical Center, Los Angeles, CA 90033, USA
3 Melbourne Orthopaedic Group, Windsor 3181, Victoria; Monash University Department of Surgery, Melbourne, Australia
Correspondence Address:
Gregory A Hoy
Melbourne Orthopaedic Group, 33 The Avenue, Windsor 3181, Victoria
Australia
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/0973-6042.167952
 |
|
|
|
| Date of Web Publication | 22-Oct-2015 |
 Abstract Abstract | | |
Context: The longevity of the glenoid component in total shoulder arthroplasty (TSA) continues to be problematic. All polyethylene glenoid components have been most widely used, but loosening rates with time and the need for revision has resulted in high-profile metal-backed components with the potential for a more stable prosthesis bone interface and liner exchange. High revision rates in the high profile metal backed designs led us to evaluate a low profile metal backed component.
Aims: To examine the rate and mode of failure of a TSA in a single surgeon consecutive series that has been identified by the Australian National Joint Replacement Registry to have a higher than anticipated rate of revision.
Materials and Methods: This is a single surgeon retrospective consecutive series of 51 arthroplasties undertaken in 50 patients (18 males and 32 females) with an average age of 70.4 ears (range 51-90) and mean follow-up of 5.5 years (range 3.7-8.1).
Results: We observed a very high (29%) rate of revision of the metal-backed glenoid components in this series. The primary mode of failure was glenoid baseplate nonintegration which with a well-fixed central cage screw led to bone resorption and implant breakage or disassembly.
Conclusion: Analysis of the mode of failure of implants identified by robust registries is essential for the development of new prostheses and the pursuit of prosthesis longevity. This low profile metal backed prosthesis has been withdrawn, but without a published mechanism of failure. We feel that any prosthesis withdrawal should be accompanied by appropriate published mechanisms to prevent future component design errors based on similar design problems.
Keywords: Glenoid component, low profile metal-backed glenoid, prosthesis design, prosthesis failure, shoulder arthroplasty
How to cite this article:
Vuillermin CB, Trump ME, Barwood SA, Hoy GA. Catastrophic failure of a low profile metal-backed glenoid component after total shoulder arthroplasty. Int J Shoulder Surg 2015;9:121-7 |
 Introduction Introduction | |  |
Total shoulder arthroplasty (TSA) has been shown to provide patients with pain relief and improved function. Problems include long-term survivorship of the prosthesis and the need for revision. Glenoid component loosening or nonintegration is a common primary cause of both loss of function and the need for revision. [1],[2]
The most widely used fixation method is the all polyethylene cemented component using either a keeled component or a pegged base. [3],[4],[5],[6],[7],[8] The incidence of postimplantation radiolucent lines varies from 10% to 85%. [7],[9],[10] Loosening and in particular, progressive lucencies have been associated with higher clinical failure rates and the need for revision. [3],[11]
Several previous metal-backed prostheses have been introduced without achieving the success of cemented components, [5],[7],[12],[13],[14],[15] although there are also limited examples of metal backed prostheses with better medium term survivorship, [16] this has not been widely achieved. Metal backed glenoid components are designed to facilitate biological on or in-growth to the surface leading to a more stable prosthesis to bone interface over the long term. Modular metal-backed components offer the advantage of allowing liner exchange with polyethylene wear. Modularity however potentially increases the thickness of the components and also introduces more points of failure.
A modular metal-backed glenoid component TSA (Arthrex, Naples, FL, USA) represented a third generation shoulder prosthesis and offered several design features with the potential to lead to a decrease in the complications and an improved overall outcome for patients. A thin titanium base plate minimized the total thickness of the component. A large central nonlocking cage screw provided primary stability, with the backside of the base plate for bone on-growth and secondary stability. A modular polyethylene liner could be exchanged without revision of the entire component. The early results reported by the design team were favorable with 300 prostheses implanted, including 197 patients with >12 months follow-up of which 115 were TSA. [17] Two of the TSA patients were reported to require revision, one for polyethylene inlay displacement, and one for subscapularis failure.
We are unaware of any nondesign team associated previous study reporting the outcome of this prosthesis. The Australian National Joint Replacement Registry (NJRR) reported a high rate of revision for this prosthesis. [18] A retrospective consecutive series cohort study was undertaken. This study was aimed to determine the rate of revision as well as examine the potential modes of failure for this low profile metal backed implant compared to standard high profile metal backed glenoids when performed by a nondesign but fellowship trained surgeon.
 Materials and Methods Materials and Methods | |  |
Institutional Review Board approval was granted for this study. A consecutive series of anatomic total shoulder replacements (TSRs) performed by a single surgeon were studied between March 2004 and October 2008. The total arthroplasty load during this period in this practice was 185, including 27 revision replacements. All patients presenting for anatomic TSA during the study period were considered for this implant, exclusions were for reverse arthroplasty candidates, type B2 glenoids, severe osteoporosis, or inadequate bone stock assessed on plain radiographs or computed tomography. Patients who were primarily deemed to be more suited to a cemented component were excluded from consideration of use of the metal-backed glenoid and this prosthesis. Patients were included in the study on an intention to treat basis, as all patients had been selected as potentially suitable for a metal back component.
Surgical technique
A deltopectoral approach was used for all replacement operations.
The glenoid implant was produced from titanium with a sintered surface for bone apposition, with a nonlocking central cage screw similar to that used in a short-stemmed humeral component from the same manufacturer. The glenoid insert was UHMWPE and was impacted into the glenoid metal back "tray" using a purpose built impactor. The humeral component was also sintered with variable geometry axis and angulation of the humeral head component.
The senior author was trained in the surgical technique by the design team, as previously published. [17] Components were implanted according to this technique, using standard instrumentation and jigging provided by the manufacturer. A unique feature of this system was an oscillating reamer used for the preparation of the glenoid surface prior to implantation, used to ream to the subchondral bone plate but not correcting significant glenoid version defects.
A cemented polyethylene component was available if bone quality was not felt to be suitable for metal backed implantation including massive cysts or osteoporosis. An uncemented univers three-dimensional humeral stem with a "variable trunnion to optimize neck-shaft angle and proximal humeral match with minimization of cuff impingement" was used in all patients. No significant rotator cuff tears were noted or repaired.
Patients followed the senior author's standard postoperative protocol. Range of movement restoration over the initial 8-week period, followed by strengthening.
Chart review was performed detailing information on the implants used and intraoperative findings.
Patient demographics and follow-up
All patients were followed up with either routine annual clinic review, but any that failed to attend were contacted for telephone review.
Fifty-one replacements were performed in 50 patients (18 males and 32 females). A single patient had bilateral staged replacements. Patients at the time of review were an average of 65.5 months postindex surgery (range 44-97 months). Average age at the time of surgery was 70.4 years (range 51-90). Four patients were deceased by the time of final follow-up. Fifteen patients were contacted by telephone as it had been 2 years or more since their last office review. Fourteen of these patients were all in the nonrevised cohort.
The primary outcome assessed was any revision surgery to the replaced shoulder. Revision was offered on clinical grounds alone, being either symptomatic loosening or prosthesis failure (component fracture, polyethylene wear or dislocation). Radiographic loosening alone was not sufficient. For patients who had undergone revision surgery, the medical record was reviewed, and the findings assessed with respect to the indication for revision and the mode of failure.
Statistical analysis
Statistical analysis was performed using a professional consultant. The association between individual variables was investigated using binomial generalized linear models. Kaplan-Meir survival analyses were undertaken with months at risk of revision as the time variable and censoring of patients who died. Statistical analyses were undertaken in SPSS 20 (IBM, USA) and Stata 12 (Statacorp, TX, USA). A P = 0.05 was determined to be a statistically significant result.
 Results Results | |  |
All surviving patients were located for follow-up. All patients had a primary diagnosis of osteoarthritis.
Forty-eight replacements were as primary procedures, and three were revisions from a humeral resurfacing component (Biomet, Warsaw, IN, USA) to a stemmed TSR. Thirty-one right and 20 left replacements were performed. The glenoid component implantation was the primary glenoid procedure in all cases.
Primary surgery
All patients had an uncemented humeral stem. Forty-five patients had a metal-backed glenoid component [Figure 1]. Four patients had a keeled glenoid component due to concerns regarding bone quality, and two had no glenoid implanted. Three of the four keeled glenoid components were implanted in the final six patients of the series as concerns regarding the secondary stability of the glenoid component surfaced.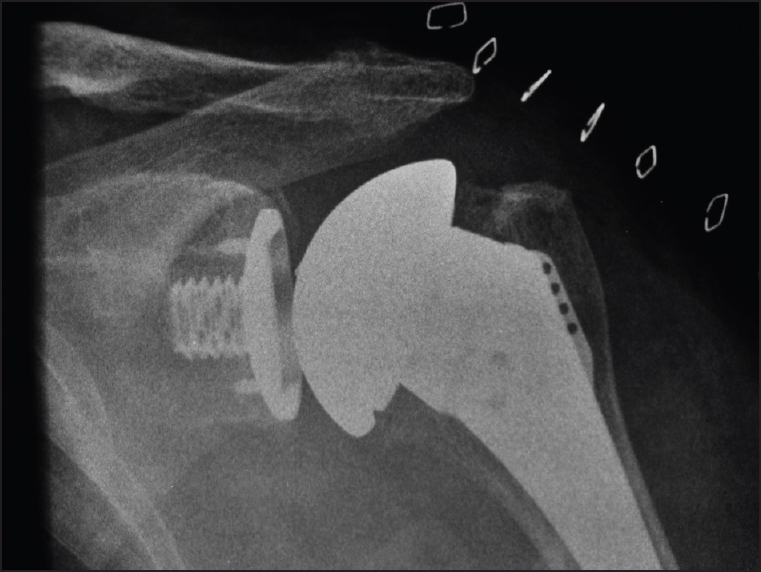 | Figure 1: Anterior-posterior postoperative radiograph of univers total shoulder replacements with a metal-backed glenoid component
Click here to view |
During surgery, all patients had the excellent primary stability of the metal-backed glenoid component. The large central cage screw was nonlocking, so that it gained excellent compression of the baseplate onto the reamed glenoid surface, but had no method to maintain compression with any later bony resorption.
Complications and revisions
None of the patients who had an all polyethylene glenoid component or hemiarthroplasty component implanted underwent revision surgery.
Seventeen of the 45 patients with metal-backed glenoid components required revision surgery. Thirteen of these were for complications associated with loosening of the glenoid component with a revision rate of 29%. All of the patients who had previously had a humeral resurfacing component prior to TSR required revision of their metal-backed glenoid component. There did not appear to be an association with a learning curve as there were 10 revisions in the first 23 glenoids implanted and seven revisions in the subsequent 22.
Three revisions were for soft-tissue complications with one subscapularis tear and two supraspinatus tears. One of these patients also had polyethylene delamination with a well-fixed glenoid base plate, necessitating a liner exchange at revision. A single patient had a peri-prosthetic humeral shaft fracture distal to the stem without compromise of the prosthesis and underwent open reduction and internal fixation.
There were no revisions for humeral component loosening. One of the revised patients had a subsequent fracture of the humeral stem trunnion, which was not exchanged at the initial revision, and this would no longer be standard practice.
The survival curve to revision is shown in [Figure 2]. The overall rate of revision was 9.38 revisions per 100 component years at risk (95% confidence interval, 5.65-14.71). There was no significant association with age, gender, or glenoid size and the rate of revision [Figure 3], although there were relatively low numbers of patients in each cohort.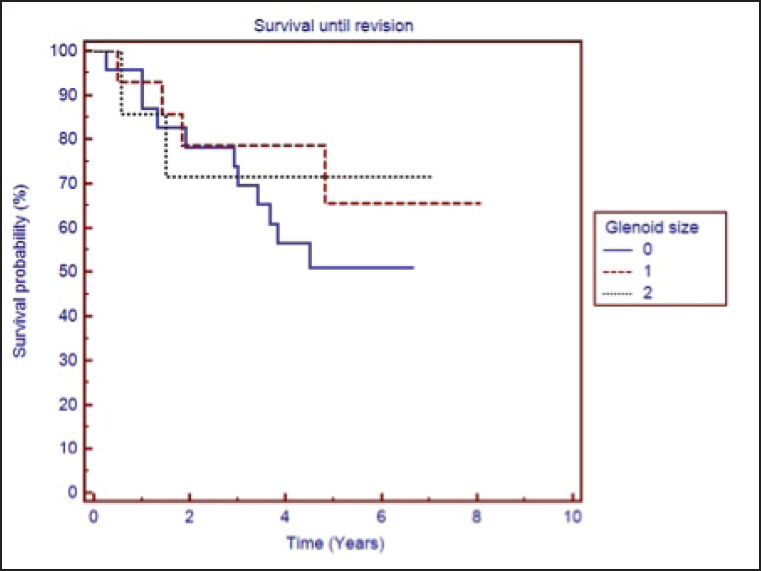 | Figure 3: Glenoid component survival according to size of implanted component
Click here to view |
Metal backed revisions
There were 13 revisions for complications associated with the metal-backed glenoid component. Early signs of loosening of the glenoid with resorption of the glenoid bone behind the baseplate were seen on serial radiographs [Figure 4].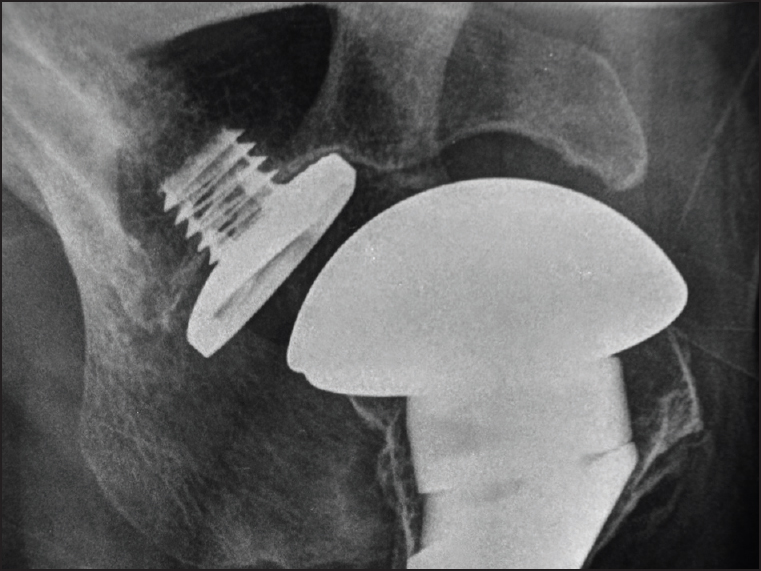 | Figure 4: Axillary lateral radiograph demonstrating a loose glenoid baseplate (proven at revision surgery)
Click here to view |
The mode of failure of each of the revisions was examined [Table 1]. All were ultimately attributed to a failure to achieve secondary stability of the base plate [Figure 5].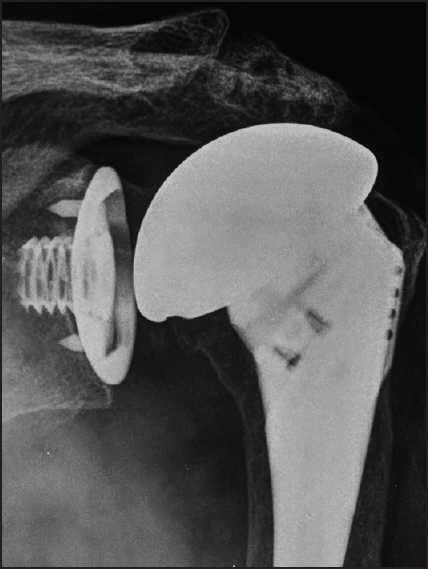 | Figure 5: Anterior-posterior radiograph demonstrating the glenoid baseplate subsiding from the cage screw leading to screw head prominence and polyethylene liner disengagement
Click here to view |
There were no problems with stability noted at the time of implantation. Polyethylene dislocation was more common in early (<2 years) and screw fracture later; however, all modes occurred at varied time intervals. In each of the three cases of prosthetic fracture, it was the cage screw that fractured. The intraoperative findings were that the deep portion of the cage screw was well-fixed to the glenoid and required manual extraction techniques to remove it. The superficial portion of the cage screw (exposed by the recession of the glenoid beneath the base plate) was sheared off [Figure 6]. | Figure 6: Retrieval specimen, cage screw with failure at bone-implant interface and no evidence of bone on-growth to the glenoid component
Click here to view |
The base plate was loose without evidence of bony on-growth in all cases [Figure 7]. Metallosis was noted in three cases.
The majority of patients were revised to a cemented keeled glenoid component with or without bone graft. Three patients had the cage screw tightened at their initial revision surgery. This restored stability intra operatively however all went on to have ongoing base plate instability with two revised, and the other symptomatically requiring revision but unable to take the necessary time for recovery. One patient at the time of revision had insufficient bone stock for immediate re-implantation; they had grafting to their glenoid and have not come to require glenoid component re-implantation. One patient has subsequently been revised a 2 nd time to a reverse prosthesis.
 Discussion Discussion | |  |
This single surgeon consecutive series of TSA demonstrates an unsatisfactorily high rate of revision, primarily due to the failure of the uncemented metal-backed glenoid component. Not all arthroplasties failed due to the glenoid component loosening, however, the soft-tissue complications and single peri-prosthetic fracture are within the observed rates of failure of other arthroplasty designs. [19]
The revisions occurred in the early to medium term. The observed mechanisms of failure were of three types:
- The polyethylene disengaged from the base plate due to relative prominence of the cage screw head as the loose backing plate receded with the resorption of the bony glenoid.
- The central exposed portion of the cage screw fractured with shear forces at the resorbed glenoid level, or
- The loose baseplate generated pain due to interface motion.
All of these failure modes can be related back to the lack of on-growth to the glenoid baseplate. The central cage screw provided excellent purchase into the glenoid neck bone and via an interference fit compressed the base plate onto the prepared glenoid surface at the time of implantation.
However, the baseplate design did not include a locking mechanism of this screw to the baseplate to prevent recession of the baseplate off the fixed screw in the event of slow bone incorporation. Subsequent subsidence of the glenoid backing bone occurred with excessive motion. [1] The polyethylene then disengaged off the base plate or the base plate wedged against the screw producing screw fracture. In order for long-term prosthetic stability, bone on-growth was required to the thin rim of the metal baseplate without the benefit of previously proven bone-metal caption modes, such as hydroxyappetite coatings, porous metal surfaces or trabecular metal.
Several of these modes of modular glenoid failure have previously been described, including polyethylene disengagement [15],[20],[21],[22] (but not due to the same mechanism as here), component fracture [13],[15],[23],[24] and failure to gain secondary stability. [25] A key feature of this prosthesis was the central cage screw, which we found to be rigidly attached to the bone, and we postulate that it should be retained in any revision of the prosthesis design.
We hypothesize that when combined axial loads and concurrent distraction loads with motion occurred, toggling of the baseplate increased subsidence of the glenoid bone. This could result in pain from interface motion, the screw head disengaging the polyethylene liner by its secondary prominence protruding off the base plate, or stress fracture of the screw head junction from repetitive motion. The screw relied on a compression fit with the glenoid baseplate, if a locking mechanism had been provided then potentially the design may have achieved better stability in the postoperative period and potentially long-term survival. Due to insufficient power, we were unable to determine if there were specific prosthesis components that were contributing to the very high level of observed failure or if, as we suspect, it was a fundamental design factor.
The Australian NJRR identified the implant as having a higher than anticipated rate of revision from 2010. [18] Subsequently, the manufacturer withdrew this implant from the Australian market in 2011 and has now been at least partially withdrawn worldwide and is no longer available for implantation in its current design. Interestingly, the humeral cage screw design of a short stem humeral prosthesis has not suffered from the same degree of failure. It is possible that the broader surface area of the humeral base plate may allow adequate metal to bone on-growth (as opposed to in-growth) to prevent failure at that level, but the different biomechanics of the axial and tension loads between humeral neck and glenoid may also explain this difference.
This paper highlights the role of registries in identifying prosthesis that have higher than anticipated rates of revision. However, the Australian registry is unable to examine clinical factors leading to failure, and may show a lag period to the publication of higher revision numbers from recognition in clinical practice.
The primary weakness of this study is that it is a single surgeon series, and this leaves the results open to criticism of factors associated with technique leading to failure. However, it reflects the experience of others as identified by the Australian NJRR. [18] The NJRR has a robust three stage review process that identifies prostheses with a higher than anticipated risk of revision. This prosthesis was identified in consecutive years prior to its withdrawal. The senior author is fellowship trained in shoulder surgery and has experienced similar results to other authors with other prostheses. [4]
There is much to be learned from this experience. It is imperative that we examine the mode of failure once a prosthesis is identified by a registry as having a higher than anticipated rate of revision in order to avoid future replication of errors.
Modes of failure in other metal backed glenoids include excessive wear, [20] dissociation with a well-fixed baseplate, [21] peri-prosthetic lucency from pegs (both with and without cement) leading to loosening, [5],[7] and uneven wear. [23]
Modular glenoid components have the theoretical advantage of achieving a stable bone prosthesis interface but are yet to reliably reach this level of functionality in clinical practice as their all polyethylene counterparts.
 References References | |  |
| 1. | Matsen FA 3 rd , Clinton J, Lynch J, Bertelsen A, Richardson ML. Glenoid component failure in total shoulder arthroplasty. J Bone Joint Surg Am 2008;90:885-96.  |
| 2. | Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop 2009;80:83-91.  |
| 3. | Cofield RH. Total shoulder arthroplasty with the Neer prosthesis. J Bone Joint Surg Am 1984;66:899-906.  [ PUBMED] |
| 4. | Groh GI. Survival and radiographic analysis of a glenoid component with a cementless fluted central peg. J Shoulder Elbow Surg 2010;19:1265-8.  |
| 5. | Fox TJ, Cil A, Sperling JW, Sanchez-Sotelo J, Schleck CD, Cofield RH. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg 2009;18:859-63.  |
| 6. | Walch G, Young AA, Boileau P, Loew M, Gazielly D, Molé D. Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis: Results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am 2012;94:145-50.  |
| 7. | Boileau P, Avidor C, Krishnan SG, Walch G, Kempf JF, Molé D. Cemented polyethylene versus uncemented metal-backed glenoid components in total shoulder arthroplasty: A prospective, double-blind, randomized study. J Shoulder Elbow Surg 2002;11:351-9.  |
| 8. | Wirth MA, Loredo R, Garcia G, Rockwood CA Jr, Southworth C, Iannotti JP. Total shoulder arthroplasty with an all-polyethylene pegged bone-ingrowth glenoid component: A clinical and radiographic outcome study. J Bone Joint Surg Am 2012;94: 260-7.  |
| 9. | Nho SJ, Frank RM, Verma NN, Romeo AA. Incidence of early development of radiolucent lines in keeled polyethylene glenoid components after total shoulder arthroplasty. Am J Orthop (Belle Mead NJ) 2010;39:333-7.  |
| 10. | Barwood S, Setter KJ, Blaine TA, Bigliani LU. The incidence of early radiolucencies about a pegged glenoid component using cement pressurization. J Shoulder Elbow Surg 2008;17:703-8.  |
| 11. | Godenèche A, Boileau P, Favard L, Le Huec JC, Lévigne C, Nové-Josserand L, et al. Prosthetic replacement in the treatment of osteoarthritis of the shoulder: Early results of 268 cases. J Shoulder Elbow Surg 2002;11:11-8.  |
| 12. | Taunton MJ, McIntosh AL, Sperling JW, Cofield RH. Total shoulder arthroplasty with a metal-backed, bone-ingrowth glenoid component. Medium to long-term results. J Bone Joint Surg Am 2008;90:2180-8.  |
| 13. | Budge MD, Nolan EM, Heisey MH, Baker K, Wiater JM. Results of total shoulder arthroplasty with a monoblock porous tantalum glenoid component: A prospective minimum 2-year follow-up study. J Shoulder Elbow Surg 2013;22:535-41.  |
| 14. | Clement ND, Duckworth AD, Colling RC, Stirrat AN. An uncemented metal-backed glenoid component in total shoulder arthroplasty for osteoarthritis: Factors affecting survival and outcome. J Orthop Sci 2013;18:22-8.  |
| 15. | Wallace AL, Phillips RL, MacDougal GA, Walsh WR, Sonnabend DH. Resurfacing of the glenoid in total shoulder arthroplasty. A comparison, at a mean of five years, of prostheses inserted with and without cement. J Bone Joint Surg Am 1999;81:510-8.  |
| 16. | Castagna A, Randelli M, Garofalo R, Maradei L, Giardella A, Borroni M. Mid-term results of a metal-backed glenoid component in total shoulder replacement. J Bone Joint Surg Br 2010;92:1410-5.  |
| 17. | Habermeyer P, Engel G. Surgical technique for total shoulder arthroplasty . Oper Orthop Traumatol 2004;16:339-64.  |
| 18. | |
| 19. | Matsen SF 3 rd , Clinton J, Rockwood CA Jr, Wirth MA, Lippitt SB. Glenohumeral arthritis and its management. In: Rockwood CA Jr, Matsen SE 3 rd , editors. The Shoulder. 4 th ed. Philadelphia: Saunders Elsevier; 2009. p. 1089-246.  |
| 20. | Cheung EV, Sperling JW, Cofield RH. Polyethylene insert exchange for wear after total shoulder arthroplasty. J Shoulder Elbow Surg 2007;16:574-8.  |
| 21. | Wallace AL, Walsh WR, Sonnabend DH. Dissociation of the glenoid component in cementless total shoulder arthroplasty. J Shoulder Elbow Surg 1999;8:81-4.  |
| 22. | Kirk PG, Sorger J. Failure of an implant after total shoulder arthroplasty. A case report. J Bone Joint Surg Am 1997;79:597-8.  |
| 23. | Gunther SB, Graham J, Norris TR, Ries MD, Pruitt L. Retrieved glenoid components: A classification system for surface damage analysis. J Arthroplasty 2002;17:95-100.  |
| 24. | Fucentese SF, Costouros JG, Kühnel SP, Gerber C. Total shoulder arthroplasty with an uncemented soft-metal-backed glenoid component. J Shoulder Elbow Surg 2010;19:624-31.  |
| 25. | Goodman S, Wang JS, Doshi A, Aspenberg P. Difference in bone ingrowth after one versus two daily episodes of micromotion: Experiments with titanium chambers in rabbits. J Biomed Mater Res 1993;27:1419-24.  |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7]
[Table 1]
|
