| |


 |
| Year : 2016 | Volume
: 10
| Issue : 1 | Page : 44-47 |
|
|
|
|
|
TECHNICAL TIP Fracture of the proximal humerus with disruption of the tendon of the pectoralis major
Bart M Berghs1, Alexander Van Tongel2, Thomas De Bo2, Lieven F De Wilde2
1 Department of Orthopedic Surgery and Traumatology, AZ Sint-Jan AV, Brugge, Belgium
2 Department of Orthopedic Surgery and Traumatology, Ghent University Hospital, Ghent, Belgium
Correspondence Address:
Bart M Berghs
Department of Orthopedic Surgery and Traumatology, AZ Sint-Jant AV, Ruddershove 10, B-8000 Brugge
Belgium
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/0973-6042.174521
 |
|
|
|
| Date of Web Publication | 20-Jan-2016 |
 Abstract Abstract | | |
Combined pectoralis major disruption and proximal humeral fractures are uncommon. A simple radiologic diagnostic tool which consists of the measurement of the displacement from the humeral shaft to the lateral side of the humeral head (lateral to the outer proximal cortex) can help to diagnose this combined lesion.
Keywords: Disruption, pectoralis major, proximal humerus fracture, radiographic analysis
How to cite this article:
Berghs BM, Tongel AV, Bo TD, De Wilde LF. Fracture of the proximal humerus with disruption of the tendon of the pectoralis major. Int J Shoulder Surg 2016;10:44-7 |
 Introduction Introduction | |  |
Treating proximal humeral fractures remains a challenge, as complications and failures are not rare. We report on a fracture of the proximal humerus with associated pectoralis major disruption. Although a proximal humeral fracture with avulsion of the pectoralis major has a specific radiographic appearance and requires a specific treatment, it cannot be classified in any of the contemporary classification systems. The more recent distinct classification system for proximal humeral shaft fractures introduced by Stedtfeld and Biber [1] does not allow the inclusion of this fracture type either. Nevertheless, recognizing the pathological anatomy of this fracture allows a specific treatment strategy.
Diagnostic technique of a proximal humeral fracture with avulsion of the pectoralis major
Understanding and recognizing the pathological anatomy of a proximal humeral fracture are essential to determine the optimal treatment. Several classifications have been conceived, but they focus mainly on the number of fractured parts of the humerus and their anatomical location (humeral head, greater tuberosity, lesser tuberosity, and diaphysis). [2],[3],[4]
Recently, more interest was given to the degree of comminution of the fractured parts and the displacement of the humeral diaphysis, as it appeared to have distinct prognostic implications: A medial comminution has a tendency to displace in varus and to result in a symptomatic malunion or pseudarthrosis of the collum chirurgicum; [5],[6] a thin and comminuted greater tuberosity has a greater tendency of fading or resorbing; [7] a lateral displacement of the humeral diaphysis of more than 5 mm has a higher probability to develop an osteonecrosis. [5]
In our limited experience, a posterolateral displacement of the humeral shaft, further than the outer lateral cortex of the proximal humerus is important to recognize as a separate pathological entity, as this displacement seems to be indicative for a disruption of the pectoralis major, either a rupture of the tendon or an avulsion fracture. To our knowledge, only one case report of this combined injury with its typical displacement of the shaft has been published. [8]
This fracture type should be considered as a separate entity for several reasons. First, a humerus fractured through its surgical neck is driven into varus because of the action of the rotator cuff muscles on the tuberosities on the proximal part, and because of the ascending force of the deltoid on the distal part. The pectoralis major muscle antagonizes the forces exerted by the supraspinatus and deltoid muscles in the adducted arm. Disruption of the pectoralis major will, therefore, only increase this varus force. Second, the fractures displaced more than 1 cm are usually caused by high-energy trauma, and therefore, often accompanied by severe comminution. Comminution of the medial wall, the so-called calcar, compromises the ability to withstand the tendency to displace in varus. [5]
In our experience, the lateral plating alone is often insufficient, as shown in our first case. In our second case, the fracture type is different as it is located more distally, and the calcar itself is not involved. Nevertheless, although the same forces apply, a centromedullary device is able to prevent the secondary displacement of the proximal humerus. In this specific case, the pectoralis major avulsion fracture was not addressed, leaving the patient with a clinical condition comparable with conservatively treated pectoralis major tendon avulsion. [9],[10]
Clinical series of patients
Case 1
A 33-year-old man was injured in his upper body by a falling metal fence. He was admitted to the emergency department of the University Hospital Ghent. Clinically, he had no apparent neurovascular dysfunction of the left arm. More specifically, the sensory function of the axillary nerve was normal. Motor evaluation of the upper arm was impossible due to pain inhibition. Plain X-ray [Figure 1] showed a comminuted two-part surgical neck fracture of the humerus, with a proximal, lateral and posterior displacement of the humeral shaft. Computed tomography scan confirmed this position of the distal part and showed an undisplaced fracture of the greater tuberosity. | Figure 1: Plain anteroposterior X-ray of the two-part surgical neck fracture. Notice the proximal and lateral displacement of the distal fragment, further than the lateral cortex of the proximal fragment
Click here to view |
The patient underwent an open reduction and internal fixation with plate and screw (S3 Humeral Plate System; DePuy, Kirkel-Limbach, Germany) on the same day. Through a standard deltopectoral approach, a bare area on the anterior aspect of the humeral shaft, corresponding to the pectoralis major insertion site, was noticed. Further exploration revealed a complete rupture of the pectoralis major at the level of its insertion with retraction of the tendinous part. The tendon was identified and tagged with five Ethibond n° 5 sutures (Ethicon, Inc., Somerville, New Jersey). Reduction and internal fixation of the three-segment two-part proximal humerus fracture were performed with a plate [Figure 2]. The insertional site of the pectoralis major on the anterior aspect was debrided of remnant tendon, with minimal abrasion of the anterior cortex. The Ethibond sutures were then passed through the plate holes near the anatomical insertion site of the pectoralis major tendon.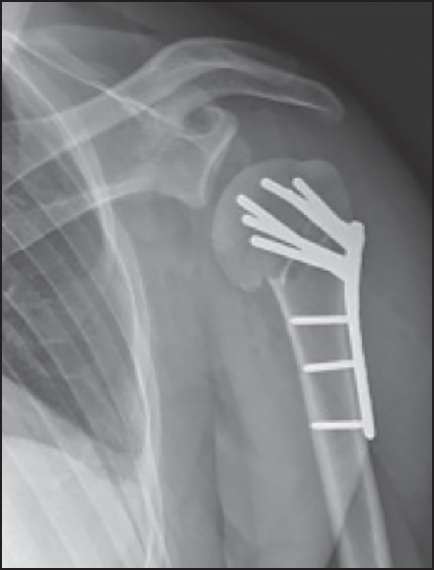 | Figure 2: Plain anteroposterior X-ray after open reduction and internal fixation on the first postoperative day
Click here to view |
Postoperatively, an adduction sling was used for 6 weeks. Passive mobilization was started immediately, without external rotation. The early postoperative period was uneventful. At 6 weeks, the patient was allowed to start active mobilization, without external rotation over 30°, until 12 weeks postoperatively.
At clinical examination 3 months postoperatively, passive external rotation was limited: External rotation in adduction was 20° versus 90° on the unaffected side, external rotation in 90° abduction was 30° versus 90° on the unaffected side.
One year postoperatively, the patient did not recover his preinjury level of performance. His absolute Constant-Murley score reached 76/100 (12/15 pain; 18/20 activities of daily living [ADL]; 40/40 mobility; and power 6/25) versus 91/100 (15/15 pain; 20/20 ADL; 40/40 mobility; and power 16/25) at the unaffected side with only restrictions for power. X-ray confirmed consolidation of the proximal humeral fracture, with varus malunion, and shortening of the medial column [Figure 3].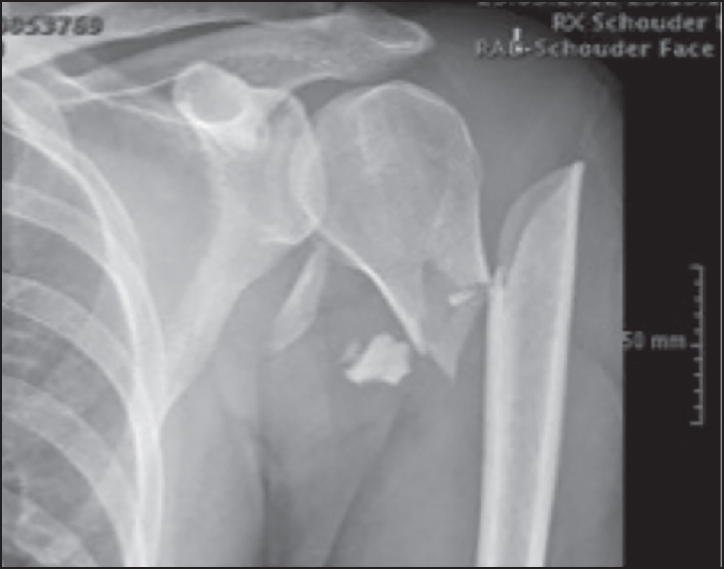 | Figure 3: Plain anteroposterior X-ray of the two-part proximal humerus fracture. Notice the lateral displacement of the distal fragment, further than the lateral cortex of the proximal fragment
Click here to view |
Case 2
A 36-year-old man consulted the out-patient clinic 1-year after a work-related trauma. He sustained a posterior fracture dislocation of the right hip and a two-part proximal humeral fracture at the meta-diaphyseal level of the left shoulder. Plain X-ray of the shoulder [Figure 4] showed a comminutive fracture of the humerus with lateral displacement of the shaft. Open reduction and internal fixation of the posterior acetabular rim were performed and intramedullary fixation of the humerus. Postoperative radiograph [Figure 3] showed a very satisfactory reduction. The early postoperative period was uneventful. | Figure 4: Plain anteroposterior X-ray after intramedullary fixation on the first postoperative day
Click here to view |
One year later, the patient still experienced pain, aggravating at night. On clinical examination, the elevation was limited to 80°, and he had a general atrophy of his left upper arm. Electromyography revealed a recovering brachial plexus injury. Constant-Murley score [2] reached only 44/100 (10/15 pain; 12/20 ADL; 22/40 mobility; and power 0/25) versus 93/100 (15/15 pain; 20/20 ADL; 40/40 mobility; and power 18/25) for the unaffected side. Besides the loss of power and limited range of motion, he experienced an induration at the anterior fold of his axilla. At the outpatient visit, 1-year after the injury, plain X-ray [Figure 3] showed a nonunion of a butterfly fragment that was displaced from its initial site. It was located in the anterior fold of the axilla. Ultrasound and CAT-scan [Figure 5] confirmed its position and showed the continuity of the fragment with the pectoralis major muscle. Due to the predominantly neurogenic pain complaints, related to the recovering brachial plexus lesion, it was decided not to repair the pectoralis major tendon avulsion and to continue physiotherapy.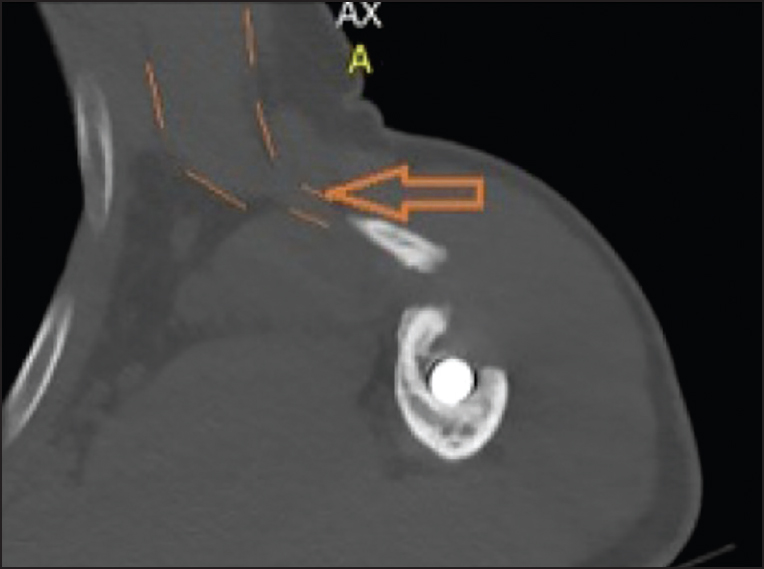 | Figure 5: Computed tomography scan of the nonunited fragment, confirming continuity with pectoralis major
Click here to view |
 Conclusion Conclusion | |  |
We report on a specific and easily recognizable entity of proximal humeral fractures that requires a specific surgical approach: A two-part surgical neck fracture with the displacement of the humeral shaft lateral and posterior to the outer cortex of the proximal humerus, appears to be accompanied by a rupture or avulsion of the pectoralis major muscle, and requires an open reduction and internal fixation of the fracture through a deltopectoral approach, whether or not reinforced with a centromedullary allograft, and repair of the pectoralis major either with suture anchors or by transosseous repair.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
 References References | |  |
| 1. | Stedtfeld HW, Biber R. Proximal third humeral shaft fractures - A fracture entity not fully characterized by conventional AO classification. Injury 2014;45 Suppl 1:S54-9.  |
| 2. | Majed A, Macleod I, Bull AM, Zyto K, Resch H, Hertel R, et al. Proximal humeral fracture classification systems revisited. J Shoulder Elbow Surg 2011;20:1125-32.  |
| 3. | Neer CS 2 nd . Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970;52: 1077-89.  |
| 4. | Resch H, Beck E, Bayley I. Reconstruction of the valgus-impacted humeral head fracture. J Shoulder Elbow Surg 1995;4:73-80.  |
| 5. | Hardeman F, Bollars P, Donnelly M, Bellemans J, Nijs S. Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury 2012;43:153-8.  |
| 6. | Sohn HS, Shin SJ. Minimally invasive plate osteosynthesis for proximal humeral fractures: Clinical and radiologic outcomes according to fracture type. J Shoulder Elbow Surg 2014;23: 1334-40.  |
| 7. | Tingart MJ, Apreleva M, von Stechow D, Zurakowski D, Warner JJ. The cortical thickness of the proximal humeral diaphysis predicts bone mineral density of the proximal humerus. J Bone Joint Surg Br 2003;85:611-7.  |
| 8. | Kono M, Johnson EE. Pectoralis major tendon avulsion in association with a proximal humerus fracture. J Orthop Trauma 1996;10:508-10.  |
| 9. | Wolfe SW, Wickiewicz TL, Cavanaugh JT. Ruptures of the pectoralis major muscle. An anatomic and clinical analysis. Am J Sports Med 1992;20:587-93.  |
| 10. | Zeman SC, Rosenfeld RT, Lipscomb PR. Tears of the pectoralis major muscle. Am J Sports Med 1979;7:343-7.  [ PUBMED] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|
