|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 2
| Issue : 1 | Page : 8-14 |
|
Knowledge and utilization of HIV counseling and testing services among students of a tertiary institution in Abia State, South East Nigeria
Ugochukwu U Onyeonoro1, Obiageli F Emelumadu2, Abali Chuku3, Okezie O Kanu4, Uzo E Ebenebe2, Nkiru Onwukwe5, Chidinma Uwakeme5, Emmanuel Ndukwe5
1 Department of Community Medicine, Federal Medical Centre, Umuahia, Abia State, Nigeria
2 Nnamdi Azikiwe University, Nnewi Campus, Nnewi, Anambra State, Nigeria
3 Department of Opthalmology, Federal Medical Centre, Umuahia, Abia State, Nigeria
4 Department of Neurosurgery, Lagos University Teaching Hospital, Idi Araba, Lagos, Lagos State, Nigeria
5 Abia State University, Aba Campus, Aba, Abia State, Nigeria
| Date of Acceptance | 21-May-2014 |
| Date of Web Publication | 1-Jul-2014 |
Correspondence Address:
Ugochukwu U Onyeonoro
Department of Community Medicine, Federal Medical Centre, Umuahia, Abia State
Nigeria
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-9157 .135743

Introduction: In Nigeria, despite increasing availability HIV counseling and testing (HCT) services, uptake of HCT among youths has remained significantly low. Although, youths are at greater risk of HIV infection many of them do not access HCT services. Consequently, this study is aimed at ascertaining knowledge and level of uptake of HCT services among students in tertiary institution in South East Nigeria. Methodology: The study is a cross-sectional, descriptive survey involving a total of 312 students selected by multi-staged sampling technique. Responses were elicited from them using a pretested, self-administered questionnaire on bio-data, knowledge of HCT, desire for HIV testing, risk perception, access and utilization of HCT services. Data collected were analyzed using SPSS version 17. Findings: Analysis of the data showed that 184 (59%) of the students were aware of HCT, with a slightly greater male preponderance than females. Common sources of information on HCT were media (49.5%), friends (25.0%), and health worker (20.7%). Majority (78%) of them desired to be desired for HIV; however, only 138 (44.2%) had ever been tested for HIV, among which 86 (62%) were tested voluntarily. Most common reasons for testing for HIV were, to know their status (51.4%), admission into school (17%), blood transfusion (9%) and during illness (7%). Common reasons for not desiring to be tested were - not aware of any HCT center (37.1%), fear of test result (22.9%), distance (8.6%) and stigma (8.6%). One hundred and ninety-three (62%) students felt that they have a high chance of acquiring HIV infection. Conclusion: Despite high awareness and desire to be tested for HIV, uptake of HCT services remains low among students in tertiary institution, therefore adoption of youth-friendly approaches will improve uptake of HIV testing among them. Keywords: Aba, information, perception, risk, South East Nigeria, uptake, youth
How to cite this article:
Onyeonoro UU, Emelumadu OF, Chuku A, Kanu OO, Ebenebe UE, Onwukwe N, Uwakeme C, Ndukwe E. Knowledge and utilization of HIV counseling and testing services among students of a tertiary institution in Abia State, South East Nigeria. J HIV Hum Reprod 2014;2:8-14 |
How to cite this URL:
Onyeonoro UU, Emelumadu OF, Chuku A, Kanu OO, Ebenebe UE, Onwukwe N, Uwakeme C, Ndukwe E. Knowledge and utilization of HIV counseling and testing services among students of a tertiary institution in Abia State, South East Nigeria. J HIV Hum Reprod [serial online] 2014 [cited 2018 Feb 19];2:8-14. Available from: http://www.j-hhr.org/text.asp?2014/2/1/8/135743 |
| Introduction | |  |
HIV counseling and testing (HCT) has been recognized as the crux of HIV surveillance, prevention, and treatment programs. It is described as a process by which an individual undergoes counseling, enabling him or her to make an informed choice about being tested for HIV. It enables people to learn whether they are infected, understand the implications of their serostatus, and make more informed choices for the future. It has been described as a vital entry point to HIV services, including prevention, care and support. It also provides essential knowledge and support that enable uninfected people to remain so and enable those infected with HIV to plan for the future and prevent HIV transmission to others. Those who are infected can also benefit from available care, treatment and support services. Knowledge of HIV infection is a prerequisite to initiating antiretroviral therapy a long-term treatment of people living with HIV, and most infected people in sub-Saharan Africa (SSA) are unaware of their status. [1],[2],[3],[4] Studies have shown that a number of factors affect acceptability and uptake of HIV counseling and testing, among which are awareness and knowledge of voluntary counseling and testing, availability of HCT services, perception of HIV, stigma, cost and distance and availability of other HIV services. [4]
In the past few years, there have been global efforts to attain universal access target for all HIV services, including HCT services. In Nigeria, measures taken to increase utilization of HCT services include, among others, dissemination of HCT-related behavior change communication messages through mass media and use of information, education and communication materials, establishment of additional HCT centers particularly in remote areas, provision of free HCT services, reduction of interval between testing and result, and integration of HCT services with maternal and child health and tuberculosis services. The success of these intervention has been modest, hence there is a need to examine pattern of HCT uptake in the country, especially among the at-risk population including youths. [5] The question then is to what extent has previous interventions impacted on youth's knowledge and uptake of HCT? For instance in Abia State, one of the measures taken to improve utilization of HCT services was establishment of stand-alone HCT facilities in three tertiary institutions (excluding Abia State Polytechnic, Aba, Abia State, Nigeria) by a nongovernmental organization with support from a World Bank-funded HIV/AIDS project few years ago. Establishment of these HCT facilities in the respective institutions resulted in increased uptake HCT among students of these institutions, but these facilities have long ceased to function since the end of project. [6]
Between 2005 and 2007, the National HIV/AIDS Reproductive Health Survey (NARHS) [7],[8] revealed an overall decline in knowledge of HIV in South East Nigeria, even though there was a marginal increase in uptake of HCT. Anecdotal evidence suggests that most people tested for HIV were pregnant women attending antenatal clinics, people who have been previously sick, or those intending to get married. In addition, mandatory HIV testing was carried for employment, admission, and overseas travel. Most health facilities, particularly the private facilities also carry out routine HIV testing for surgical patients and pregnant women, but not in line with the national guidelines. Some of these measures rather than increase uptake of HCT services have resulted in increased stigmatization.
According to the NARHS report, [8] as at 2007 the proportion of young people ever tested for HIV in the country were, for 15-19 years old 7.0% and 7.1% and for 20-24 years old 13.2% and 15.3% for males and females respectively. In addition, a review of the records of facilities providing HCT in accordance to the national guidelines in Abia State, revealed that a total of 22, 338 (1.5%) persons out of an estimated population of 1,496,645 eligible (≥15 years) persons received HCT as at 2009. [5]
Young people are vulnerable and are greater risk of acquiring HIV infection compared to adults. In SSA, about 50% of new HIV infections occur among youths aged between 15 and 24 years. [9] Among the factors responsible for high incidence of HIV among this group are; premarital sex, multiple concurrent sexual partnerships, transactional sex and low use of condom. In Abia State HIV prevalence among young women aged 15-24 years in urban areas increased from 1% in 2005 to 5.9% in 2008. [5],[10] Despite, obvious vulnerability of this group to HIV infection, HIV interventions, including HCT services targeting them are few. In Nigeria, HCT services are predominantly clinic-based. Consequently, youths are disproportionately disadvantaged because they do not often utilize clinic services like their adult counterparts. The current orientation and pattern of provision of health care services in the country is not youth-friendly. Furthermore, health programs addressing young people sexual and their reproductive health needs are limited both in scope and coverage, and are poorly integrated into the existing health care system, thereby limiting their access to HCT services. It has been shown that increasing access to HCT services to youths not only enhance access to HIV services but also promote initiation of risk reduction behaviors. [9]
The recently developed National HIV/AIDS Strategic Plan (2010-2015) [11] is focused on attaining universal access goal of providing HCT services to 80% of the (eligible) population. The plan provides for measures to improve access to the hard to reach populations such as youths. Understanding current pattern and factors influencing uptake of HCT services among youths is important in evolving appropriate and innovative approaches of reaching a significant proportion of them with HCT services.
Therefore, this study is aimed at ascertaining the level of knowledge and uptake of HCT among students of Abia State Polytechnic, Aba, Abia State, Nigeria.
| Methodology | |  |
The study is a cross-sectional, descriptive study carried out in a tertiary institution-Abia State Polythecnic, Aba, Abia State, Nigeria. The institution is located in Aba a major commercial town, with a high population density. Besides commerce, there is huge presence of large, medium and small scale industries; however, the town is largely characterized by poor physical infrastructure. As a result of the commercial activities in the town, it attracts a lot of businessmen in transit who sometimes engage in transactional sex. Furthermore, there is high predominance of out-school youths, who are traders, apprentices, "keke" drivers (tricyclists) and commercial drivers or their assistants. In additon, activities of commercial sex work are high in the town. Attendant effects of the high level of economic activities include increasing male school drop-out rate. On the other hand, literacy rate is relatively high (85%). Physical access to health care services is high, but rising cost of quality health care services remains a major barrier. Some public and private health care facilities in the town provide HIV services including HCT services. There are also several educational institutions both private and public ranging from primary, secondary to postsecondary institutions.
Abia State polytechnic is one of the five public tertiary institutions in the state. The institution was established in 1992 and has four Schools of Business and Management Technology, Science and Industrial Technology, Science and Engineering Technology and Environmental Development and Technology, all which comprise of six, two, three, and six departments, respectively giving a total of 17 departments. Each Department has two Ordinary National Diploma (OND) classes and two Higher National Diploma (HND classes), and average number of students/class is 80 (60-100). Thus, the institution has a student population of 5,440. Being a state-owned institution greater proportion of the students are indigenes from Abia State, however there are few nonindigenes from other states also admitted into its academic program. The school has a health center with a medical officer in-charge that provides primary health care services to the academic community on out-patient basis. HIV interventions are carried out in the institution through a number of school-based organizations and some nongovernmental youth organizations based outside the school. The school medical center does not routinely provide HCT services to the students.
A total of 320 students were selected using a multi-stage sampling technique. First, from the list of all the departments in the school, four departments were selected by simple random sampling. From each of the selected departments, a total of 40 students each were selected from the OND2 and HND1 class by simple random sampling. Data were collected by three trained research assistants who were clinical medical students of Abia State University, Aba Campus, Aba using a pretested, semi-structured, self-administered questionnaire. Responses were elicited from the selected students on personal data, knowledge of HCT, desire for HIV testing, risk perception, access and utilization of HCT services. Only students who consented after due explanation of the purpose and procedure of the study and assurance of confidentiality were enrolled into the study. Consent was verbal and in event of a selected respondent declines to participate in the study or withdraws his/her consent he/she was replaced by another consenting student. Furthermore, institutional approval to carry out the study was obtained from the school authority. Data collected were first entered into Ms Excel (Microsoft Corporation, Washington, USA) and exported to SPSS version 17 (SPSS Inc., Chicago Illinois, USA) for analysis.
| Results | |  |
A total of 320 questionnaires were distributed and retrieved. Three hundred and twelve questionnaires were duly completed, and the remaining eight that were poorly completed were discarded giving a response rate of 97.5%. Of the 312 respondents analyzed, 186 (59.6%) were males and 126 (40.4%) were females. The mean age of the boys and the girls was 23.3 ± 3.3 years and 22.8 ± 3.1 years, respectively. Majority (92.6%) of them were never married, 6.7% were married and the remainder were either separated or widowed. One hundred and eighty four students (59%) were aware of HCT, out of which 60.2% and 57.1% of males and females respectively have heard of HCT. [Table 1] shows sources of information on HCT and knowledge of HCT and they were media (49.5%), friends (25.0%) and health worker (20.7%). Among those that have of heard of HCT, 68.4% said it is associated with HIV/AIDS, and a greater proportion were girls (76.8%).
Among those that have heard of HCT, only 103 (56.0%) of them knew of place where HCT could be accessed. Sixty-five (58.0%) of the males and 38 (52.8%) of the female students knew of places where HCT could be provided.
Two hundred and forty-two (77.6%) students had desired to be tested for HIV, however less than half (44.2%) of them had HIV test done as shown in [Table 2].
[Figure 1] shows the proportion of individual desiring HCT that were actually tested for HIV. Only 57% of all respondents desiring to be counseled and tested for HIV were actually tested, and a greater proportion of females (60.2%) desiring HCT than males (54.9%) were tested.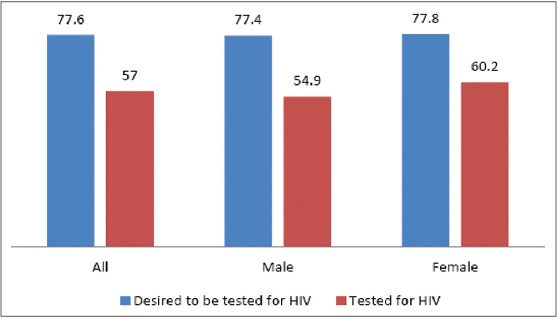 | Figure 1: Proportion of individuals desiring HIV counseling and tested for HIV
Click here to view |
[Table 3] shows reasons for undergoing HIV test and they include; to know my status (51.4%), school admission (16.7%), blood transfusion (9.4%), and during illness (7.2%). Further, analysis revealed that besides knowing their status more boys than girls were tested during blood transfusion (13.2%) and for employment (5.1%), while more girls than boys did HIV test for school admission (22.0%), during illness (10.2%) and for marriage (8.5%).
Seventy students (22.4%) said that they do not have the desire to be tested for HIV. The reasons they gave were as follows; not aware of any HIV testing center (37.1%), fear of test result (22.9%), distance (8.6%), and fear of stigma (8.6%) [Table 4].
One hundred and ninety-three students (61.9%) felt that they have a high chance of acquiring HIV infection, while 40 (12.8%) felt that they have no chance of being infected with HIV. As shown in [Table 5], a total 229 (73.6%) students were of the opinion that HCT is important. However, there no significant association was observed between gender and HIV risk perception (χ2 = 2.66, P = 0.26) and perception of importance of HCT (χ2 = 1.45, P = 0.48).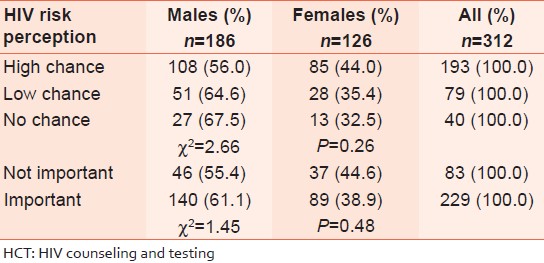 | Table 5: Respondents perception of risk of acquiring HIV infection and perception of importance of HCT
Click here to view |
| Discussion | |  |
Awareness of HCT among the respondents was only 59%, in contrast to previous studies, which have reported high awareness of HCT among students in tertiary institutions in Nigeria. [12],[13] Media was the most common source of information on HCT, followed by friends and health workers. An earlier study among undergraduate students in Anambra State reported that beside the media, churches were the next most common source of information on HCT, [12] while friends/relatives were the most common source of information on HCT in Uganda, followed by media and billboards. [14] In Zambia, enhanced capacity of youths to provide HCT information to their peers was found to have increased uptake of HCT among youths. [15] Therefore, expanding youths' access to HIV information is important in improving access to HCT services, and will as well impact positively on reducing HIV transmission among them.
Only 56% of the students were knowledgeable of places where they can get HIV test, and a slightly greater proportion of them were males. Similarly, National HIV/AIDS Reproductive Health Survey (NARHS), reported that 57% males and 51.4% females aged 20-24 knew of places to get HIV test. [8] Elsewhere in Africa, 90% of undergraduate students in Ghana, 74% of health care professionals in training in Tanzania and 28% of Ugandan undergraduate students were knowledgeable of place where HCT services can be obtained. [16],[17],[18]
Desire to get tested for HIV was quite high (77.7%) among the students, however, only about 44.3% of them had actually been tested for HIV an observation, which has been reported in previous studies that most students in tertiary institutions had not taken HIV test. [8],[12],[16] In general, in SSA desire to get tested for HIV is quite high between 75% and 90%, but low uptake of HIV test remains prevalent, including among young people. [19] Low uptake of HCT services among young people in higher institution could be attributed to the current approach of providing HCT services. The current approach of providing HCT information and services via health facilities is more favorable to the adults, who have been found to utilize health services more than youths. [20],[21] A study among students in Tanzania revealed that most in-school youths prefer school-based HCT services or HCT services integrated into other reproductive health programs. [17]
In general, an evaluation of HIV in SSA revealed that youths are not accorded due priority in most interventions including HCT services. [20],[21] However, it is important that young people be accorded priority in HIV prevention considering their high susceptibility to HIV infection. Furthermore, the transitory nature of youth makes sustained school-based HIV program imperative in HIV control, because each passing year more children transit from childhood to adulthood. Hence missing a generation may reverse previous gains already achieved and will impact negatively on the overall HIV control efforts. [21]
Although, majority of students did not pay for HIV test, about 38% of them did. Paying for HIV test is a major barrier to young people's utilization of HCT services. Provision of free HCT services is vital to increasing uptake HIV test, yet many health facilities in the country still charge fee for the test. [22],[23],[24] Since, most undergraduate students desired to be tested for HIV, financial barriers should be addressed alongside other social barriers that limits their access to HIV testing.
The most common reason preferred by the students for doing HIV test was to know their status. Willingness to know their serostatus was a stronger motivation for HIV test for male students, while school admission, illness and marriage were a stronger motivation for their female counterparts. Similarly, in the general population desire to know one's HIV status (90.7%) was the most common reason for desiring HIV testing. [8] On the other hand reasons for not desiring to get tested for HIV included; lack of knowledge of where to get tested, fear of test result, distance and stigma. Generally, most people in Nigeria do not test for HIV because they feel it is not necessary, low risk perception, fear of the test result, stigma. [8],[21],[25] Elsewhere in Africa, youths do not desire HCT because of incurable nature of the disease, cost of treatment and never had sex. In communities where stigma is prevalent access to HCT services is limited and risky sexual behaviors are high. [26],[27] Therefore, it is noteworthy that interventions aimed at enhancing uptake of HCT among young people should address the following issues among others providing information on places where HCT could be accessed, anxiety about positive test, stigma and low risk perception. This is because, most people particularly young persons are concerned about how their serostatus will affect their relationship, career and livelihood and opportunity to access care and support. [15],[26]
Majority of the students felt that they have a high chance of acquiring HIV infection and more than 70% of them believe that HCT is important. More boys than girls considered HCT to be important, even though greater proportion of them feel that they have no chance acquiring the infection. Risk perception among the students we studied was higher when compared with health care professional students in Tanzania. [17] Studies elsewhere had reported that even though many students believe that HCT is important, most of them believe that they are not at risk of contracting HIV infection, which results in low uptake of HCT services. [28],[29]
| Conclusion | |  |
The study revealed high awareness and desire to be tested for HIV, but low uptake of HCT among students in tertiary institution. It also highlighted the need to address financial and social barriers limiting young people's access to HCT information and services. This could be achieved through collaboration between school authorities and relevant partners in establishing a sustainable youth-friendly, school-based HCT services. Furthermore, while efforts should be made to incorporate sexual reproductive health/HIV education into the training curriculum of tertiary institutions, the current peer education intervention should be strengthened and be used to promote HCT messages and referral.
| References | |  |
| 1. | Kasaija J, Nsabagasani X, editors. Community HIV Counselling and Testing a Handbook on Participatory Needs Assessment. Kampala, Uganda: Uganda Programme for Human and Holistic Development (UPHOLD); 2008. 
|
| 2. | USAID. Technical Issue Brief. HIV Counselling and Testing, 2010. Available from: http://www.usaid.gov. [Last accessed on 2011 Oct 10]. 
|
| 3. | Alwano-Edyegu MG, Marum E. Knowledge is Power: Voluntary HIV Counselling and Testing in Uganda. UNAIDS Case Study. Geneva: UNAIDS; 1999. 
|
| 4. | UNAIDS. Voluntary Counselling and Testing. UNAIDS Technical Update. Geneva: UNAIDS; 2000. 
|
| 5. | Ajuwon AJ, Titiloye M, Oshiname F, Oyewole O. Knowledge and use of HIV counseling and testing services among young persons in Ibadan, Nigeria. Int Q Community Health Educ 2010;31:33-50. 
|
| 6. | Onyeonoro UU, editor. Abia State HIV/AIDS Epidemiology, Response Policy Synthsis (ERPS). Umuahia, Nigeria: Abia State Agency for Control of AIDS (ABSACA); 2009. 
|
| 7. | FMOH. National HIV/AIDS Reproductive Health Survey (NARHS). Abuja, Nigeria: FMOH; 2005. 
|
| 8. | FMOH. National HIV/AIDS Reproductive Health Survey (NARHS). Abuja, Nigeria: FMOH; 2007. 
|
| 9. | Wusu O, Okoukoni S. The role of HIV counselling and testing in sexual health behaviour change among undergraduates in Lagos, Nigeria. Tanzan J Health Res 2011;13:27-32. 
|
| 10. | FMOH. National HIV Sero-Prevalence Sentinel Survey. Abuja, Nigeria: FMOH; 2008. 
|
| 11. | NACA. National HIV/AIDS Strategic Plan (2010-2015). Abuja, Nigeria: NACA; 2009. 
|
| 12. | Ikechebelu IJ, Udigwe GO, Ikechebelu N, Imoh LC. The knowledge, attitude and practice of voluntary counselling and testing (VCT) for HIV/AIDS among undergraduates in a polytechnic in Southeast, Nigeria. Niger J Med 2006;15:245-9. 
|
| 13. | Daniyam CA, Agaba PA, Agaba E. Acceptability of voluntary counselling and testing among medical students in Jos, Nigeria. J Infect Dev Ctries 2010;4:357-61. 
|
| 14. | Ntalaka R. Baruga F. Sources of information for clients seeking HIV counseling and testing services at AIDS Information Centre (AIC) Uganda 2004-2008. Health and Biosciences. AIDS Information Centre - Uganda Kampala, Uganda. World Library and Information Congress: 76 th IFLA General Conference and Assembly, 10-15 August 2010, Gothenburg, Sweden. Available from: http://www.ifla.org/en/ifla76. Last accessed on 2014 Feb 14. 
|
| 15. | Denison JA, Lungu N, Dunnett-Dagg WA, McCauley A, Sweat MD. Social Relationships and Adolescents' HIV Counseling and Testing Decisions in Zambia, Horizons Research Summary. Washington, DC: Population Council; 2006. 
|
| 16. | Oppong Asante K. HIV/AIDS knowledge and uptake of HIV counselling and testing among undergraduate private university students in Accra, Ghana. Reprod Health 2013;10:17. 
|
| 17. | Sebudde S, Nangedo F. Voluntary counselling and testing services: Breaking resistance to access and utilization among the youths in Rakai district of Uganda. Educ Res Rev 2009;4:490-7. 
|
| 18. | Charles MP, Kweka EJ, Mahande AM, Barongo LR, Shekalaghe S, Nkya HM, et al. Evaluation of uptake and attitude to voluntary counseling and testing among health care professional students in Kilimanjaro region, Tanzania. BMC Public Health 2009;9:128. 
|
| 19. | Abebe A, Mitikie G. Perception of students towards voluntary HIV counselling and testing using health belief model in Butajira, SNNPR. Ethiop J Health Dev 2009;23:148-52. 
|
| 20. | Hoffmann O, Boler T, Dick B. Achieving the global goals on HIV among young people most at risk in developing countries: Young sex workers, injecting drug users and men who have sex with men. World Health Organ Tech Rep Ser 2006;938:287-315. 
|
| 21. | Monasch R, Mahy M. Young people: The centre of the HIV epidemic. World Health Organ Tech Rep Ser 2006;938:15-41. 
|
| 22. | Iyaniwura CA, Oloyede O. HIV testing among youths in a Nigerian local population. West Afr J Med 2006;25:27-31. 
|
| 23. | Aniebue PN, Aniebue UU. Voluntary counseling and willingness to screen among Nigerian long distance truck drivers. Niger Med J 2011;52:49-54. 
[PUBMED]  |
| 24. | Oshi SN, Ezugwu FO, Oshi DC, Dimkpa U, Korie FC, Okperi BO. Does self-perception of risk of HIV infection make the youth to reduce risky behaviour and seek voluntary counselling and testing services? A case study of Nigerian youth. J Soc Sci 2007;14:195-203. 
|
| 25. | Iliyasu Z, Abubakar IS, Kabir M, Aliyu MH. Knowledge of HIV/AIDS and attitude towards voluntary counseling and testing among adults. J Natl Med Assoc 2006;98:1917-22. 
|
| 26. | Koku EF. Desire for, and uptake of HIV tests by Ghanaian women: The relevance of community level stigma. J Community Health 2011;36:289-99. 
|
| 27. | Koku EF. Stigma, sexual risk and desire for HIV tests in Ghana. Sex Health 2011;8:110-9. 
|
| 28. | Payne NS, Beckwith CG, Davis M, Flanigan T, Simmons EM, Crockett K, et al. Acceptance of HIV testing among African-American college students at a historically black university in the South. J Natl Med Assoc 2006;98:1912-6. 
|
| 29. | Norman LR, Gebre Y. Prevalence and correlates of HIV testing: An analysis of university students in Jamaica. MedGenMed 2005;7:70. 
|
[Figure 1]
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
|