|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2015 | Volume
: 1
| Issue : 2 | Page : 46-50 |
|
Developing Nurse's Educational Program Regarding Pain Management of Cancerous Patient: Does Health Belief Model Useful?
Hossein Shahnazi1, Gholamreza Sharifirad2
1 Department of Health Education and Promotion, School of Public Health, Isfahan University of Medical Sciences, Isfahan, Iran
2 Department of Public Health, School of Health, Qom University of Medical Sciences, Qom, Iran
| Date of Web Publication | 22-Sep-2015 |
Correspondence Address:
Dr. Gholamreza Sharifirad
Department of Public Health, School of Health, Qom University of Medical
Sciences, Qom, Iran.
Iran
 Source of Support: None, Conflict of Interest: None  | Check |
 
Background: Some of reasons such as fear from side effects of anti-pain drugs, fear from decreasing concentration in disease treatment, and believe that pain unseparatable section from cancer, resulted that treatment staff such as nurses who are patients main caregivers do not have suitable approach toward cancer pain management. This study aims to determine application of Health Belief Model (HBM) in nurses education regarding pain management of cancerous patients. Materials and Methods: In this prospective quasi-experimental study, among educational hospitals of Isfahan University of Medical Sciences two eligible hospitals (Al-Zahra and Seyed Al-Shohada) have considered to do study. Data gathering tool was HBM base questionnaire which after confirmation of validity and reliability has completed by two groups. Two and six months after educational intervention, questionnaire completed by two groups again. Resulted data entered to SPSS version 18, (SPSS Inc., Chicago, IL, USA) software and analysed by related statistical tests at significant level of P < 0.05. Results: Finding showed that, the mean scores HBM constructs hadn't have significant difference between two groups before educational intervention (P>0.05). Measuring the mean scores 2 and 6 months after educational intervention showed significant differences between two groups in case of mentioned variables (P< 0.001). Repeated measure ANOVA test indicated that 2 and 6 months after education, the mean scores of HBM constructs have significantly increased in the intervention group (P< 0.001). Conclusion: The results of this study indicate the effectiveness of educational intervention based on HBM in increasing knowledge and attitude of nurses regarding pain management in cancerous patient. Since, the palliative care is a new topic, doing similar studies with patient and cure staff target groups will be promoted pain management approach in the country. Keywords: Education, Health Belief Model, nurse, pain management
How to cite this article:
Shahnazi H, Sharifirad G. Developing Nurse's Educational Program Regarding Pain Management of Cancerous Patient: Does Health Belief Model Useful?. J Hum Health 2015;1:46-50 |
How to cite this URL:
Shahnazi H, Sharifirad G. Developing Nurse's Educational Program Regarding Pain Management of Cancerous Patient: Does Health Belief Model Useful?. J Hum Health [serial online] 2015 [cited 2018 Aug 21];1:46-50. Available from: http://www.jhhjournal.org/text.asp?2015/1/2/46/165912 |
| Introduction | |  |
Over the past two decades, it has shown that there are many problems and shortcomings in the treatment of cancer symptoms such as patient's pain. Patient's quality of life can be affected by pain.[1] The acute or chronic pain prevalence in cancer patients is high, in this way that 30%, 50–70% and 60–80% of them are newly diagnosed, being treated and advanced cancer, respectively.[2] It has totally estimated that 60% of cancer patients at least in the course of their disease will experience some degree of pain that in many cases, appropriate action is not taken to control pain.[3],[4] Some studies showed that either cancer pain of large number of patients is not sufficiently controlled or receive tranquilizer slowly and irregularly that cannot be effective in controlling pain.[5] Modern pain theory considered pain as a complex process that resulted by the exchange emotional, cognitive and motivational components.[6] In the most patients (over 90%), pain can be significantly controlled if proper treatment of pain occur under existing protocols.[7] Palliative treatment failure in cancer patients can be formed by several factors that are related to patients and treatment personnel (including social-psychological factors) and low or non-regular use of tranquilizers (including misinformation about tranquilizers).[8] In the most cases, failure to pain control treatments is contributed to treatment personnel perceived barriers in terms of drugs and treatment process.[9] Medical staff including nurses that are main caregivers may not have appropriate approach in controlling pain of cancer patients because of fear of tranquilizers side effects, afraid of losing focus on the treatment and the belief that pain is an inseparable part of cancer.[10] There are some cognitive, emotional and sensory barriers of management of cancer pain.[11] Results of numerous surveys presented that there are two cognitive barriers related to pain management that are included:
- Concerns related to the use of tranquilizers (fear of addiction to drugs)
- False beliefs about pain control (the belief that cancer pain will not be relieved).
Other cognitive factors has diagnosed in different studies about pain management including patient concerns toward other people reactions about her complaints of pain and lack of confidence in health system.[12] Emotional changes of cancer patient that prevent appropriate analgesic treatment are defined as emotional barriers. Despite the fact that cancer patients who are suffering pain have involved in high prevalence of mood disorders, attention to emotional changes that play an inhibitory role in palliative treatments has not been considered, significantly. The relationship between cognitive and emotional factors in cancer patients has been described in many different ways. Depression, negative mood and stress are interconnected with false beliefs regarding pain management therapies and concerns about the use of pain medications.[13] Another concern which makes nurses do not fully comply with pain management is the fear of adverse drugs that is a sensory barrier of pain control treatment.[14] An experimental investigation has shown that 20–75% of cancer patients and about 68% of oncology nurses are worried about the side effects of pain medications, therefore; simultaneously while reducing perceived barriers, increase the perceived benefits associated with the prescription and medication adherence to control patient pain by nurses is very important.[15] Perceived self-efficacy of nurses in pain management in cancer patients is not well studied. Of course, some studies were examined perceived behavioural control very generally and vaguely. For example, Yates and colleagues study showed that educational intervention through interview with nurse causes increase nurses' perceived behavioral control related to pain management.[16] But none of the studies, have not provided detailed information about the role of this agent in pain management. Several studies also has not been pointed to the role of nurses perceived threat in pain management of cancer patients, only some of studies, including the study of Tsai et al. and Bostroum and colleagues. have pointed out perceived barriers (not separately).[17],[18] So far, several approaches have been used in medicine to control pain in patients with cancer. Despite these approaches, it can be said that very few attempts using educational approaches have been used to control pain.[19],[20],[21] However, educational plans for medical staff, especially nurses, to support them to comply with perceived barriers of tranquilizers (such as fear of addiction) seems basically vital. Perceived self-efficacy of nurses about prescribing tranquilizers can be promoted using educational and systematic medical approaches. As inappropriate attitudes of nurses are leading causes of the palliative treatment failure in patients with cancer, it can be concluded that implementing more successful treatments of pain management can be achieved through decrease barriers and perceived threats and increase benefits and self-efficacy using targeted training programs. As aforementioned, Health Belief Model (HBM) constructs were respected, then; this survey was aimed at educational intervention on nurses in improving pain management of cancer patients based on HBM.
| Materials and Methods | |  |
This survey was a quasi-experimental study using pre- and post-test with randomized control group. The study populations were nurses working in two hospitals of Isfahan named Seyed Al-Shohada and Al-Zahra that were main referral and treatment centre of cancer patients in Isfahan. Multi-stage sampling was used, in this way that atfirst, case and control group were selected randomly from Al-Zahra and Seyed Al-Shohada Hospital, respectively. Then, 44 samples were considered for each hospital, in total, 88 individuals were picked out to survey.
Data gathering tool
Data were collected using a questionnaire included 54 questions that was designed in 2 parts:First section was included age, gender, marital status, education, job experience, employment and economic status.
Second part was about HBM constructs including perceived benefits (5 questions), perceived barriers (5 items), perceived threat (5 items), self-efficacy (5 items) and cues to action (4 items). Aforementioned questions were formed based on 5 point Likert scale and ranged 0 (strongly disagree) and 4 (strongly agree), for negative questions, reversed scoring was done, as well.
Validity and reliability
Content validity was used to test scientific validity of the questionnaire. Questionnaire was designed by literature review and then, was revised by health education and anaesthesiology scholars. To evaluate reliability, Cronbach's alpha coefficient was used that was 0.85 for HBM constructs.
Intervention
Three educational sessions (each session 90 min) were held through lecture method using slides and inquiry for nurses of case group. Trainer was specialized in anaesthesiology and pain management. Thefirst session contents were including general topics relating to classification of pain, the pain spread and importance of pain management in cancer patients. In second session, barriers to successful pain relief, principles of pain assessment and history-taking and how to communicate effectively with patients suffering from cancer were described for participants. Amount, how and when use pain-relieving medication, the patient's addiction to narcotic medications and drug side effects were explained to the audience the third one. Nurses were asked to present their questions and implication using phone or verbal, on completion of training sessions, in brief. Two and 6 months after training sessions to review the research variables, questionnaire was distributed among the intervention and compare group, again. It must be noted that during the study period, compare group was not provided by any training or other intervention.
Data analysis
HBM constructs (perceived benefits, perceived barriers, perceived threat, perceived self-efficacy and cues to action) questions were scored based on 5 point Likert scale, 0 and 4 score was respected for items including completely disagree and completely agree, respectively. For negative questions, reversed scoring was done. To compare the mean score, repeated measure ANOVA was used. To analysis same aforementioned variable between the intervention and comparison groups after intervention, independent t-test was implemented. Chi-square and Mann–Whitney test was also used to investigation demographic variables.
| Results | |  |
Results presented that the vast majority of nurses in the two groups were woman, married and had a bachelor's degree in nursing [Table 1].
Independent t-test showed that the mean score of HBM constructs (perceived benefits, perceived barriers, perceived threat and perceived self-efficacy) in nursing; before education was not significant between the two groups, but the average score were significantly greater in the intervention group than the control group 2 and 6 months after training. Repeated measure ANOVA showed that the mean score of the listed constructs in the control group, 2 and 6 months after training, was not significantly different. On the other hand, aforementioned test was also maintained that in the case group, the mean scores of perceived benefits before, 2 and 6 months after training was significant [Table 2].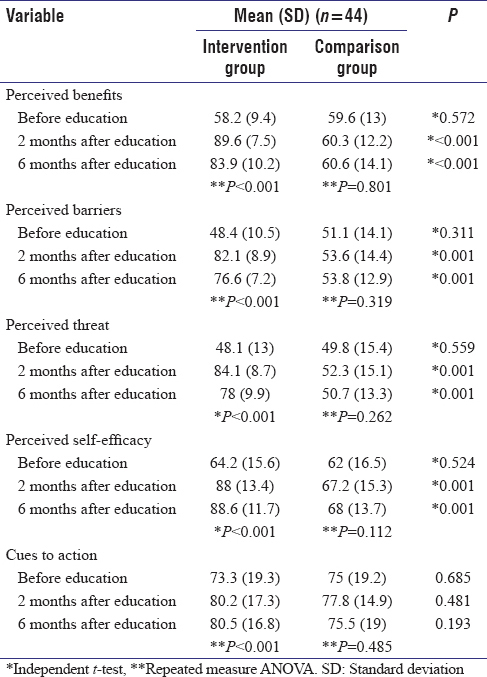 | Table 2: The mean score of Health Belief Model constructs among nurses about pain control in cancer patients
Click here to view |
Independent t-test showed that the mean score of cues to action of nurses before training was not different before 2 and 6 months after education. Repeated measure ANOVA showed that the mean score of cues to action in the control group, before 2 and 6 months after training, was not different, while; mentioned test delineated that there was significant statistical difference before 2 and 6 months after training in the case group [Table 2].
| Discussion | |  |
According to average scores of perceived benefits, findings showed that there was not significant relationship between the two groups, before intervention, while; 2 months after education intervention in the intervention group, the mean score of perceived benefits was promoted from 58.2 to 89.6. Meanwhile scores of perceived benefits in the comparison group was not changed significantly. Yates et al. survey also showed that nurses' perceived benefits of the intervention group increased after training, Whereas; in the comparison group, a significant difference between the perceived benefits were not observed before and after training.[16] In a study conducted by Lovell et al. on cancer patients, the results showed that after educational programs through lectures, videos training, manuals, perceived benefits of intervention group in terms of regular use of analgesics was significantly increased compared to the comparison group.[22] Despite of fall compared to 2 months after education, results of our study presented that, 6 months after intervention, perceived benefit score was significant compared to before training. In fact, it can be said that over time was lead to decreased nurses' perceived benefits, despite of this drop, it was still different with before education intervention scores. In the same investigation, Zhang et al. study reported that nurse' perceived benefits regarding pain control was enhanced meaningfully, 1-month after intervention. In contrast, in the comparison group, a significant difference was not observed between nurses' perceived benefits before and 1-month after training. This increase was also existed in after 3 months education measurement that was caused by training sessions during investigation.[23] However, according to increase of perceived benefits scores, it can be concluded that nurses perception after intervention were promoted compared to before intervention regarding benefits of pain management process. This augmentation in nurses will elevate motivation and willingness of them to undertake appropriate actions to manage cancer pain.
Based on our results, the perceived barriers score of two groups before the intervention was not different significantly, whereas 2 months after education, perceived barriers score of intervention group was augmented from 48.4 to 82.1, while the comparison group was not reported the same statistically significant increment. Six months after training intervention, perceived barriers score in the intervention group compared to the 2 months after training was partly diminished, although there was still a significant difference before pre-training. Several studies suggest a positive impact of education in increasing the perceived barriers score of different groups of nurses in pain management of cancer. For example, in Lovell et al. study, it was determined that intervention caused increases the perceived barriers score of medical and educational staff in cancer pain management using attendance and non-attendance training session.[22] Vallerand et al. have conducted an educational intervention on 202 nurses using lecture and group discussion, results showed that after the intervention; perceived barriers scores were immediately elevated. Although, over time, mentioned score has declined, as 1-year after training, perceived barriers score after education compared to before was not significantly different [24] that this finding is inconsistent with the results of our study, despite the drop compared to 2 months after training, in our study, perceived barriers scores 6 months after training were different compared to before education. This difference in our investigation may be resulted by offering an educational booklet pain control to nurses of intervention group. Of course, many studies have accentuated on the positive impact of education on sustainable changes of nurses' perceived barriers regarding cancer pain management. For example, Rand and et al. study was conducted on 144 nurses showed that 6 months after education, nurses' perceived barriers score was still higher than before training and showed significant difference.[25] According to our study, before intervention, perceived threat score was not statistically different between the two groups, however; it was promoted from 48.1 to 84.1 after educational intervention in intervention group. While, there was no evidence of increase in comparison group. Perceived threat of experimental group nurses in 6 months after the training than 2 months after intervention was reduced, partly; on the other hand, this construct score is still different before training. Lovell et al. study showed that different training session for medical staff caused increase of perceived threat score.[22] In another survey done by Vallerand et al., the results showed that after conducting educational programs for nurses, immediately, the perceived threat score of pain management was increased, aforementioned score was gradually inclined, as 1-year after intervention, it was not different compared to before that.[24] This finding is not in relevance with our study results; its reason seems to be look like what presented as the perceived barrier that is keeping education using training booklet that lead to increased model constructs in our investigation. Many studies have also indicated the positive effect of education on sustainability of perceived threat score. For instance, Rand et al. study results showed that nurses perceived threat scores was ranged acceptable 6 months after education, and it was also meaningful compared before training.[25] The results of the Zhang et al. study showed that intervention program increases the perceived threat score of nurses about pain management of cancer patients and this score was measured in 1 and 6 months after intervention that was significantly different in 2 times.[23]
The results showed that perceived self-efficacy in the treatment group is 64.2 and 62 in the comparison group, before intervention that indicated the lack of significant differences between the two groups before intervention. However, intervention has caused augmented self-efficacy scores in the intervention group from 64.2 (before intervention) and reaches 88 (2 months after training) in intervention group, although this score was not differ in comparison group. Six months after education, group self-efficacy score reached 88.6 in intervention group, while; the same score reached 68 without a significant difference in comparison one. Wilson survey found that intervention not only impact on knowledge and attitudes of nurses but also increase their perceived self-efficacy in cancer pain management process, moreover; this increased self-efficacy) was conserved over time (4 months after the intervention).[26] In a study implemented in Australia by Yates et al., self-efficacy was explored as an enabling factor of pain control that findings presented that nurses self-efficacy was low before intervention, but after intervention that was increased.[16]
[Table 2] indicated that cues to action were not different between the two groups before intervention. Two months after training, cues to action score was reached from 73.3 to 80.2 in intervention group, while; this increase was not existed in comparison group. Furthermore; cues to action score of intervention group was 80.5 in 6 months after training, but, in comparison group, 6 months after intervention, constructs scores were not different (before, 2 and 6 months after training).
It seems likely that increase score of intervention group caused by introducing booklets and several websites for nurses regarding palliative medicine and providing information about pain management. This is why that 2 months after training session, around 90% of intervention participants considered that booklets and training session had plays an important role in escalating knowledge and attitudes of nurses about pain control. In a study done by Fax et al. regarding pain management, results showed that nurses mentioned that continuous and regular training to increase their knowledge and practice in the field of pain management was theirfirst priority.[27] Jacobsen et al. in a study named related barriers of pain management in cancer patients said that the most important barrier for appropriate managing of pain is lack of training session from nurse's point of view,[28] Ward et al. survey also showed that the most determining barrier is nurse's disability in making communication with patients properly that caused by lack of workshops and training seminars.[29]
| Conclusion | |  |
Our study findings indicate that using HBM seems to be beneficial to promote nurses attitude in terms of pain control of cancer patients. Since, current survey is one of thefirst educational intervention studies in this field, it is recommended that similar planned and implemented explorations to appropriate education approaches for promoting medical staff performance will achieved.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| References | |  |
| 1. | Otto SE. Oncology nursing. Philadelphia: Mosby Press 2001.  |
| 2. | acobsen R, Liubarskiene Z, Møldrup C, Christrup L, Sjøgren P, Samsanaviciene J. Barriers to cancer pain management: A review of empirical research. Medicina (Kaunas) 2009;45:427-33.  |
| 3. | Bhaskar AK. Interventional management of cancer pain. Curr Opin Support Palliat Care 2012;6:1-9.  |
| 4. | Yu Yl, Zhou J, Li Q, Bian F, Cao CS, Jin X, et al. The preliminary application of assessment system for cancer pain management Eur Rev Med Pharmacol Sci 2015;19:1164-9.  |
| 5. | Borneman T, Koczywas M, Sun VC, Piper BF, Uman G, Ferrell B. Reducing patient barriers to pain and fatigue management. J Pain Symptom Manage 2010;39:486-501.  |
| 6. | Beuken-van Everdingen MHJ, Rijke JM, Kessels AG, Schouten HC, Kleef Mv, Patijn J. Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Ann Oncol 2007;18:1437-49.  |
| 7. | Corner J. Bailey C. Cancer nursing care in content. Blackwell science: London 2001.  |
| 8. | Mann E, Carr E. Pain management: Essential clinicical skill for nurses. Blackwell: UK; 2006.  |
| 9. | Raj PP. Practical management of pain. rd ed. London: Mosby 2000.  |
| 10. | Shahnazi H, Saryazdi H, Sharifirad G, Hasanzadeh A, Charkazi A, Moodi M. The survey of nurse's knowledge and attitude toward cancer pain management: Application of Health Belief Model. J Educ Health Promot 2012;1:15.  |
| 11. | Prandi C, Garrino L, Mastromarino P, Torino F, Vellone E, Peruselli C, et al. Barriers in the management of cancer-related pain and strategies to overcome them: Findings of a qualitative research involving physicians and nurses in Italy. Ann Ist Super Sanita 2015;51:71-8.  [ PUBMED] |
| 12. | Scharff L, Urk DC, Arcus DA. The Relationship of Locus of Control and Psychosocial-Behavioral Response in Chronic Headache. Headache: The Journal of Head and Face Pain 2005;35:527-533.  |
| 13. | Munaf M, Trim J. Chronic pain: A handbook for nursing. Butterworth Heinermann: Oxford 2000.  |
| 14. | Salehi Sh, Akhundzadeh K, Hosseini A. Critical Thinking and Decision Making in Nursing. Isfahan Medical University: Isfahan 2006.  |
| 15. | Akhundzadeh K, Khorrami Rad A, Heidari S, Abedini Z. The relationship between pain coping strategies and pain intensity in chronic pain patient. The 3 rd International Congress of Psychosomatic Medicine Psychosomatic Aspect of Pain & Pain Management. Isfahan 2011.  |
| 16. | Yates P, Edwards H, Nash R, Aranda S, Purdie D, Najman J, et al. A randomized controlled trial of a nurse-administered educational intervention for improving cancer pain management in ambulatory settings. Patient Educ Couns 2004;53:227-37.  |
| 17. | Tsai FC, Tsai YF, Chien CC, Lin CC. Emergency nurses' knowledge of perceived barriers in pain management in Taiwan. J C  |
| 18. | Boström B, Sandh M, Lundberg D, Fridlund B. Cancer-related pain in palliative care: Patients' perceptions of pain management. J Adv Nurs 2004;45:410-9.  |
| 19. | Ferel BR, Ferel BB. Pain in aging. Translated by: Sharifi M and Shahrir N. 1th ed. Tehran: Iran pain association 2005.  |
| 20. | Breivik H, Cherny N, Collett B, Conno F, Filbet M, Foubert AJ, et al. Cancer-related pain: A pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol, 2009;20:1420-33.  |
| 21. | NCCN: National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Adult Cancer Pain 2007. Available at: www.nccn.org. [Last accessed on 2011 Jul 14].  |
| 22. | Lovell MR, Forder PM, Stockler MR, Butow P, Briganti EM, Chye R et al. A randomized controlled trial of a standardized educational intervention for patients with cancer pain. J Pain Symptom Manage 2010;40:49-59.  |
| 23. | Zhang CH, Hsu L, Zou BR, Li JF, Wang HY, Huang J. Effects of a pain education program on nurses' pain knowledge, attitudes and pain assessment practices in China. J Pain Symptom Manage 2008;36:616-27.  |
| 24. | Vallerand AH, Musto S, Polomano RC. Nursing's role in cancer pain management. Curr Pain Headache Rep 2011;15:250-62.  |
| 25. | Rond M, de Wit R, van Dam F. The implementation of a Pain Monitoring Programme for nurses in daily clinical practice: Results of a follow-up study in five hospitals. J Adv Nurs 2001;35:590-8.  |
| 26. | Wilson B. Nurses' knowledge of pain. J Clin Nurs. 2007;16:1012-20.  |
| 27. | Fox CR. What health care providers know and need to know about palliative care. J Allied Health 2007; 36:209-15.  |
| 28. | Jacobsen R, Liubarskiene Z, Møldrup C, Christrup L, Sjøgren P, Samsanaviciene J. Barriers to cancer pain management: A review of empirical research. Medicina (Kaunas) 2009;45:427-33.  |
| 29. | Ward S, Donovan H, Gunnarsdottir S, Serlin RC, Shapiro GR, Hughes S. A randomized trial of a representational intervention to decrease cancer pain (RIDcancerPain). Health Psychol 2008;27:59-67.  |
[Table 1], [Table 2]
|