|
 
 |
| REVIEW ARTICLE |
|
| Year : 2013 | Volume
: 1
| Issue : 3 | Page : 89-94 |
|
Ergonomics, posture and exercises - Painfree, prolong orthodontic career
Avesh Sachan, Vinay Kumar Verma, Sujit Panda, Karuna Singh
Department of Orthodontics, Rama Dental College, Hospital and Research centre, Kanpur, Uttar Pradesh, India
| Date of Web Publication | 20-Dec-2013 |
Correspondence Address:
Avesh Sachan
Department of Orthodontics, Rama Dental College, Hospital and Research Centre, Kanpur - 208 024, Uttar Pradesh
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/2321-3825.123318

Orthodontists are exposed to several occupational hazards. Back and neck pain arising due to improper posture is very common in this community. The nature of work entails abnormal flexion of the lumber spine and subsequent loading on the inter-vertebral disks or extra tension in the spinous ligaments causing musculoskeletal disorders. Neck and shoulder, lower back, hand and wrist are the most commonly involved regions. Obtain an accurate diagnosis from a qualified healthcare provider. Early intervention is the key. Treatment may range from pain relief medications and rest to surgery and ergonomic interventions at work place and home. The current paper discusses etiology of musculoskeletal disorders (MSD) preventive measures which can be incorporated to ensure a trouble free professional career. Keywords: Ergonomics, exercises, musculoskeletal disorders, orthodontics, posture
How to cite this article:
Sachan A, Verma VK, Panda S, Singh K. Ergonomics, posture and exercises - Painfree, prolong orthodontic career. J Orthod Res 2013;1:89-94 |
How to cite this URL:
Sachan A, Verma VK, Panda S, Singh K. Ergonomics, posture and exercises - Painfree, prolong orthodontic career. J Orthod Res [serial online] 2013 [cited 2017 Jan 11];1:89-94. Available from: http://www.jorthodr.org/text.asp?2013/1/3/89/123318 |
| Introduction | |  |
Orthodontic professionals often develop musculoskeletal problems, which are related to suboptimal work-environment ergonomics that might be responsible for improper sitting postures and movements causing unnecessary musculoskeletal loading, discomfort, and fatigue. Insufficient or inappropriate equipment, inappropriate work-area design, direct injuries, repetitive movements from working with instruments, or sitting for extended times with a flexed and twisted back are contributing factors to neck and low-back ailments. [1],[2],[3],[4]
Musculoskeletal disorders, including repetitive motion injuries, result in painful work, lost work days, and in extreme cases, disability resulting in forced retirement. Musculoskeletal disorders are not highly predictable in any single person. Individual susceptibility or predisposition and personal risk factors such as past injury and underlying medical conditions contribute to the risk for musculoskeletal disorders. Every Orthodontic professional can take steps to reduce their risk of sustaining musculoskeletal disorders. The limited research in the orthodontic literature showed increased risks for developing these types of musculoskeletal disorders (MSDs). [4],[5],[6],[7]
Etiology
The dental chair position and the operator's stool position and orientation relative to that of the patient, combined with the orthodontist's effort to maintain visibility of the oral environment, result in awkward positions over long periods of time; these in turn result in back problems. [8] The causes of MSDs include equipment that is poorly designed or improperly used; the use of various types of force by parts of the body; awkward posture; repetition; the use of vibrating tools; and other factors, including some that are not work related (such as obesity, arthritis, autoimmune disorders, and smoking). Although there are known risk factors for MSDs, it is difficult to attribute a given disorder to a specific risk factor.
Effects of MSDs
Musculoskeletal problems happening outside the work environment can either worsen with work or make work difficult. [9] Various structures can be affected - muscles, ligaments, tendons, nerves, joints, and supporting structures (inter-vertebral disks). A number of disorders are included under this category: Upper and lower back pain, herniated disk, neck pain with or without cervical root problems, carpal tunnel syndrome, tendinopathies, shoulder pain, rotator cuff tendinopathies, and repetitive strain injuries. Upper and lower back pain and inter-vertebral disk diseases (acute or chronic) are responsible for absence inOrthodontic practice. The symptoms include low back pain, stiffness, and sciatica with neurological features such as tingling, paresthesia, and muscle weakness. This can result in chronic pain (mechanical low back pain) and difficulty in performing various tasks such as bending, lifting, and driving long distances. [9]
Neck problems are associated with a similar etiology, especially awkward body and head posture, which are often required for direct vision into the mouth (commonly in lingual orthodontic practice). The introduction of indirect bonding and magnifying loupes is probably the only development over the years that helps orthodontists keep a more neutral or balanced posture. [10] The symptoms include intermittent neck pain, often radiating to the shoulders (with stiffness); headaches; tingling, or pins and needles down the arms and fingers, resulting in weakness; and clumsiness. In more severe situations, disk prolapse can occur and, later, degeneration (cervical spondylosis). Because the shoulder muscles are innervated by the brachial plexus, there is also strain on the shoulder muscles (pain, weakness) that will complicate the situation.
Tendonitis usually causes pain and discomfort that worsens with movements. Tears also cause weakness in abduction; old and degenerative tears cause impingement in the subacromial region (arc pain in abduction, eased beyond 90-100°). Although direct injuries are rare in dentistry, eccentric loading of the tendon or the muscle and working with the arm in an abducted position for a long time is common. Cervical spondylosis can cause further muscle weakness, which will give rise to more pain exacerbated by radiating pain from nerve root irritation. [11]
Carpal tunnel syndrome (CTS) is the most common nerve entrapment syndrome. It involves the entrapment of the median nerve at the level of the wrist. In the work environment, CTS results from rapid, repetitive, and daily use of the hand and fingers for many hours at a time. The problem is compounded when working with a bent wrist, exerting force, working with vibratory tools, and in cold environments. This can result in tingling in the thumb, index, middle, and half of the ring finger; night pain; and pain when handling tools. [12]
Tendinopathies are inflammations of the tendons or the tendon sheaths. The affected area is swollen and sensitive to touch, whereas pain is elicited with certain movements such as grasping and pinching. Practically, this translates to difficulty in handling instruments because it affects grasping and rotational and lateral bending of the wrist.
Good Ergonomics
The practice of good ergonomics is a significant strategy for the prevention of MSDs. There are several recommendations for improved ergonomics specific to dentistry [Table 1]. Ergonomics in orthodontics is the study of the relationship of humans or clinicians to their working environment and the development of methods, tools, and equipment to improve working conditions, increase efficiency, and reduce injury. In realistic terms, this means selecting and appropriately using equipment that allows for comfortable postures, using instruments that minimize gripping force and vibration, positioning the patient to allow maximum access and visibility with minimal bending and leaning, maintaining good general health, and recognizing and addressing the warning signals for MSDs early in their progress. [13],[14],[15]
Dental Equipment and Dental Instruments
Items attached to the dental cart or delivery system may provide resistance because of weight, balance, or the pull of cords. Some potential solutions to these issues include
- Selecting high-speed suction handles that are not awkward to hold and activate.
- Purchasing lightweight instruments that have a balanced feel.
- Installing cords that are long enough to allow the operator to manipulate into a comfortable position yet not so long as to add unnecessary weight.
- Any other available features that make the equipment more comfortable to operate.
Some useful strategies for reducing the risk of repetitive strain injuries are to use instruments with larger-diameter handles that require less gripping force; select instruments that are textured to allow easier gripping; avoid awkward wrist positions; take small rest breaks when performing repetitive tasks; and use mechanical scaling devices where appropriate to reduce the need to exert force when root planning and scaling. The use of mechanical scaling devices will also decrease the duration of the stressful activity. [16]
Posture and Patient Positioning
Orthodontists often work using static body positions, such as extended elbows, for prolonged periods of time. This requires the retraction of at least 50% of the body's muscles to allow the body to remain motionless while resisting gravity. This static loading of the muscles causes greater fatigue than moving forces, and may lead to MSDs in addition to chronic back, neck, or shoulder pain. [17],[18] Posture and patient positioning are two important tools in preventing the use of static body positions. Operator and assistant posture and patient positioning go hand in hand as a strategy for improving chair-side ergonomics. Good operator position consists of the following elements:
- Head and neck relatively erect with the focal distance 13 inches to 18 inches from the patient's face.
- Operator loupes adjusted to focus on the working field at a distance of 13 inches to 18 inches.
- Shoulders should be parallel to the floor.
- The back should be supported at approximately a 100° to 110° angle to the stool seat.
- Elbows should be at the sides at the level of the patient's mouth.
- Forearms should generally be parallel to the floor.
- Knees should be slightly below hip level.
- The left leg should be extended under the patient's chair with the foot flat on the floor while the right foot operates the rheostat (reverse for a left-handed operator).
Ideal position to place the patient, while working on the maxillary arch is with the chair fully supine. With the patient in this position, the operator can use the mirror for indirect vision without bending, leaning, or stretching. For the mandibular arch, elevate the back of the patient's chair between 5 degrees and 30°. When working on either arch lower the patient's chair to just above the operator's leg.
Four-Handed Orthodontics
Working with an assistant not only increases the efficiency of the procedure, but also allows the Orthodontist to maintain posture and avoid awkward positions. Effective four-handed techniques require the active participation of both the Orthodontist and the assistant. The Orthodontist must communicate adequately to the assistant, the sequence of instruments, so that the appointment progresses smoothly. Instrument transfers should occur in a designated transfer zone, ensuring that both the assistant and the Orthodontist understand where and how instruments will be passed, reducing the need for unnecessary movement while also increasing efficiency and reducing the risk of accidentally dropping the instrument.
The Orthodontist Chair-Saddle Seat
If a seat does not allow the pelvis to maintain its neutral position during work, it will cause spinal stress. A good sitting posture maintains the spinal curves normally present in the erect standing position. The saddle seat has radically changed the seated position and it can actually help and give back support to pain-free work. [19] Thighs of Orthodontist should be parallel with the floor and the feet flat on floor. Position the chair close to the patient (to minimize forward bending). Orthodontist's legs should be directly under the patient's chair. The saddle seat maintains the shape of the spine in a natural "S" shape rather than strained seating positions [Figure 1].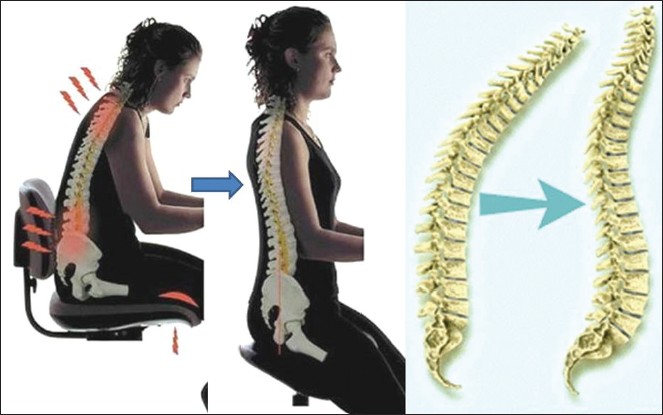 | Figure 1: Saddle seat maintains the shape of the spine in a natural "S" shape
Click here to view |
| Exercises | |  |
Hip Bridge Exercise
How to do it - Lie on your back, feet flat and hip-width apart, arms relaxed, and knees bent. Squeeze your buttocks as you lift your hips, creating a straight line from the knees to the shoulders. Hold for a slow count of five, and then lower slowly [Figure 2]. Build up to 10 to 20 repetitions.
What it does - This move counteracts the effects of too much chair time, which puts excessive pressure on the spine. It stretches the hip flexors and strengthens the muscles that stabilize the spine, including those of the lower back, the gluteus, and the large stabilizing abdominal muscles.
Strengthening the Neck Muscles
These exercises strengthen the neck musculature. This includes cervical paraspinal muscles and suboccipital muscles. These exercises are called isometric exercises. Isometric exercise is a type of exercise involving the static contraction of a muscle without any visible movement in the angle of the joint. In simple terms, this means that in these exercises the length of the muscle does not change. [20]
- Press your palms against your forehead and push against each other, resisting motion. Hold this position for 5 seconds and repeat this exercise 3 times.
- With this next cervical strengthening exercise place your hand against the side of your head. Try to bring to your ear your shoulder, resisting the motion. Repeat this exercise on the other side. Hold each position for 5 seconds and when finished relax slowly.
- Cup both hands against the back of your head. Attempt to push your head back, resisting the motion. Hold this position for 5 seconds, and when finished relax slowly.
- In the final cervical strengthening exercise, put your right hand against the right temple. Attempt to turn your chin to your right shoulder, resisting the motion. Repeat this on the left side. Hold for 5 seconds, and then relax slowly. Do these neck exercises 3 times [Figure 3].
Wrist Strengthening Exercises
- Support your forearm on a table. Holding putty in your hand. Bend your fingers pressing deeply into a sponge/ball of wool. Then straighten fingers as much as possible.
- Wrist in mid-position. Put the other hand over the back of the hand to be exercised. Try to lift the back of the hand up while preventing movement with your other hand.
- Wrist in mid-position. Put the other hand under the hand to be exercised. Try to bend the hand down while preventing movement with your other hand [Figure 4]. [21]
Fingers and Thumbs Strengthening Exercises
Like with exercising any other part of your body, warming up of fingers and thumbs is important and should not be overlooked.
- Bend each finger back until you feel a slight stretching. Then bend each finger forward. Note that this should not be done to the point of pain.
- Place one hand flat on a table in front of you, palm down. Lift and lower each finger one by one.
- Keep your fingers flat on the table. Spread them apart as far as you can, then bring them as close together as possible.
- Alternatively, crumple up a piece of paper or cloth so it fits comfortably in your grasp. Squeeze the object as hard as you can, then relax.
- Touch your thumb to each of your fingertips. Make sure that each touch makes an ''O'' shape.
- Bend the end joint of your finger, keeping all other joints straight. Hold for a moment, then straighten.
- Keeping your fist joints straight, bring your fingers in as tightly as you can. Then, open your fingers completely.
- Bring your thumb over your palm as far as possible. Stretch it away from your palm as far as possible.
- Slap your pinkie, ring finger, and middle finger against your palm.
- Hold a Newspaper between your thumb and forefinger. Hold it out from you at arm's length. Using only your fingers, crumple the paper into a ball [Figure 5].
| Conclusion | |  |
Many factors influence the risk of MSDs among dental workers. A comprehensive approach to prevention includes education, assessment of risk factors, proper equipment and instruments, posture, and personal habits such as exercise. In the dental office, a team approach including the use of four-handed techniques can help both the dentist and the assistant work more comfortably. It is also important to be aware of the warning signs of MSDs and to seek medical intervention as early as possible. Regular exercises, frequent breaks during the day and assuming correct posture can increase efficiency and prolong the professional careers of the practitioners.
| References | |  |
| 1. | Hamann C, Werner RA, Franzblau A, Rodgers PA, Siew C, Gruninger S. Prevalence of carpal tunnel syndrome and median mononeuropathy among dentists. J Am Dent Assoc 2001;132:163-70. 
[PUBMED] |
| 2. | Miller DJ, Shugars DA. The health of the dental professional. J Am Dent Assoc 1987;114:515-8. 
|
| 3. | Lehto TU, Helenius HY, Alaranta HT. Musculoskeletal symptoms of dentists assessed by a multidisciplinary approach. Community Dent Oral Epidemiol 1991;19:38-44. 
[PUBMED] |
| 4. | Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. J Calif Dent Assoc 2002;30:139-48. 
[PUBMED] |
| 5. | Kerosuo E, Kerosuo H, Kanerva L. Self-reported health complaints among general dental practitioners, orthodontists, and office employees. Acta Odontol Scand 2000;58:207-12. 
[PUBMED] |
| 6. | Brown PN. What′s ailing us? Prevalence and type of long-term disabilities among an insured cohort of orthodontists. Am J Orthod Dentofacial Orthop 2004;125:3-7. 
[PUBMED] |
| 7. | Lalumandier JA, McPhee SD, Parrott CB, Vendemia M. Musculoskeletal pain: Prevalence, prevention, and differences among dental office personnel. Gen Dent 2001;49:160-6. 
|
| 8. | Szymamka J. Disorders of the musculoskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann Agric Environ Med 2002;9:169-73. 
|
| 9. | Rundcrantz BL. Pain and discomfort in the musculo-skeletal system in dentists. Swed Dent J 1991;76 (Suppl):101-2. 
|
| 10. | Oleske DM, Neelakantan J, Andersson GB, Hinrichs BG, Lavender SA, Morrissey MJ, et al. Factors affecting recovery from work-related, low back disorders in autoworkers. Arch Phys Med Rehabil 2004;85:1362-4. 
[PUBMED] |
| 11. | Krishnan SG, Hawkins RJ. Rotator cuff and impingement lesions in adult and adolescent athletes. In: DeLee JC, Drez D Jr, editors. DeLee and Drez′s orthopaedic sports medicine: Principles and practice. Philadelphia: Saunders; 2003. p. 1065-95. 
|
| 12. | Fish DR, Morris-Allen DM. Muscoloskeletal disorders in dentists. N Y State Dent J 1998;64:44-8. 
[PUBMED] |
| 13. | Bassett S. Back problems among dentists. J Can Dent Assoc 1983;49:251-6. 
[PUBMED] |
| 14. | Berkson M, Nachemson A, Schultz A. Mechanical properties of the human lumbar spine motion segment: II. Response in compression and shear. J Biomech Eng 1979;101:53-7. 
|
| 15. | Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: Strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc 2003;134:1604-12. 
[PUBMED] |
| 16. | Yamalik N. Musculoskeletal disorders (MSDs) and dental practice part-2- risk factors for dentistry, magnitude of the problem, prevention and dental ergonomics. Int Dent J 2007;57:45-54. 
[PUBMED] |
| 17. | Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U, Leggat P. Occupational health problems of dentists in Southern Thailand. Int Dent J 2000;50:36-40. 
|
| 18. | Diakow PR, Cassidy JD. Back pain in dentists. J Manipulative Physiol Ther 1984;7:85-8. 
[PUBMED] |
| 19. | Ratzon N, Yaros T, Mizlik A, Kanner T. Musculoskeletal symptoms among dentists in relation to work posture. Work 2000;15:153-8. 
|
| 20. | Hanney WJ, Zbaraschuk, Karis S , Cathy J , Klausner, Sheila H, Wawrzyniak, Loretta. Neck pain: Exercise and training consideration. Strength Cond J 2011;33:104-10. 
|
| 21. | Crisco J, Chelikani S, Brown R, Wolfe S. The effect of exercise on ligamentous stiffness in the wrist. J Hand Surg 1997;7:43-6. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
[Table 1]
|