|


 |
| CASE REPORT |
|
| Year : 2011 | Volume
: 3
| Issue : 1 | Page : 40-43 |
|
|
Traumatic fracture of thin pedicles secondary to extradural meningeal cyst
Daniel S Yanni, Antonios Mammis, Nikhil G Thaker, Ira M Goldstein
Department of Neurological Surgery, University of Medicine and Dentistry of New Jersey, Jersey Medical School, Newark, New Jersey, USA
| Date of Web Publication | 30-Mar-2011 |
Correspondence Address:
Ira M Goldstein
Department of Neurological Surgery, University of Medicine and Dentistry of New Jersey, 90 Bergen Street, Suite 8100 Newark, New Jersey 07103
USA
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.78472

 Abstract Abstract | | |
Spinal dural meningoceles and diverticula are meningeal cysts that have a myriad of clinical presentations and sequelae, secondary to local mass effect. Our objective is to report a technical case report, illustrating a traumatic spinal injury with multiple pedicle fractures, secondary to atrophic lumbar pedicles as well as the diagnostic workup and surgical management of this problem. Posterior lumbar decompression, resection of the meningeal cyst, ligation of the cyst ostium, instrumentation, and fusion were performed with the assistance of intraoperative isocentric fluoroscopy. The cyst's point of communication was successfully located with intraoperative fluoroscopy and the lesion was successfully excised. We suggest that patients with traumatic spinal injuries, having evidence of pre-existing anomalous bony architecture, undergo advanced imaging studies, to rule out intraspinal pathology. The positive clinical and radiographic results support the removal and closure of the pre-existing meningeal cyst at the time of treatment of traumatic spinal injury. Intraoperative isocentric fluoroscopy is a helpful tool in the operative management of these lesions. Keywords: Arachnoid cyst, Cerebrospinal fluid diverticula, extradural meningeal cyst, spinal meningeal cyst, thin pedicles
How to cite this article:
Yanni DS, Mammis A, Thaker NG, Goldstein IM. Traumatic fracture of thin pedicles secondary to extradural meningeal cyst. J Surg Tech Case Report 2011;3:40-3 |
How to cite this URL:
Yanni DS, Mammis A, Thaker NG, Goldstein IM. Traumatic fracture of thin pedicles secondary to extradural meningeal cyst. J Surg Tech Case Report [serial online] 2011 [cited 2016 Jun 12];3:40-3. Available from: http://www.jstcr.org/text.asp?2011/3/1/40/78472 |
 Introduction Introduction | |  |
Spinal dural meningoceles and diverticula have been previously classified by Tarlov, in 1970, and subsequently by Nabors, in 1988. This type of pathology has been referred to as arachnoid cysts, meningoceles, Cerebrospinal fluid (CSF) diverticula, and pseudomeningoceles. Nabors has classified these cysts as extradural meningeal cysts without nerve fibers (type I), also known as CSF diverticula. The extradural meningeal cysts with nerve fibers (type II) are described as spinal meningoceles. In contrast, type III spinal meningeal cysts are intradural arachnoid cysts. [1] For the sake of clarity, we will use Nabors classification to describe our findings.
These meningeal cysts are rare and may occur at all levels of the thecal sac. Although the origin of these meningeal cysts is thought to be congenital, some have postulated traumatic, iatrogenic, and inflammatory etiologies. [2],[3],[4] Cyst formation is believed to occur as arachnoid herniates through a defect in the dura. The mechanism of cyst expansion has been attributed to CSF pulsation, a ball-valve mechanism, osmosis, active fluid secretion, and hydrostatic forces. [2],[3],[4] The most common location of cyst ostia is the junction of the dural sleeve of the nerve root and thecal sac or dorsal midline.
The clinical presentation of the cysts may range from asymptomatic to pain, weakness, numbness, paresthesias, and paralysis. [5],[6],[7] Diagnostic evaluation of these cysts should include magnetic resonance imaging (MRI), myelography, or computed tomography (CT) myelography. [6] The MRI findings typically associated with meningeal cysts are the mass effect on the surrounding structures, hyperintense signal to the CSF on T2, partial enhancement with contrast, and possible signal void on the fast spin echo sequence (FSE). [8] Myelography or CT myelography may reveal communication with the cyst, in addition to compression of the surrounding structures, and may demonstrate the site of communication between the cyst and thecal sac. [7]
Treatment of these cysts consists of resection of the cyst and primary closure of the dural defect with a watertight closure. [4] As most cysts arise from the junction of the dural sac and the nerve root, a posterior approach via laminotomy / laminectomy may be used. [1],[7],[9],[10] A watertight closure consists of various combinations of dural repair with a nonabsorbable suture using a taper or reverse cutting needle, muscle or fat graft, fascial graft or dural substitute, and a fibrin sealant or dural sealant. [2],[3]
Although the mechanism for cyst expansion is not clear, it is believed to be the result of a physiological one-way valve mechanism. [1],[4],[7] In this manner, the cyst expands with any transient increase in intrathecal pressure due to systolic pulsation or valsalva maneuver; however, the unidirectional nature of the valve prevents decompression of the cyst. These hydrodynamic forces within the meningeal cyst can cause osseous changes in the spine including thinning of pedicles, erosion of the posterior and anterior elements, and widening of the neural foramen. [8] There have been no previous reports describing the tendency to fracture in thin pedicles secondary to spinal extradural meningeal cysts.
 Case Report Case Report | |  |
We present a case of a 20-year-old female who was an unrestrained back seat passenger in a motor vehicle collision. She denied any history of back pain, leg pain, weakness, numbness, or bowel / bladder dysfunction. She denied any history of prior surgeries. The patient presented to the ER with severe back pain and an inability to move her legs. Initial examination revealed bilateral lower extremity plegia, an L1 sensory level, and an absent rectal tone, indicating complete spinal injury. The CT scan revealed an L1 burst fracture with subluxation and bilateral pedicle fractures at L1 and L2 [Figure 1] and [Figure 2]. The patient was noted to have asymmetrically and atypically thin pedicles at these levels [Figure 2]. We suspected the presence of intraspinal pathology as the cause of the thin pedicles. Subsequent advanced imaging with MRI revealed the presence of an extradural meningeal cyst [Figure 1] and [Figure 2]. | Figure 1: (Left) sagittal T2 MRI showing fracture subluxation at L1 and the anterior displacement of the neural elements, arrow points to the dorsally located extradural meningeal cyst; (right) sagittal CT revealing the burst fracture with subluxation at L1
Click here to view |
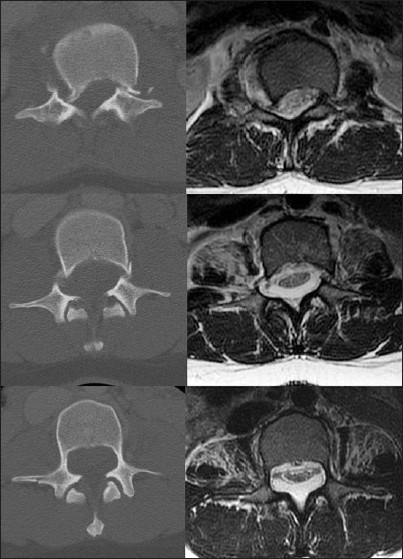 | Figure 2: (Top) axial CT and T2 MRI at the level of L1 showing bilateral pedicle fractures and subluxation associated with canal compromise. (Middle) axial CT and T2 MRI at the level of L2 showing bilateral pedicle fractures and a dorsally located extradural meningeal cyst. (Bottom) axial CT and T2 MRI at the level of L3 showing aberrantly thin pedicles, anterior displacement of the neural elements, and dorsally located extradural meningeal cyst
Click here to view |
Given the high suspicion of the multilevel intraspinal pathology, spinal canal compromise, coronal plane deformity, and sagittal plane deformity, a posterior approach was chosen, to address both decompression and stabilization. We performed a posterior thoracolumbar decompression, dissection of the cyst, identification of its communication with the dura, ligation of the ostium, repair of the dural defect, stabilization, and fusion. In the operating room, a midline approach was used to expose the T10 to L5. Laminectomies were performed at L1, L2, and L3. At this point the meningeal cyst was visualized and dissection was carried out around the cyst. To better define the point of communication, a diluted Omnipaque (GE Healthcare) was injected into the cyst in order to obtain an intraoperative myelogram. Isocentric fluoroscopy (Siemens Siremobile, Malvern, PA) was then used to obtain an intraoperative CT scan; this reconstructed CT myelogram / cystogram revealed communication with the thecal sac at the L3 level, laterally. Given the cyst origin, remote from the site of the spinal trauma and the presence of chronic osseous changes, it was concluded that the cyst was a pre-existing condition and not a result of the trauma. The meningeal cyst was resected and the ostium of the meningeal cyst was found in the axilla of the L3 nerve root near the thecal sac [Figure 3] and [Figure 4]. The ostium of the meningeal cyst was subsequently ligated using monofilament sutures and a primary dural repair was carried out using a local paraspinal muscle graft. This, in turn, was covered with a fibrin sealant. There was no spinal fluid leak visualized intraoperatively after valsalva. At this point, the L1 pedicle was resected and an offset bone impactor advanced ventral to the thecal sac to directly reduce the displaced L1 vertebra. Subsequently, posterior thoracolumbar instrumentation with polyaxial pedicle screws and rods were placed from T10 to L5, sparing the atretic pedicles of L1, L2, and the left L3. The nonstructural iliac crest bone graft using a marrow aspirate was added to the nonstructural allograft and local autograft, which were applied to the posterolateral fusion site. | Figure 3: Intraoperative photo showing an extradural meningeal cyst (double arrow) dissected away from the dura of the thecal sac (single arrow)
Click here to view |
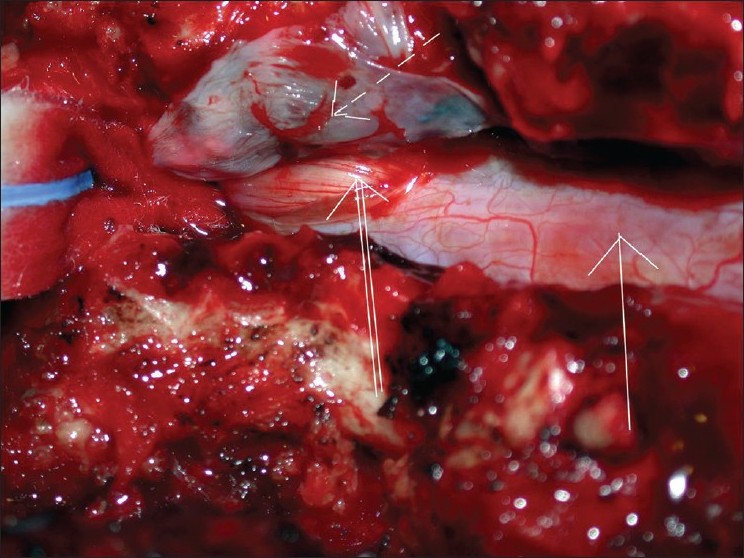 | Figure 4: Intraoperative photo showing the emptied extradural meningeal cyst resected (broken arrow) and cyst ostium (double arrow) of the thecal sac (single arrow) laterally
Click here to view |
This patient's postoperative management was routine for a patient with severe spinal injury. She was transferred to the floor following the recovery room. The incision healed without any complications or any spinal fluid-related issues. Radiographically, postoperative x-rays and a CT demonstrated excellent alignment and placement of pedicle screw instrumentation [Figure 5]. The patient was fitted with a Thoracolumbosacral orthosis (TLSO) brace on postoperative day 1. Rehabilitation was initiated on postoperative day 1. Over the course of a week, the patient's examination improved to American Spinal Injury Association (ASIA) C with antigravity strength at the iliopsoas. The patient continued to improve in rehabilitation over the following months. | Figure 5: Postoperative AP and lateral X-rays showing good alignment, reduction of the subluxation, and instrumentation
Click here to view |
 Discussion Discussion | |  |
Routine evaluation
Our routine workup for a patient with severe traumatic injury includes, a CT scan of the spine, often as a reconstruction of the abdominal scan obtained by the trauma service during the patient's early assessment, and CT imaging, which demonstrates bony injury without ligamentous or other soft tissue evaluation. A neurological deficit that is not explained by these bony findings then justifies an MRI or CT myelography. Typically, such studies would be expected to reveal the presence of traumatic disk herniation or an intraspinal hematoma. An occasional workup will reveal occult pathology, such as a benign tumor. As the use of CT imaging for the radiographic evaluation of severe trauma is increasingly the norm, deviant anatomy may be seen with increasing frequency. Such findings are generally not associated with a traumatic injury and do not influence the nature of the injury. When the bony anatomy is abberant, the presence of a longstanding mass lesion should be suspected. The pattern of the bony anomaly will often hint as to the location and nature of the lesion.
The information obtained will aid in both diagnosis and therapeutic management. From a diagnostic standpoint, patients with compromised pedicles or other supporting structures may have a greater magnitude of injury associated with a given trauma than expected. From a therapeutic standpoint, the presence of an intraspinal pathology may influence the approach and procedure used. In the case of an extradural meningeal cyst, a laminectomy will facilitate a further or at least a similar growth of this cyst, due to removal of the bony restriction inhibiting its growth. Treatment of the initial underlying pathology should be performed, particularly when the spinal injury sustained requires dorsal decompression.
Extradural meningeal cyst
This case depicts a previously asymptomatic patient with a large dorsal extradural meningeal cyst. The magnitude of the fracture and deformity associated with this trauma increased our suspicion for the presence of a chronic spinal pathology. Asymmetrically and aberrantly sized pedicles suggested a longstanding intraspinal process. Typical radiographic findings of chronic intraspinal mass lesions include scalloping of the vertebral body, thinning of the pedicles, erosion of the posterior and anterior elements, and widening of the neural foramen. [8] A preoperative MRI elucidated the presence of an extradural meningeal cyst and helped design the surgical treatment plan. Intraoperative CT myelography aided in the definitive identification and treatment of the cyst ostium.
In our extensive review of the literature for the association of trauma with intraspinal pathology, we found no documented cases of spinal fractures associated with pre-existing intradural or epidural cysts, tumors or other mass lesions.
We wish to demonstrate that patients who have intraspinal pathology may present with bony injuries, more comprehensive than otherwise expected. The appearance of anomalous bone morphology should make the attending physician suspicious of underlying chronic pathology. Advanced imaging studies to rule out benign tumors, congenital anomalies, CSF collections, or other pre-existing pathology should be obtained, as they may influence surgical management. Management may need to be modified with respect to the approach, instrumentation, and intraoperative imaging.
 Disclosure Disclosure | |  |
The authors do not report any conflict of interest concerning the materials or methods used in this study or the findings specified in this article.
 References References | |  |
| 1. | Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 1988;68:366-77. 
[PUBMED] [FULLTEXT] |
| 2. | Couture D, Branch CL Jr. Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus 2003;15:E6. 
|
| 3. | Hawk MW, Kim KD. Review of spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus 2000;9:e5. 
|
| 4. | Liu JK, Cole CD, Kan P, Schmidt MH. Spinal extradural arachnoid cysts: Clinical, radiological, and surgical features. Neurosurg Focus 2007;22:E6. 
|
| 5. | Fiss I, Danne M, Hartmann C, Brock M, Stendel R. Rapidly progressive paraplegia due to an extradural lumbar meningocele mimicking a cyst. Case report. J Neurosurg Spine 2007;7:75-9. 
[PUBMED] [FULLTEXT] |
| 6. | Krings T, Lukas R, Reul J, Spetzger U, Reinges MH, Gilsbach JM, et al. Diagnostic and therapeutic management of spinal arachnoid cysts. Acta Neurochir (Wien) 2001;143:227-34. 
[PUBMED] [FULLTEXT] |
| 7. | Marbacher S, Barth A, Arnold M, Seiler RW. Multiple spinal extradural meningeal cysts presenting as acute paraplegia. Case report and review of the literature. J Neurosurg Spine 2007;6:465-72. 
[PUBMED] [FULLTEXT] |
| 8. | Chen CJ, Ro LS. The MRI signs of spinal arachnoid diverticula. Neuroradiolog 1997;39:446-9. 
|
| 9. | Pyeritz RE, Fishman EK, Bernhardt BA, Siegelman SS. Dural ectasia is a common feature of the Marfan syndrome. Am J Hum Genet 1988;43:726-32. 
[PUBMED] [FULLTEXT] |
| 10. | Tei R, Morimoto T, Miyamoto K, Aketa S, Shimokawara T, Shin Y, et al. Dural repair for intraspinal extradural meningeal cyst. Neurol Med Chir (Tokyo) 2007;47:434-7. 
[PUBMED] [FULLTEXT] |
[Figure 1], [Figure 2], [Figure 3], [Figure 4], [Figure 5]
|