|


 |
| CASE REPORT |
|
| Year : 2011 | Volume
: 3
| Issue : 1 | Page : 44-48 |
|
|
Surgical and nonsurgical management of bilateral periapical lesions in the maxillary anterior region
Sweta Tolasaria, Utpal K Das
Department of Conservative Dentistry and Endodontics, Guru Nanak Institute of Dental Science and Research, Kolkata, India
| Date of Web Publication | 30-Mar-2011 |
Correspondence Address:
Sweta Tolasaria
Sun City Complex, Tower-A, Flat-502, 105/1, Bidhannagar Road, Ultadanga, Kolkata - 700 067
India
 Source of Support: None, Conflict of Interest: None
DOI: 10.4103/2006-8808.78473

 Abstract Abstract | | |
Conventional nonsurgical endodontic treatment has a high degree of clinical success, but in certain cases surgical intervention becomes necessary. This is the case report of a patient presenting with bilaterally separate periapical lesions in the maxillary anterior region. One lesion was managed by periapical surgery using a novel and safe method of separating the soft tissue mass of the periapical lesion which was in proximity to vital and vulnerable anatomical tissues, and the other was managed by long-term intracanal medicament, emphasizing the need of application of treatment in the best interest of the patient. Keywords: Bilateral periapical lesions, intracanal medicament, periapical surgery
How to cite this article:
Tolasaria S, Das UK. Surgical and nonsurgical management of bilateral periapical lesions in the maxillary anterior region. J Surg Tech Case Report 2011;3:44-8 |
How to cite this URL:
Tolasaria S, Das UK. Surgical and nonsurgical management of bilateral periapical lesions in the maxillary anterior region. J Surg Tech Case Report [serial online] 2011 [cited 2016 Jun 12];3:44-8. Available from: http://www.jstcr.org/text.asp?2011/3/1/44/78473 |
 Introduction Introduction | |  |
In modern endodontic practice, the number of indications for endodontic periapical surgery is decreasing. Still periapical surgery accounts for 3% to 10% of typical endodontic practice. [1] This case report has been presented to emphasize that all nonvital teeth with periapical lesion should be first treated conservatively, and the treatment mode is to be changed to surgical therapy only when conventional treatment proves ineffective. Oztan and Kalaskar et al. have confirmed that large periapical lesions can respond favorably to nonsurgical treatment using calcium hydroxide paste. [2],[3] Cohn proposed periapical surgery as a predictable option when root canal treatment is either not possible or fails. [4] Thus surgical endodontic treatment is indicated in limited number of cases of persistent periradicular pathosis. Selection between alternative treatments should be based on assessment of individual case, as done in the present case report.
A meticulous removal of periapical granulation tissue is an important aspect of surgical endodontic treatment. Removal of very large anterior cysts in maxilla may produce oro-nasal communication in cases wherein the cyst has destroyed the bony floor of the nasal cavity, with only soft tissue lining left in between. [5],[6] An innovative method of surgical removal of the periapical lesion to save teeth with periapical pathosis refractory to conventional treatment and to preserve the adjacent vital structures has been introduced.
The present case report shows the management of bilateral maxillary pathosis. The large "through and through" periapical pathosis with both buccal and palatal bone loss is managed by periapical surgery adopting a novel method of separation of lesion after nonresponsiveness of the pathosis to intracanal medicament and of the smaller periapical pathosis to long-term intracanal medicament. To the best of our knowledge, such a case has not been reported previously in the literature.
 Case Report Case Report | |  |
A 19-year-old female patient was referred to the Department of Conservative Dentistry and Endodontics with the chief complaint of pain and recurrent swelling in the upper front teeth region since 10 to 12 weeks. Medical history and investigations did not reveal anything that could oppose or influence the proposed treatment plan. The patient gave a history of trauma to the teeth 10 years back. On clinical examination, labial and palatal swelling was seen in association with maxillary right central incisor (tooth no. 11), lateral incisor (12) and canine (13). A discharging periapical sinus was seen apically between the roots of teeth nos. 12 and 13. Maxillary right and left central incisors (tooth no 11 and 21) were discolored and fractured. Teeth nos. 11, 12, 13 and 21 were tender to percussion. Periodontal examination revealed sulcus depths within normal limits. Teeth nos. 11, 12, 13 and 21 gave a negative response with the electrical pulp tester (Digitest, Farmingdale, NY). The maxillary occlusal radiograph showed a large radiolucent periapical lesion in association with maxillary right anterior teeth and a relatively small radiolucent periapical lesion in association with maxillary left anterior tooth [Figure 1].
Based on the history, clinical examination, sensitivity test and radiographic examination, a diagnosis of pulp necrosis with symptomatic periapical pathosis was made for the right maxillary central incisor, lateral incisor and canine. Same was the diagnosis for the left maxillary central incisor. A decision of conventional root canal treatment with the placement of intracanal medicament was made after discussion with the patient. The patient consented to the treatment plan.
The operative field was isolated, and access preparation was done in 11, 12, 13 and 21 without local anesthesia. After the radiographic determination of the working length, biomechanical preparation following 'step back' method was done using 2.6% sodium hypochlorite and normal saline as an irrigating agent. Iodine containing calcium hydroxide (Vitapex, Neo Dental Chemical Products, Tokyo, Japan) was placed as intracanal medicament, and the root canal access was sealed with zinc oxide eugenol cement at the end of the first appointment. After 21 days, the patient reported with no relief from her symptoms. There was no resolution of the buccal-palatal swelling, and tenderness to percussion continued to be present in 11, 12 and 13; but tooth 21 became asymptomatic.
Decision was changed in favor of periapical surgery on the right maxillary anterior region. The plan for long-term intracanal medicament on tooth 21 was continued. Revised consent was obtained from the patient prior to the surgical treatment. Teeth 11, 12 and 13 were obturated with zinc oxide eugenol sealer and gutta-percha using the lateral condensation technique.
Assessment of the surgical site showed adequate mouth opening, little attached gingiva and adequate depth of the vestibule. Local anesthesia of 2% lignocaine with 1:80,000 adrenaline was infiltrated in the alveolar buccal mucosa superficial to the periosteum at the level of root apices from 13 to 21 to get added advantage of less surgical bleeding. Nasopalatine nerves were also anesthetized by infiltration in the incisive foramen. The buccal full-thickness triangular mucoperiosteal flap was elevated to expose the area of periapical lesion. Already existing pathological cortical bone window was expanded until underlying pathology was adequately exposed and sufficient space was available for thorough curettage.
Sterilized gauze was placed between the pathological soft tissue mass and the lateral wall of the crypt, and lateral pressure was applied on the gauze with the concave surface of the curette facing the bone. This helped in separation of the periapical lesion from the surrounding bone and the nasal mucosal and palatal linings [Figure 2]. The dental assistant supported the palatal lining from inside the oral cavity with his finger while the cystic lining was being separated from the palatal lining. The periodontal curette was used to remove the tissue firmly attached to the root surface [Figure 3]. Caution was exercised in separating the lesion from the roof because no intervening bone was present between the nasal lining and the lesion. However, the lesion was curetted in toto, leaving the nasal and the palatal linings intact. The nasal lining could be seen moving with inhalation and exhalation.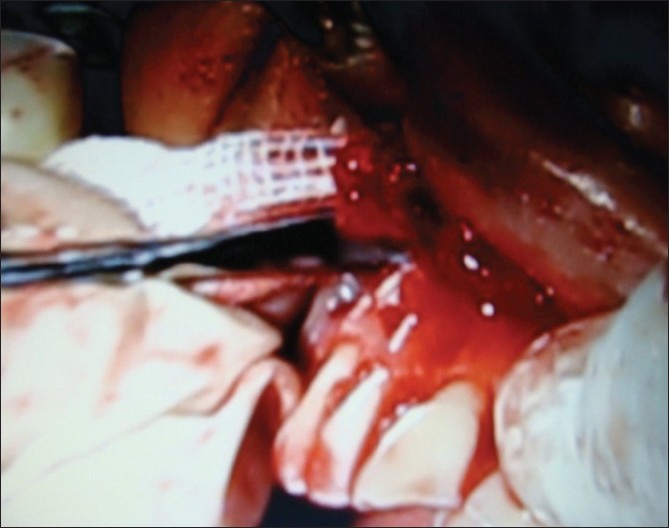 | Figure 2: Sterilized gauze placed between the soft tissue mass and the lateral wall of the crypt from the distal aspect with the curette
Click here to view |
 | Figure 3: After separation of the periapical lesion from the surrounding bone and the nasal and palatal linings but attached to the root surface
Click here to view |
The enucleated periapical lesion was stored in 10% buffered formalin solution and sent for histopathological examination. The root resection was not done to maintain maximum cemental covering on the root surface and to maintain the original root length to help tooth stability. Gutta-percha at the exposed root apex was burnished. The bone cavity was irrigated with sterile normal saline and gently dried with moist gauze. Careful clinical and radiographic inspection of the area was done to ensure no residual lesion tissue was left behind. The flap was repositioned and the flap margins were ensured to rest on sound bone. The flap was sutured using 5-0 silk with interrupted sutures.
The patient was given postoperative instructions both verbally and in writing. Antibiotics, analgesics and mouthwash were prescribed. On the 4 th postoperative day, healing of covering mucosa with primary intention was observed and the sutures were removed. Histopathological report diagnosed the lesion as radicular cyst.
The patient was free from all symptoms and signs with optimum tissue healing at the 6-month follow-up visit. Radiographic examination revealed decrease in the size of periapical radiolucency bilaterally. Tooth 21 was obturated with zinc oxide eugenol sealer and gutta-percha using lateral condensation technique. Esthetic rehabilitation of 11 and 21 was done. A radiographic review at the 1½-year follow-up showed good evidence of bone healing bilaterally [Figure 4].
 Discussion Discussion | |  |
Conservative approach of treatment of any lesion is always preferable over surgery as most periapical lesions are the result of an inflammatory response to bacterial infection within the root canal, i.e., intracanal infection. Nonsurgical root canal treatment involves cleaning and disinfecting the root canal system, thereby reducing the bacterial load and creating an environment in which periapical healing can occur. This has limited periapical surgery in contemporary dental practice to very selective cases - those in which the causative factors are located outside the root canal, such as microorganisms colonizing the periapical tissues, cysts and foreign body reactions. [7] To prevent tooth loss, surgical solution for the inflammatory periapical lesions was considered in the present case as right maxillary anterior region did not respond favorably to conservative treatment.
Here we have reported a case of bilateral large periapical lesions. Nonsurgical root canal treatment using calcium hydroxide as intracanal medication was attempted on both sides, emphasizing conservative treatment, expecting that the long-term intracanal medicament will be effective in resolving the periapical lesions. Follow-up after 21 days revealed, left tooth was asymptomatic but the teeth in the right region were symptomatic. Treatment for the right side was changed to surgical intervention according to the clinical need.
Calcium hydroxide intracanal medicament can facilitate periapical healing in nonvital teeth with periapical lesion. [8] Intracanal medicaments are advocated to eliminate remaining bacteria after chemomechanical instrumentation, even in the inaccessible areas of the root canal system, reduces inflammation of the periapical tissues, dissolves remaining organic material and counteracts coronal microleakage. [9] In the case presented here, calcium hydroxide intracanal medicament created a more favorable environment leading to healing of periapical lesion in the left central incisor. The periapical lesion on the right side, however, did not respond to the intracanal medicament because of the causative factor being located beyond the root canal system, viz., within the inflamed periapical tissue, thus requiring surgical intervention. [10],[11]
Conventional method of removing soft tissue from the bony crypt consists of using curettes. Curettes are initially used with the concave surface facing the internal wall of the osseous crypt to separate the soft tissue lesion from the lateral borders of the crypt and subsequently used in a scraping manner to remove the remainder of the lesion from the osseous defects. [1],[7] Curette being sharp margined, there always remains a risk of penetration of the vital anatomic structures or pathological soft tissue mass, which will make the removal of the tissue mass difficult and time consuming.
The surgical technique is a fundamental consideration, since it largely conditions the prognosis of periapical surgery. [12] A novel method of separation of lesion was adopted in this case with large periapical lesion to prevent injury to other surrounding vital anatomic structures. Caution was required in separating the lesion from the roof because no intervening bone was present between the nasal lining and the lesion. Application of gentle lateral pressure on the sterilized gauze placed between the pathological soft tissue mass and the lateral wall of the crypt with the concave surface of the curette facing the bone to free the soft tissue in the present case helped in the removal of the entire tissue mass without injuring the nasal mucosa and palatal lining. The lesion too was curetted in toto.
The present method has the advantage of more predictable removal of the soft tissue lesion in toto because of the blunt technique used, compared to using sharp curettes with higher chances of penetration of the soft tissue lesion making the removal of the remaining tissue tags difficult and more time consuming. At the same time, the present method results in greater safety of the approximating vital and vulnerable anatomical tissues, resulting in better postoperative comfort and outcome for the patient.
At the 6-month and 1½-year postoperative recall examination, the teeth were asymptomatic and radiographically showed signs of healing of periapical lesions. Evaluating success of the periapical surgery based on clinical and radiographic criteria of von Arx and Kurt, the surgery can be considered to be successful. [13],[14]
 Conclusion Conclusion | |  |
It can be concluded that endodontic treatment with calcium hydroxide as intracanal medicament might be a viable approach for promoting periapical healing and success in root canal treatment in nonvital teeth associated with periapical lesion. However, periapical surgery may be the only alternative when the tooth with periapical lesion fails to respond to calcium hydroxide as intracanal medicament. To prevent injury to other vital anatomic structures, a novel method of surgically treating large periapical lesions has also been introduced in the present case report.
 References References | |  |
| 1. | Johnson BR, Witherspoon DE. Periradicular Surgery. In: Cohen S, Hargreaves KM, editors. Pathways of the Pulp. 9th ed. Missouri: Mosby; 2006. p. 724-85. 
|
| 2. | D. Öztan. Endodontic treatment of teeth associated with a large periapical lesion. Int Endod J 2002;35:73-8. 
|
| 3. | Kalaskar R. Tiku A, Damle SG. Periapical repair and apical closure of a pulpless tooth using calcium hydroxide - A case report. J Indian Soc Ped Prev Dent 2004;22:158-61. 
|
| 4. | Cohn SA. When all else fails. Aust Endod J 1998;24:128-9. 
|
| 5. | Kapoor V. Textbook of Oral and Maxillofacial Surgery. 1 st ed. New Delhi: Arya Pulishing House; 2001. 
|
| 6. | Verghese GM, George T, Kuttappa MA, Girish KG. Management of a large periapical cyst (apical matrix and surgical complications) - A case report. Endodontology 2009;84-89. 
|
| 7. | Morrow SG, Rubinstein RA. Endodontic Surgery. In: Ingle JI, Bakland LK, editors. Endodontics. 5 th ed. Hamilton:BC Decker Inc; 2003. p. 405-570. 
|
| 8. | Gutmann JL, Fava LR. Periradicular healing and apical closure of a non-vital tooth in the presence of bacterial contamination. Int Endod J 1992;25:307-11. 
|
| 9. | Tronstad L. Clinical Endodontics A Textbook. 2 nd ed. Germany: Gulde Druck; 2003. 
|
| 10. | Nair PN. Biology and pathology of apical periodontitis. In: Estrela C, editors. Endodontic Sciences. 2 nd ed. Brazil: Artes Medicas; 2009. p. 285-348. 
|
| 11. | Nair PN. Review: New perspectives on radicular cysts: Do they heal? Int Endod J 1998;31:155. 
|
| 12. | Rahbaran S, Gilthorpe MS, Harrison SD, Gulabivala K. Comparison of clinical outcome of periapical surgery on endodontic and oral surgery unit of a teaching dental hospital. A retrospective study. Oral Surg Oral Med Oral Pathol 2001;91:700-9. 
|
| 13. | Von Arx T, Kurt B, Ilgenstein B, Hardt N. Preliminary results and analysis of a new set of sonic instruments for root-end cavity preparation. Int Endod J 1998;31:32-8. 
|
| 14. | Von Arx T, Kurt B. Root-end cavity preparation after apicoectomy using a new type of sonic and diamond-surfaced retrotip: A 1-year followup study. J Oral Maxillofac Surg 1999;57:656-61. 
|
[Figure 1], [Figure 2], [Figure 3], [Figure 4]
|